Portal venous gas is a radiological sign that up until a few years ago was associated with evolved stages of intestinal ischemia and a tragic prognosis. However, more and more authors have been reporting cases of portal venous gas associated with acute inflammatory processes with survival rates of 70%–80%.1,2
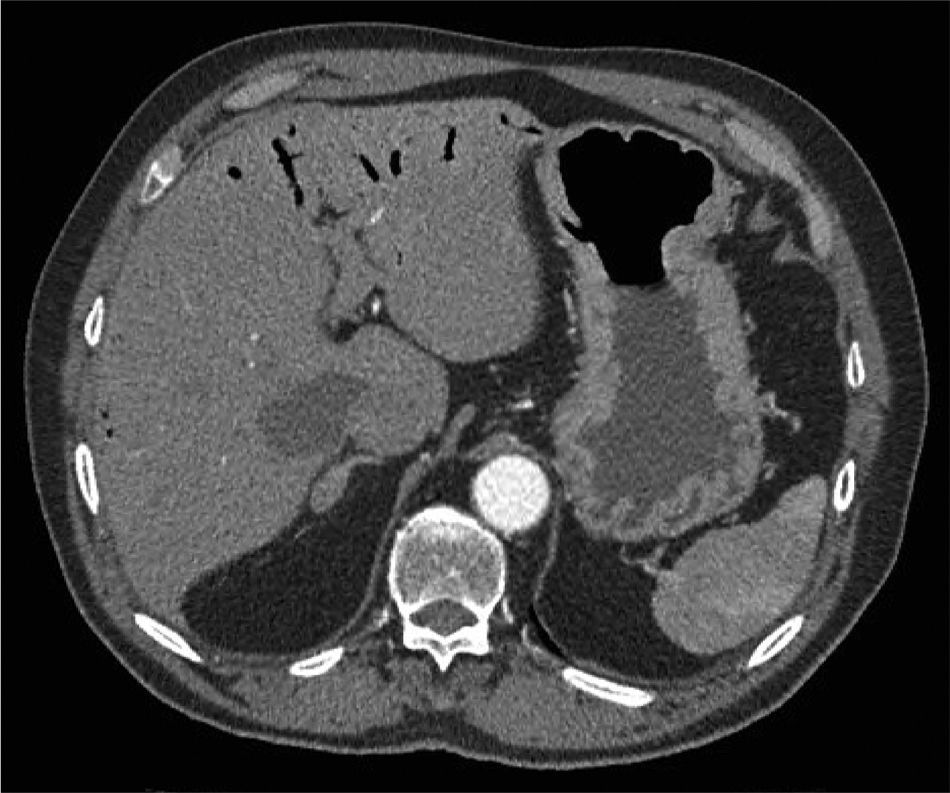
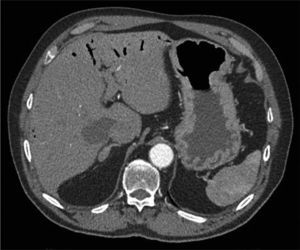
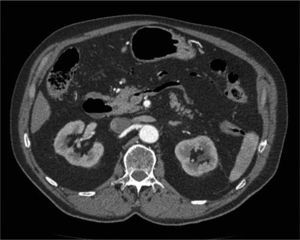
We present the case of a 62-year-old male with a history of hypertension. He came to the Emergency Department after an episode of abrupt central chest pain, hypotension and having fallen to the ground without loss of consciousness. Physical examination revealed pale mucous membranes, sweating, blood pressure 65/45mmHg and a heart rate of 34 beats per minute in sinus rhythm. He presented a protruding abdomen with no signs of peritoneal irritation. After stabilizing the patient, and given the suspicion of aortic dissection, we quickly decided to perform a thoracoabdominal-pelvic computed tomography (CT) scan with intravenous contrast, which showed extensive portal venous gas, with gas in the inferior mesenteric and splenic veins, and no other justifiable findings (Figs. 1 and 2). Blood test results (hematology, biochemistry, coagulation) were non-significant. Due to the discrepancy between the symptoms and radiology results, a meticulous exploratory laparoscopy was carried out, which showed no evidence of any cause that would explain the presence of gas in the portal venous system. The patient was admitted for further monitoring and remained asymptomatic throughout his hospital stay. He was discharged 72h later after another abdominal-pelvic CT that demonstrated no relevant findings. After 6 months of follow-up, the patient remains asymptomatic.
Portal venous gas is a radiological sign with numerous etiologies. It has been described in association with vascular pathology, infections, hollow viscus perforation, abdominal trauma and inflammatory diseases, or secondary to endoscopic studies, chemotherapy, drug use, etc.2,3 The pathophysiology of this finding is not well understood. Factors that are supposedly related with the appearance of gas in the portal venous system are: gas leak caused by certain gas-producing microorganisms in the intestinal lumen or in abscesses, or the presence of these microorganisms in the portal venous system.3
The diagnosis of portal venous gas has increased in recent years due to the growing number of radiological examinations performed and their greater sensitivity. CT is the radiological test of choice because it can diagnose the underlying cause and direct treatment.4,5
In the last few years, several authors have attempted to create management algorithms for portal venous gas in order to avoid unnecessary laparotomies and achieve more efficient treatment. In short, we could say that the objective is to determine whether the underlying cause is a pathology that requires emergency surgery (intestinal ischemia, peritonitis, etc.), a reversible cause (intra-abdominal abscess, inflammatory disease, gastroenteritis, etc.) or an incidental finding. In the former instance, in addition to the radiological sign of portal venous gas, the patient will have signs of sepsis, and mortality can reach 80%–90%. However, when it is an incidental finding, which is a diagnosis that is reached after having ruled out all other possible causes of portal venous gas, mortality is 0%.6–9 In this case, and considering the possible pathophysiology of portal venous gas, it would seem advisable to use prophylactic antibiotics. However, there are no studies recommending their generalized use.
Therefore, it is important to make a proper differential diagnosis of the presence of gas in the portal venous system and to rule out causes requiring emergency surgical treatment as soon as possible. Do not forget that it may be a chance finding that requires no specific therapy.
Please cite this article as: Garcés Albir M, López Mozos F, Martí Cuñat E, Martí Obiol R, Ortega Serrano J. Neumatosis portal-hepática-mesentérica, ¿es siempre un diagnóstico ominoso? Cir Esp. 2014;92:65–67.