The purpose of this work is to present 8 minilaparoscopic-assisted transvaginal appendectomies using rigid instruments in patients with acute appendicitis.
Material and methodsEight minilaparoscopic-assisted transvaginal appendectomies were performed from the 10th of August 2009 to the 30th of June 2010. The inclusion criteria were women between 18 and 65 years of age with a diagnosis of acute appendicitis. The exclusion criteria were palpable masses, appendicular abscesses, ASA III and IV; morbid obesity (BMI>35); gynaecological infections; virgin patients and pregnant women. The surgical intervention was performed with rigid instruments. Surgical time, the need for post-operative analgesics, and post-surgical complications.
ResultsThe age range varied between 18 and 42 years, with a mean of 29.6 years. The mean surgical time was 48.3min (37–75min). Analgesics were given to 2 patients after surgery (1 parenteral and 1 oral). Five patients were discharged before 24h and 3 at 48h. There were no post-operative complications.
ConclusionsMinilaparoscopic-assisted transvaginal appendectomy with rigid instruments, in selected women is a feasible and safe method, and with better aesthetic results than laparoscopic appendectomy, but future studies will be required that can demonstrate its advantages.
Reportar 8 apendicectomías transvaginales asistidas por minilaparoscopia en pacientes con apendicitis aguda, con el empleo de instrumentos rígidos.
Material y métodosDesde el 10 de agosto del 2009 al 30 de junio del 2010, fueron realizadas 8 apendicetomías transvaginales asistidas por minilaparoscopia. Criterios de inclusión: mujeres entre 18 y 65 años de edad con diagnóstico de apendicitis aguda. Criterios de exclusión: Masas palpables; abscesos apendiculares; Asa III y IV; obesidad mórbida (IMC>35); infecciones ginecológicas; pacientes vírgenes y gestantes. Las intervenciones quirúrgicas fueron realizadas con instrumentos rígidos. Se estudió el tiempo quirúrgico; necesidad de analgésicos en el postoperatorio y complicaciones postoperatorias.
ResultadosEl rango de edad fluctuó entre los 18 y 42 años con una media de 29.6 años. El tiempo quirúrgico medio fue de 48,3min (37-75). En el postoperatorio se administraron analgésicos a 2 pacientes (1 parenteral y 1 oral). El alta hospitalaria se dio a 5 pacientes antes de las 24 horas y en 3 a las 48 horas. No se presentaron complicaciones postoperatorias.
ConclusionesLa apendicectomía transvaginal asistida por minilaparoscopia con el empleo de instrumentos rígidos, en mujeres seleccionadas, es un método factible, seguro y con mejores resultados estéticos que la apendicectomía laparoscópica, pero serán necesarios estudios futuros que demuestren sus ventajas.
Acute appendicitis is the condition most often faced by the general surgeon in the emergency department.1
For over a century, the treatment of choice for an inflamed caecal appendix was removal via the incision described by McBurney2 in 1894. For most patients the intervention could be performed through this small incision, so appendectomy was performed with relative ease. Minimally invasive appendectomy was therefore not pursued with the same enthusiasm as for benign diseases of the gallbladder, as it was claimed that there were no advantages over the traditional technique,3 the operating time was longer4 and hospital costs were higher.5 However, laparoscopic appendectomy has gained acceptance and, although there are still some controversial aspects,6 it has become a familiar technique in emergency general surgery.7
Some unconventional approaches have been used to remove this organ without injuring the abdominal wall. For example, gynaecologists have for 60 years been performing incidental appendectomy while performing a vaginal hysterectomy.8,9
Recently, after Kalloo et al.10 demonstrated the possibility of using natural orifices, appendectomies have been reported in patients with acute conditions using flexible endoscopes via peroral transgastric routes11 and the vaginal orifice.12
This article describes our experience treating acute appendicitis with a minilaparoscopy-assisted transvaginal approach, using rigid instruments.
Patients and MethodsAfter obtaining permission from the Research Ethics Committee and the patients’ informed consent, 8 minilaparoscopy-assisted transvaginal appendectomies were performed in the period from 10th of August 2009 to 30th of June 2010.
Women between 18 and 65 diagnosed with acute appendicitis were operated upon by this method when general surgeons with previous experience in transvaginal cholecystectomies were available to perform emergency surgery. Exclusion criteria were: palpable mass, appendicular abscess, ASA III and IV, morbid obesity (BMI>35), gynaecological diseases, virgins or pregnant women and contraindications for laparoscopic surgery. The operating time, the need for analgesics and postoperative complications were studied.
A gynaecological physical examination, abdominal ultrasound and other studies typical of emergency surgery were performed. Preoperative antibiotic therapy was indicated according to the department protocol: metronidazole 500mg and gentamicin 240mg by intravenous infusion. If a complicated appendicitis (gangrenous or perforated) was diagnosed during the intervention, antibiotic treatment was continued afterwards with the standard frequency and dosages. The administration of oral antibiotics was then re-evaluated, depending on the patient's evolution.
One of the study variables was the need for postoperative analgesics on demand, according to the verbal analogue scale from 0 to 10: patients with mild pain (1–3) were prescribed oral acetaminophen 1g, or an ampoule of avafortan intravenously if the oral route had not been started; moderate pain (4–7) was prescribed 50mg tramadol intravenously; and severe pain (8–10) was prescribed intramuscular morphine at 1mg/kg, due to not having an infusion pump available in the hospital.
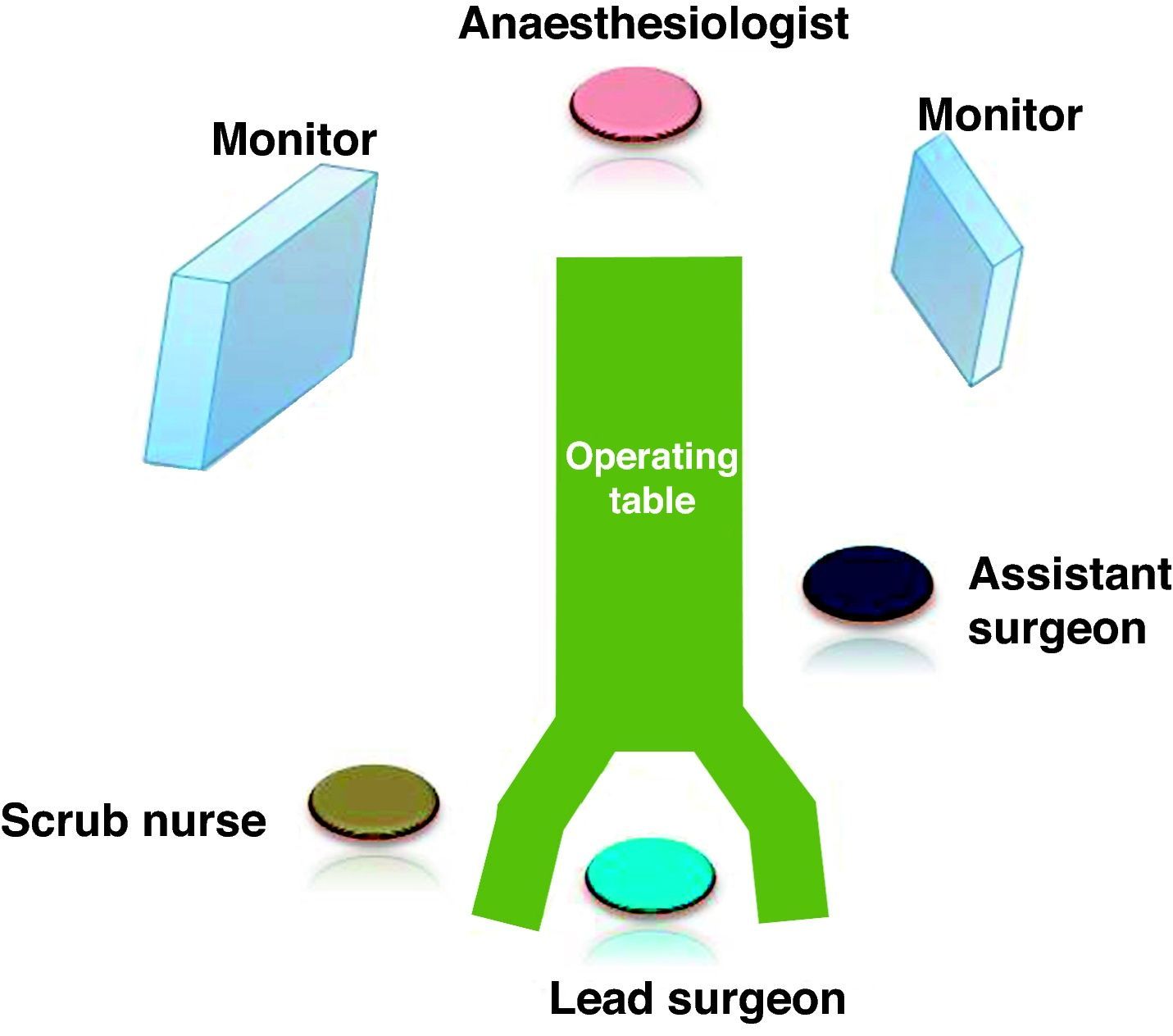
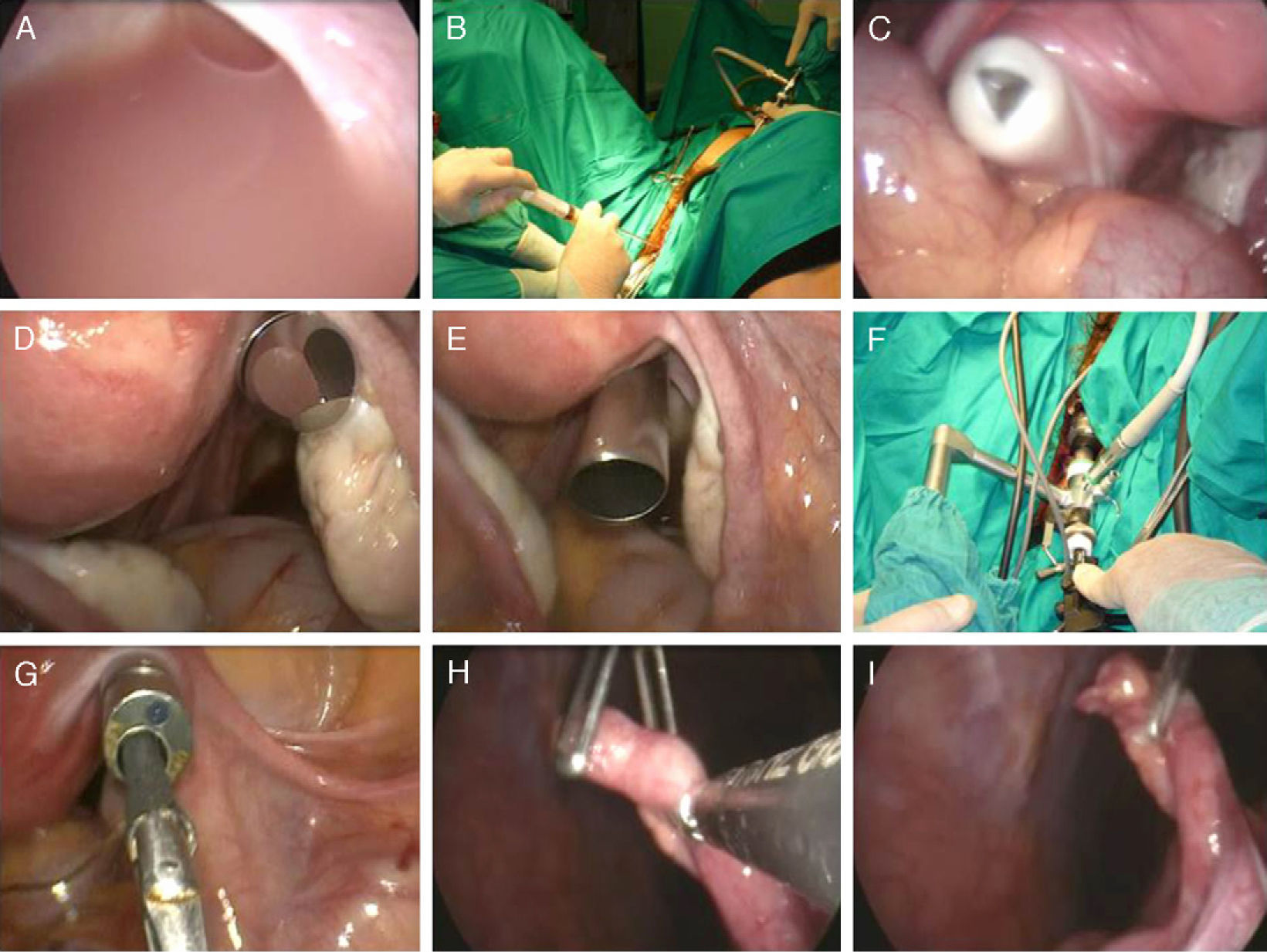
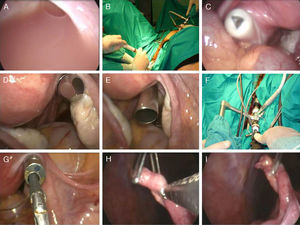
General endotracheal anaesthesia and short-term analgesics (fentanyl) were used. Lithotomy position. Disinfection of the abdomen, vagina and perineum using 10% povidone-iodine. Urine was evacuated with a catheter. The operating table was in the Trendelenburg position (on her left side) and the surgical team as shown in Fig. 1. Pneumoperitoneum was at 15mm Hg, and a 5mm trocar was inserted in the lower inner edge of the navel with a laparoscope of 5mm diameter and 45° inserted through it. The abdomen was explored and the diagnosis confirmed. When pus or seropurulent fluid was found in the pouch of Douglas (Fig. 2A), an internal puncture was performed using a vaginal approach while monitoring for evacuation (Fig. 2B), and a sample taken for bacteriological culture.
(A) Pus in the pouch of Douglas; (B) puncture of the pouch of Douglas; (C)–(E) vaginal trocar entry into the peritoneal cavity; (F) external view of the telescope with a working channel; (G) internal view of the telescope with a working channel; (H)–(I) caecal appendix traction from the umbilical miniport.
An 11mm diameter trocar (Fig. 2C–E) was inserted directly through the vaginal fornix, which led a 10mm diameter telescope with a working channel of 6mm (Karl Storz 26034 AAK), see Fig. 2F and G.
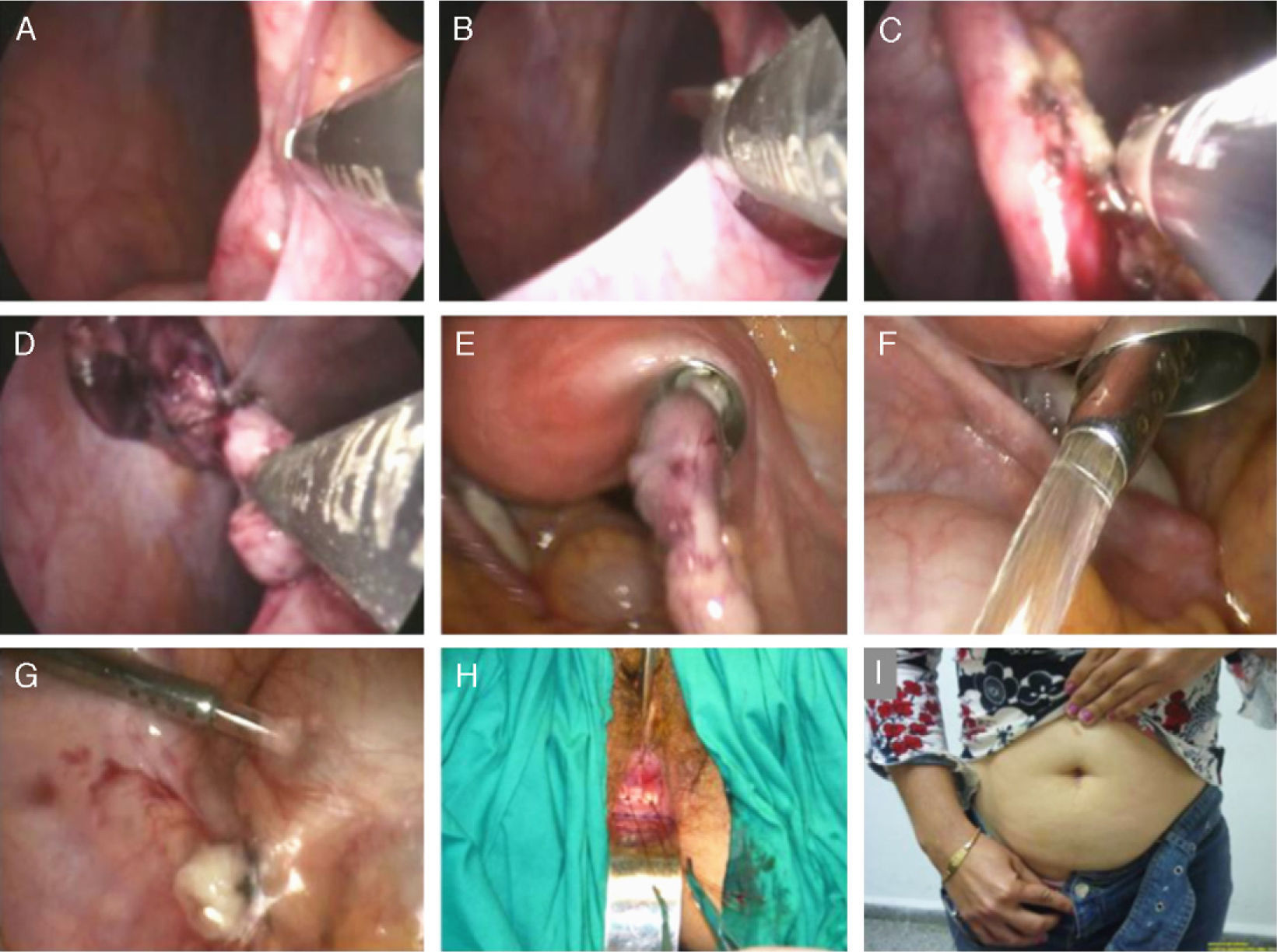
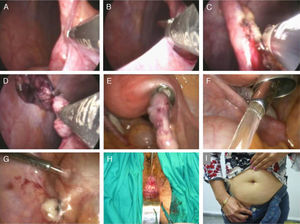
The distal end of the appendix was held with a grasper located in the umbilical miniport (Fig. 2H and I). Then, through the working channel of the laparoscope, adhesions were released (Fig. 3A and B), the mesoappendix electrocoagulated with bipolar clamp (Fig. 3C) and sectioned. The base was ligated with an endoloop and the organ amputated with scissors (Fig. 3D).
(A) and (B) Release of adhesions; (C) electrocoagulation of the mesoappendix; (D) amputation of the caecal appendix; (E) removal of the organ inside the vaginal trocar cannula; (F)–(G) irrigation and aspiration of the region; (H) colpotomy closure; (I) aesthetic result of the intervention.
The stump was treated with monopolar electrocautery and not invaginated. According to its diameter, the appendix was removed within the vaginal trocar cannula (Fig. 3E) or in a laparoscopy bag. The region was irrigated with saline and aspirated (Fig. 3F and G). The vaginal trocar was removed under visual control from the umbilical miniport and the colpotomy was closed with 2 chromic catgut stitches (Fig. 3H).
Outpatient monitoring of patients was scheduled weekly for the first postoperative month, then every month until the third month, then every three months until 1 year after the surgery.
ResultsEight patients with acute appendicitis underwent minilaparoscopy-assisted transvaginal appendectomies. The ages of the patients were between 18 and 42 years (mean 29.6 years). The mean operating time was 48.3min (37–75min).
Administration of analgesics was necessary in the postoperative period for 2 patients: one for moderate pain and the other for mild pain. The remaining 6 did not complain of pain.
Five patients were discharged within 24h and 3 within 48h. Histological analysis of the samples confirmed the diagnosis of uncomplicated acute appendicitis.
Of the 8 patients, 2 have had their 1-year follow-up, and the remaining 6 patients continue with a regular follow-up, having elapsed between 5 and 11 months (mean 8.1 months) since the operation. No procedure-related complications have been found during this time.
DiscussionThe vagina has been used as a route to the abdomen for more than 100 years. In 1896, Kelly13 reported ectopic pregnancies treated by colpotomy. But it was Von Ott14 in 1901 who first used it to observe the peritoneal cavity. Later work by Klaften, Telinde, Palmer and Decker contributed to the development of culdoscopy,15 which became very popular as a means of diagnosis and for minor surgical procedures. In the 1970s it fell out of favour with gynaecologists who preferred laparoscopy.16
In the 1990s, laparoscopic surgery contributed to it being taken up again in some hospitals,17 which took advantage of the magnification of the images and the long surgical instruments to perform more complex and less aggressive surgical procedures. Also at this time, general surgeons and urologists began to use it as an exit port for large surgical specimens.18–23 Removals of large gallbladder stones,18 the spleen,20,21 kidney19,22 and colon segments23 were reported.
Since 1949, when Bueno8 performed the first transvaginal appendectomy in Spain, gynaecologists performed it during vaginal hysterectomy as an additional operation on normal appendices for purely preventive purposes. They used the same instruments for open surgery and accessed the organ when it was visible from the vagina, provided that it was not attached to adjacent structures and had a very loose mesoappendix.9
Pelosi et al.9 suggested releasing adhesions and the full mobilisation of the organ laparoscopically to then perform the appendectomy through the vagina using the open surgery techniques described before. Tsin et al.24 were first to do this through the vagina using video-assisted surgery techniques and an abdominal miniport. Placing a 5–12mm diameter trocar at its top allowed the use of staplers.
However, it was only after the proposal by Kalloo10 when general surgeons became interested in the vaginal approach as an entry route to the abdomen. Within a short period of time, there were numerous studies showing that surgery was possible on organs as distant as the gallbladder,25–28,33–39 liver,29,41 stomach30,31 and spleen,32,42 using either flexible25–35 or rigid36–41 instruments, and with the assistance25–32,36–41 or not33–35 of miniports in the abdominal wall.
Despite its proximity to the vaginal fornix, transvaginal appendectomies are not reported frequently in patients undergoing surgery for appendicitis. Palanivelu et al.12 reported the first cases in 2007 on 6 patients using a flexible endoscope. Conversion to laparoscopic surgery because of technical difficulties was required in 3 (50%) of them. The help of a 3mm diameter miniport in the abdominal wall was needed in 2 cases, and 1 (12.5%) was performed entirely using the vaginal approach (T-NOTES). Bernhardt et al.43 performed a similar intervention in a woman with subacute appendicitis. Recently, Zorrón et al.44 reported a series of 37 patients.
To the best of our knowledge, there are no published reports of transvaginal appendectomies in women with acute appendicitis performed with rigid instruments and only a miniport in the abdominal wall.
The 8 appendectomies in our series were performed without difficulty: 5 were oedematous and 3 fibrinopurulent appendicitis. The latter group had pus or seropurulent fluid in the pouch of Douglas, without the organ being perforated or the formation of abscesses. The fluid was aspirated through the vagina, which facilitated the subsequent entry of trocars under internal control. Given that the possibility of postoperative intraperitoneal septic complications is not uncommon in acute appendicitis, and that the transvaginal approach may lead to confusion about the origin of any germs (whether from the inflamed organ or the bacterial flora of the vaginal opening), it was decided to take an initial sample of peritoneal fluid for culture analysis to help identify the source of any infection. However, this complication did not occur.
The treatment of the mesoappendix at the base of the organ was always performed through the vaginal port, using the working channel of the endoscope. The umbilical miniport was used only for traction and mobilisation of the appendix. This channel also facilitated the passage of 5mm diameter clippers. However, if the surgeon requires the use of larger diameter (10mm) clippers or staplers, the camera can be moved to the umbilical miniport and the staplers inserted through the vaginal port, after removing the telescope with a working channel.
The use of staplers reduces operating time and makes the intervention less difficult,45,46 by placing a larger diameter (5–12mm) trocar into the vagina. These were not used for patients treated in our series, because its high cost did not allow it to be used in such a common operation.
Appendectomies were technically easy to perform, so it was possible to perform surgery with only 2 working ports (vaginal and umbilical). However, in difficult cases, such as retrocaecal appendicitis, placing a second port (5mm diameter) in the vaginal fornix or inserting working instruments adjacent to the 10mm trocar using the same hole, gives greater opportunities for dissection. In our experience, when performing transvaginal cholecystectomies,37 we found that inserting instruments through the same trocar hole usually caused gas to escape, necessitating a vaginal tamponade with a wet compresses, which was certainly uncomfortable for the surgeon. So we preferred to insert a second trocar.
The operating time in our series was similar to laparoscopic appendectomies performed in our hospital47 and in other international studies.48 However, it was lower than that reported in transvaginal appendectomy using only flexible instruments.12 None of our patients required conversion to laparoscopic or open surgery, but that may be because we had no complex cases. Five of our patients were discharged from hospital within 24h of surgery, while the remaining 3 had purulent or seropurulent fluid in the pelvic cavity and were kept under observation for 48h, without continued preoperative antibiotic treatment.
Although only 2 patients required parenteral or oral analgesic treatment, this was a very small series for these indicators to be assessed objectively.
Hybrid techniques represent an intermediate step between laparoscopic surgery and “pure” surgery through natural orifices (T-NOTES/T-NOS).17,31,49 They contribute to clinical study and technological innovation, while ensuring greater safety for the patient.
Currently, a hybrid transvaginal appendectomy has advantages over pure ones. Prior to performing a colpotomy, the umbilical miniport allows the peritoneal cavity to be explored and confirms the diagnosis, which is sometimes difficult in a woman.50 This makes it possible to detect previously undiagnosed endometriosis, which would contraindicate the vaginal route of entry39; it provides an opportunity for the surgeon to identify the exact location of the caecal appendix (which is variable in humans) and to generally assess the degree of difficulty of the intervention. This makes it possible from the outset to decide whether a second working port needs to be placed in the vaginal fornix.
Secondly, internal observation guarantees that entry into the peritoneal cavity is as safe as possible. Despite the experience of gynaecologists with the “blind” opening of the vaginal fornix, where low rates of iatrogenic cases are reported,51 entry through such a small space is not without iatrogenic injuries to adjacent important organs.52 Therefore, and because of the growing interest in this surgical approach, gynaecologists have suggested trying new techniques to make the vaginal orifice a safer gateway to the abdomen without any monitoring.53–55 However, these are not yet widespread, nor are there studies showing any benefits.
In addition, there are no large series published and the vaginal approach has not been studied under the new concept of surgery through natural orifices, where the number and diameter of trocars placed in the vaginal fornix are greater than previously known. They also include new procedures such as direct insertion of trocars into the peritoneal cavity to achieve greater speed and improved sealing,41 which is a manoeuvre that would be impossible without internal visual inspection.
Finally, an umbilical miniport during surgery ensures adequate assistance. It facilitates dissection manoeuvres, and the entire peritoneal cavity can be irrigated and aspirated through it. Furthermore, if there is generalised peritonitis, a standard 5mm diameter cannula can be used and the working channel telescope in the vaginal port can be replaced with an extra long one of 30° or 45°.
Anatomically, the right iliac fossa is located very close to the vaginal fornix and is nearly facing it, so it can be addressed without great difficulty using a rigid telescope with a working channel. It is known that the current flexible endoscopes are complex and difficult to use in open areas such as the peritoneal cavity.31,56,57 Disadvantages include the fact that they are unstable along their axis, which makes positioning manoeuvres difficult in the surgical field.32 Without the support of the luminal wall, gravity causes the endoscope to settle on other organs as it passes through58; their very flexibility limits any transmission of force59; their working channels only allow the passage of small diameter instruments which cannot manage the triangulation necessary to perform the dissection operations, due to sliding along parallel channels close together60; the optics and working instruments do not have independent sideways movement and move along together simultaneously61; in addition, it is difficult to perform quick manoeuvres if there is any bleeding, and as yet there are no adequate tools for haemostasis.52
Technological development will surely provide flexible instruments that will play a central role in all surgical activity.62–64 However, it is not currently possible to dispense with rigid instruments, or the assistance of at least one miniport in the abdominal wall, if safe, efficient and reproducible surgery is required through natural orifices.31,39
Minilaparoscopy-assisted transvaginal appendectomy with the use of rigid instruments in selected women with acute appendicitis is a feasible, safe method with better cosmetic results than laparoscopic appendectomy. However, prospective randomised studies are needed to demonstrate its advantages.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Castro Pérez R, et al. El abordaje transvaginal en la apendicitis aguda. Cir Esp. 2011;89:517–23.