The liver is the second most damaged organ in abdominal trauma. The purpose of this article is to present the experience of our regional reference hospital and summarise the management of these types of injury over the last four years.
Patients and methodsAn observational, descriptive and retrospective study was performed on patients with hepatic trauma admitted to our Department from January 2006 to March 2010. The clinical variables collected were: age, sex, aetiology, injury type, presence of haemodynamic stability and peritonism, type of treatment, and complications.
ResultsThe study included 17 patients, with a mean age of 25.3 years, and 12 of them were male. Ten patients received non-surgical treatment. Of those who received surgical treatment, packing was performed on 3, with one of them requiring a hemi-hepatectomy in a second operation. There were complications in 4 patients, 2 surgical and 2 non-surgical.
Discussion and conclusionsThe most important criterion for the choice of non-surgical treatment is haemodynamic stability. The most recommended surgical technique for the rapid control of liver bleeding is compression packing, achieving stabilisation and to transfer the patient to a hospital with experience in hepatic surgery.
El hígado es el segundo órgano más dañado en los traumatismos abdominales. El objetivo de este trabajo es presentar la experiencia de nuestro hospital de referencia regional y resumir el manejo de este tipo de lesiones a lo largo de los cuatro últimos años.
Pacientes y métodosSe realiza un estudio observacional, descriptivo y retrospectivo de los traumatismos hepáticos ingresados en nuestro Servicio desde enero de 2006 hasta marzo de 2010. Se recogen diferentes datos clínicos (edad, sexo, etiología, tipo de lesión, presencia de estabilidad hemodinámica y peritonismo, tipo de tratamiento y complicaciones).
ResultadosDiecisiete pacientes son incluidos, con una edad media de 25,3 años, 12 de ellos son varones. Diez pacientes reciben tratamiento no quirúrgico. De los intervenidos, en 3 se realiza un packing y, 1 de estos requiere una hemihepatectomía en la segunda intervención. Aparecen complicaciones en 4 pacientes, 2 operados y 2 no operados.
Discusión y conclusionesEl criterio más importante para la elección del tratamiento no quirúrgico es la estabilidad hemodinámica. La técnica quirúrgica más recomendada para el control rápido de la hemorragia hepática es el packing, permitiendo estabilizar y derivar al paciente a un hospital con experiencia en cirugía hepática.
After the spleen, the liver is the most frequently injured organ following blunt abdominal or thoracic trauma. It is the most damaged in open or penetrating trauma.1,2
The evolution in the diagnostic and therapeutic management of liver trauma (LT) in recent years has led to a decline in mortality, which is currently between 4% and 15% depending on the type of injury and the presence or absence of other affected organs.2 This decrease is attributed by some authors to improved surgical techniques in managing injuries to major vessels and bile ducts, the use of damage control principles, the use of angiography, embolisation and the shrinking number of LT operations.3,4
Currently, treatment of LT tends to be increasingly conservative, with surgery performed in specific cases. This study is intended to present the experience of the Extremadura referral hospital over the last 4 years and summarise the management of this condition.
Patients and MethodsAn observational, descriptive, cross-sectional and retrospective study was performed. All cases of LT admitted from January 2006 to March 2010 in the Hepatobiliary and Pancreatic Surgery and Transplant Department of the Hospital Infanta Cristina, Badajoz (Spain), were reviewed. This is the referral centre for treatment of this disease for the region of Extremadura.
The following information was collected from the medical records reviewed: age, sex, aetiology, hospital stay, type of trauma according to the Liver Injury Scale (LIS)—see Table 1—the presence of peritonitis or haemodynamic instability (HI) upon admission, the need for transfusion and surgery and the presence of complications. The Student's t-test was used to compare means. Tests were also conducted for normality (runs), randomness (Kolmogorov–Smirnov) and homoscedasticity (Levene). The chi-square and Fisher's exact tests were used to establish the relationship between qualitative variables.
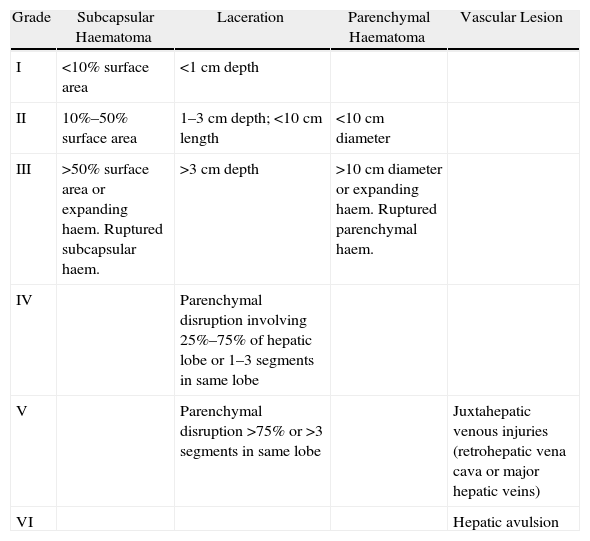
Classification of Liver Trauma According to the Liver Injury Scale.
| Grade | Subcapsular Haematoma | Laceration | Parenchymal Haematoma | Vascular Lesion |
| I | <10% surface area | <1cm depth | ||
| II | 10%–50% surface area | 1–3cm depth; <10cm length | <10cm diameter | |
| III | >50% surface area or expanding haem. Ruptured subcapsular haem. | >3cm depth | >10cm diameter or expanding haem. Ruptured parenchymal haem. | |
| IV | Parenchymal disruption involving 25%–75% of hepatic lobe or 1–3 segments in same lobe | |||
| V | Parenchymal disruption >75% or >3 segments in same lobe | Juxtahepatic venous injuries (retrohepatic vena cava or major hepatic veins) | ||
| VI | Hepatic avulsion |
During the study period, 17 patients with LT were admitted: 12 men and 5 women. The age was from 14 to 44 years (mean 25.3±9). Hospital stay varied from 4 to 37 days (mean 17.29±8.93).
Only 1 of the injuries was penetrating, due to an accidental shooting with a firearm. Of the closed LT, 8 were for car or motorcycle accidents, 2 for a bicycle fall, 2 for a kick from a horse and the others due to the impact of blunt objects. Among them, 2 patients had signs of peritoneal irritation and 3 were haemodynamically unstable at admission, 9 required a transfusion and 7 needed surgery. All transfusion cases were performed with packed red blood cells (from 2 to 14 units), 3 of them had plasma (4 to 8 units), 3 had platelets (2 to 5 units) and 2 had clotting factors.
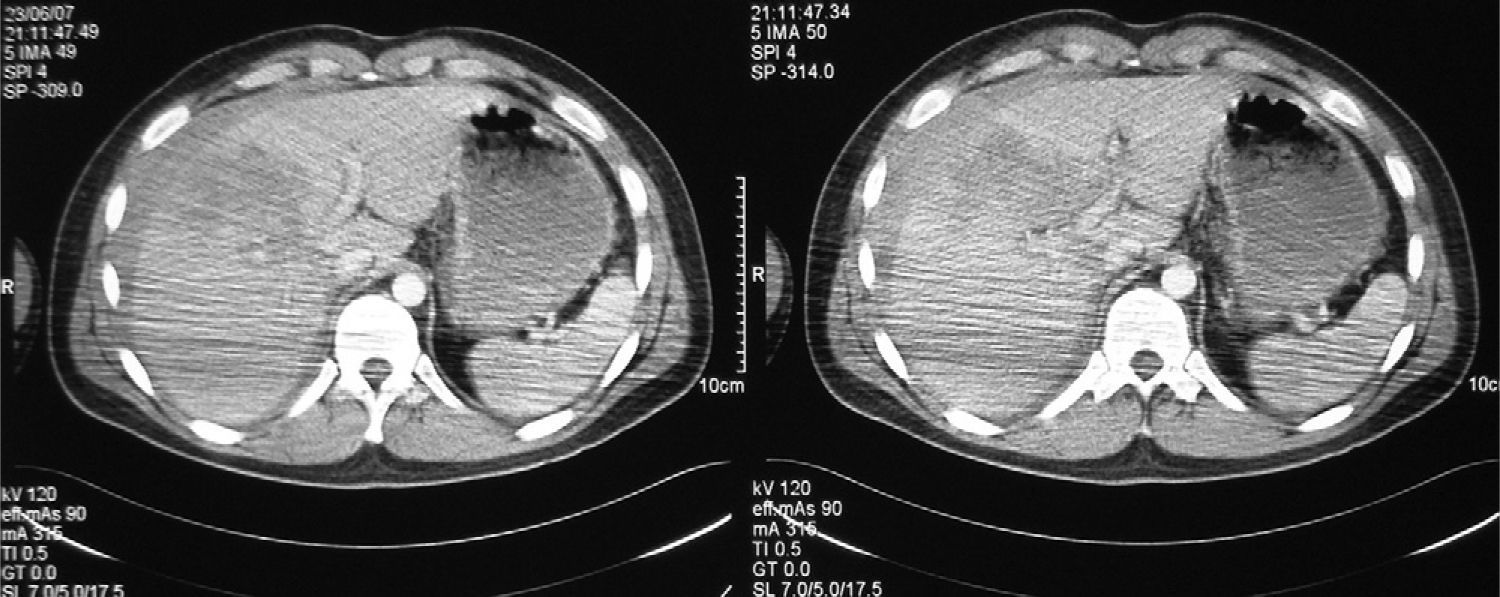
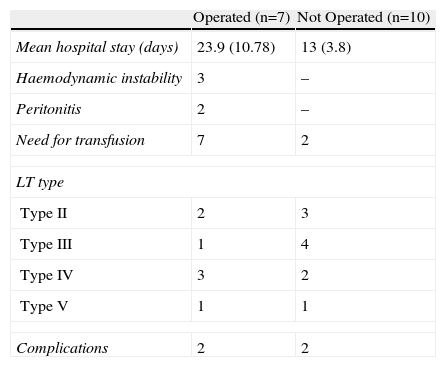
Computed tomography (CT) was used as the diagnostic radiology test for all LT, and ultrasound was used in 7 of them. According to the LIS classification, 5 patients suffered from type II LT, 4 from type III, 5 from type IV, and 2 from type V (Figs. 1 and 2). Table 2 compares the group of patients undergoing surgery with those not operated upon.
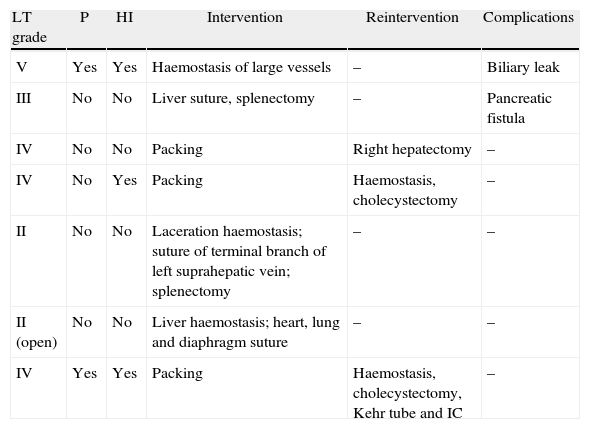
Of the 7 patients who underwent surgery, 3 required reinterventions as the first surgery was for a perihepatic packing, all due to grade IV LT. Another 2 of the surgery cases required a splenectomy, and 1 a cholecystectomy. In the reoperations, 1 patient underwent a right hepatectomy, 2 underwent cholecystectomy, and 1 of these also a choledochotomy to insert a Kehr tube for a small leak in segment VII (Table 3).
Patients Undergoing Surgery.
| LT grade | P | HI | Intervention | Reintervention | Complications |
| V | Yes | Yes | Haemostasis of large vessels | – | Biliary leak |
| III | No | No | Liver suture, splenectomy | – | Pancreatic fistula |
| IV | No | No | Packing | Right hepatectomy | – |
| IV | No | Yes | Packing | Haemostasis, cholecystectomy | – |
| II | No | No | Laceration haemostasis; suture of terminal branch of left suprahepatic vein; splenectomy | – | – |
| II (open) | No | No | Liver haemostasis; heart, lung and diaphragm suture | – | – |
| IV | Yes | Yes | Packing | Haemostasis, cholecystectomy, Kehr tube and IC | – |
HI: haemodynamic instability; IC: intraoperative cholangiography; LT: liver trauma; P: peritonitis.
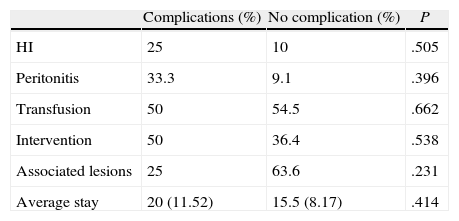
Two patients had complications while undergoing surgery: a bile leak in a grade V LT patient, which required an endoscopic sphincterotomy and biliary prosthesis placement; and a grade III LT case required a pancreatic low-flow fistula due to spontaneous closure. As for non-surgically treated (NST) patients, a biloma appeared in segment IV in 1 case with a grade II LT, and 1 patient with grade IV LT developed abdominal pain 3 weeks after discharge; both improved with treatment. No statistical relationship was found between complications and other variables, such as hospital stay, LT aetiology, the presence of peritonitis or haemodynamic stability, LT grade, or the need for surgery or transfusion. A statistically significant relationship was found between the need for surgery and a longer hospital stay, as well as a higher percentage of transfusion patients appearing among those undergoing surgery than in those not operated upon (Table 4).
Statistics for Complications and the Need for Surgical Intervention.
| Complications (%) | No complication (%) | P | |
| HI | 25 | 10 | .505 |
| Peritonitis | 33.3 | 9.1 | .396 |
| Transfusion | 50 | 54.5 | .662 |
| Intervention | 50 | 36.4 | .538 |
| Associated lesions | 25 | 63.6 | .231 |
| Average stay | 20 (11.52) | 15.5 (8.17) | .414 |
| Operated (%) | Not operated (%) | P | |
| HI | 40 | 0 | .09 |
| Peritonitis | 33.3 | 0 | .125 |
| Transfusion | 100 | 20 | .002 |
| Intervention | 33.3 | 50 | .538 |
| Associated lesions | 57.1 | 60 | .646 |
| Average stay | 23.43 (10.78) | 13 (3.8) | .044 |
HI: haemodynamic instability.
Radiographic improvement was observed in all hepatic lesions during follow-up after discharge.
DiscussionThe most common cause of LT is road traffic accidents (67% of cases).2 In our cohort, 47% was for this cause, and 29% due to impact with a blunt object. Severe LT accounts for 10%–30% of all liver injuries and 40%–80% of mortality.1 In our study, 7 patients suffered severe LT (grades IV and V) without any cases of death.
For the diagnosis of LT, CT is the most sensitive and specific test to determine the extent and severity of injuries.2,5 However, it has a 13% false negative rate for associated intestinal perforation. Ultrasound is the radiological technique of choice when the patient is unstable, as it allows rapid detection of the haemoperitoneum with a sensitivity of 83.3% and a specificity of 99.7%. Both tests have replaced diagnostic peritoneal lavage.3 The CT scan for all our patients was diagnostic, with 7 of them undergoing a prior ultrasound before referral to our hospital. Some authors have attempted to establish an increase in serum transaminase as a liver injury marker in stable patients with abdominal trauma to predict who may need a CT to study the LT.6
NST in adults is as a result of the experience with LT and spleen trauma in children. The natural development of much LT towards spontaneous haemostasis, along with the high regenerative capacity of the liver, means that this can often heal without surgery. The most important variables considered for indication of NST in LT patients are: haemodynamic stability (systolic blood pressure >90mm Hg, heart rate <100 beats per minute, normal base excess and lactate levels in serum), neurological integrity, the absence of signs of peritoneal irritation, no transfusion requirements, the degree of LT (according to the LIS scale), aetiology of the injury, the availability of an Intensive Care Unit (ICU), the amount of haemoperitoneum, the absence of other associated internal abdominal injuries and a history of anticoagulant therapy.2,3,7 The most important of all these variables is haemodynamic stability upon arrival at the Emergency Department or after initial resuscitation (up to 2l of fluid) and the absence of peritoneal irritation.1,8,9
In stable patients, the estimated success rate for LT grades I and II is 91.5%, 79% for grade III, 61%–86% for grade IV and 32%–77% for grade V. However, it is impossible to predict which patients will not respond to the initial NST. NST mortality for LT is less than for surgical treatment (4%).2,9,10
The advantages of NST are mainly due to decreasing the risk from laparotomy, in both the short term (due to anaesthetic or iatrogenic complications, abdominal infections, lower transfusion requirements, shorter hospital and ICU stay) and the long-term (risk of bowel obstruction or hernia due to scarring). However, NST poses a risk of delayed bleeding or complications from a perforated hollow viscus not detected by CT (this occurred in 0.3% of patients in a blunt trauma study of 225000 cases). According to some authors,3,9 leaving blood in the abdominal cavity can cause adhesions with the associated risk of intestinal obstruction. They therefore propose a laparoscopy to clean the interior of the abdomen a week after the trauma.
Numerous studies have shown the usefulness of arteriography with embolisation in the treatment of LT, with a success rate of up to 91%. The benefits of this technique are a shorter hospital stay and less need for transfusions and surgical intervention.5 No interventional radiology was used for managing LT in our cohort. However, it was useful for managing patients with non-traumatic bleeding lesions, which is not discussed in this study.
All LT patients with haemodynamic shock resistant to fluid therapy and whose abdominal ultrasound shows free fluid in the upper right quadrant need emergency abdominal surgery.2 The main criteria for indicating surgical treatment are haemodynamic instability and the need for transfusion.1 However, if a stable patient under observation becomes unstable or has peritoneal irritation, surgery is required.9 When a LT patient initially undergoing NST requires surgical treatment, it is more difficult because of the procedure and the instability of the patient.3
In general, the most recommended incision for LT surgical treatment is supra and infra-umbilical midline laparotomy, because it allows for the examination of the abdomen. However, hepatobiliary surgeons prefer the bilateral subcostal to the Rio Branco incision, as it offers better exposure to the right hepatic lobe, suprahepatic veins, and vena cava. Perihepatic packing contains over 80% of the LT profuse bleeding requiring a laparotomy, and allows for intraoperative resuscitation. This is the procedure that less experienced surgeons are usually recommended for controlling and stabilising a patient before being sent to the referral hospital.2,4 In our series, of the 7 patients requiring a laparotomy, perihepatic packing was performed in only 3 of them, as this was performed in other area hospitals to stabilise the patients before subsequent transfer to our hospital. The Pringle manoeuvre was performed in another LT patient, being partially haemostatic. Of reoperated patients, only 1 required a right hemihepatectomy after packing, while in the other 2 cases a cholecystectomy was performed, with 1 of them having a Kehr tube inserted for a small leak detected by intraoperative cholangiography.
In the experience of some authors, almost half of penetrating stab wounds in the anterior abdominal wall and 86% in the posterior wall can be managed with NST. However, this is more controversial with isolated LT caused by a gunshot wound. The high sensitivity and specificity of CT to rule out hollow viscus perforation, and embolisation by arteriography in cases of contrast leakage, may allow a NST with increased safety for penetrating LT.2 Only 1 of our patients had a penetrating LT caused by a gunshot with associated intrathoracic injuries (Table 3).
The complications rate is 5%–42% for NST and is related to the degree of LT. Thus, for grade V LT it is 63%, 21% for grade IV, 1% for grade III, and 0% for the other morbidities. The most frequent is bleeding (2.8%–8.4%), biliary leak, abdominal compartment syndrome (1%), liver necrosis, liver abscess, and injuries to other organs (1%–5%). Late bleeding is the leading cause of death in LT, which usually occurs within 72hours after starting NST (and especially in the first 24hours). Biliary complications (0.5%–4.5%) usually occur after the third day following LT. If these are not resolved by percutaneous drainage, a biliary stent can be inserted with help from an endoscopic retrograde cholangiopancreatography.11 Of the 4 complications in our cohort, there were 2 secondary to a bile duct injury, 1 due to biloma and another one due to bile leak, with the latter requiring a prosthesis to be inserted. The lack of statistical significance between complications or the need for surgical intervention with the other variables analysed may be due to the limited sample size.
Other areas where there are still no agreed standards for managing LT are ICU or hospital stay, LT follow-up protocol, and the time for the patient to rest before returning to a normal life. Recommendations include performing regular control CT scans, according to the patient clinical status, from the first month. Significant physical activity should not be attempted until at least 90%–95% of the initial injury has healed, according to the CT.2,9
ConclusionsThe most important criterion for choosing NST is haemodynamic stability. If there is clinical deterioration or signs of peritonitis, a laparotomy is recommended. Perihepatic packing is the most recommended technique for damage control surgery, especially in hospitals with less experience in liver surgery and multiple trauma, as it provides rapid stabilisation before transferring the patient to a referral hospital.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please, cite this article as: Ayuso Velasco R, et al. Manejo del traumatismo hepático: cuatro años de experiencia. Cir Esp. 2011;89:511–6