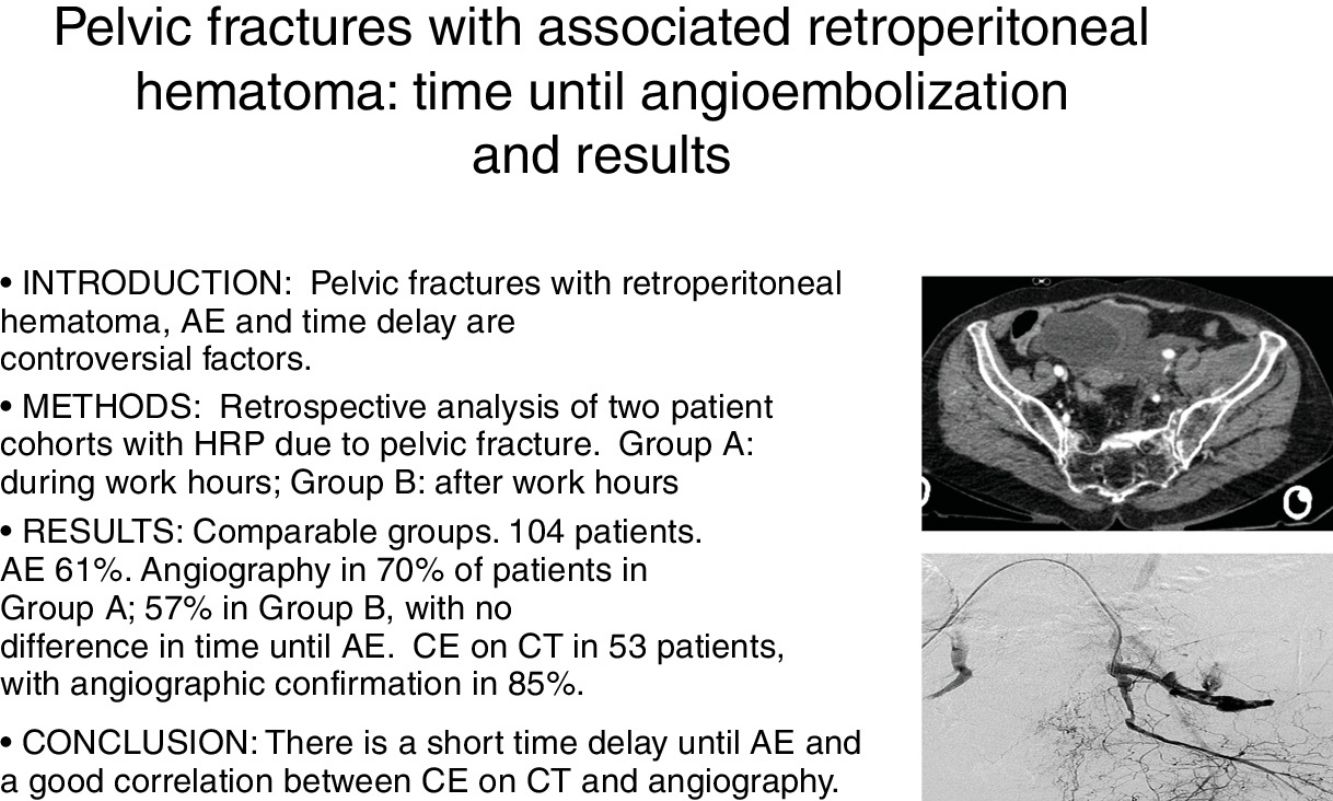
Two areas of controversy in the management of bleeding pelvic fractures are the need to perform angioembolization (AE) in patients with a retroperitoneal hematoma (RPH) but no contrast extravasation (CE) on Computerized Tomography (CT) and/or angiography, and the delay to AE.
Our main objective was to assess whether there had been differences in the percentage and delay to AE between patients admitted on weekdays versus off-hours (weekends and admission after 3pm) at our hospital. Our hypothesis was that angiography and AE would be more frequent on weekdays, and the time delay would be longer during off-hours, with a higher mortality in this latter group for a similar overall severity. A secondary objective was to assess the correlation between CE on CT scan and angiography.
MethodsRetrospective review of two cohorts of patients with RPH from a pelvic fracture during a period of 24 years. Patients were divided depending on the time of arrival (Group A: weekdays, and Group B: off-hours). The decision to perform angiography and AE was made by the general surgeons on call, in consensus with the interventional radiologist. We analyzed demographics, mechanism of injury, associated injuries, physiologic and anatomic trauma scores, CE on CT scan, need of AE, Intensive Care Unit (ICU) stay and mortality.
Results104 patients were admitted with RPH from a pelvic fracture. We performed AE in 63 cases (61%). The groups were comparable in the variables analyzed. In 70% of patients in group A, angiography was done, vs 57% in group B, with the same median time delay. CE on CT scan was seen in 53 out of 96 patients and confirmed by angiography in 45 (85%) of them. No significant differences were found in mortality between the two groups.
ConclusionsThere was a short delay from admission to AE, even during off-hours, and a good correlation of CE on CT scan and angiography.
El tratamiento de las fracturas de pelvis con hematoma retroperitoneal (HRP) es controvertido. Especialmente la necesidad de angioembolización (AE) cuando no hay extravasación de contraste (EC) en la tomografía computarizada (TC) o angiografía. Otro aspecto relevante es el retraso hasta la misma.
Nuestro objetivo ha sido determinar si existen diferencias en el tiempo hasta la AE entre los pacientes admitidos durante el horario laboral y los admitidos fuera del mismo y durante los fines de semana y festivos. Nuestra hipótesis era que la angiografía y AE serían más frecuentes en el horario laboral, y el tiempo hasta las mismas sería superior fuera del horario laboral habitual, con una mortalidad mayor en este grupo para una gravedad global similar. Un objetivo secundario ha sido valorar la correlación entre EC en la TC y la angiografía.
MétodosAnálisis retrospectivo de 2 cohortes de pacientes con HRP por fractura de pelvis. Se estudia la realización de angiografía dividiendo a los pacientes según su hora de llegada a lo largo de un periodo de 24 años (grupo A: horario laboral, y grupo B: fuera del mismo). La indicación de angiografía y AE fue realizada por la guardia de cirugía general, en consenso con el radiólogo intervencionista. Se han analizado variables demográficas, mecanismo lesivo, lesiones asociadas, gravedad fisiológica y anatómica, EC en la TC y la angiografía, necesidad de AE, estancia en unidad de cuidados intensivos (UCI) y mortalidad.
ResultadosSe admitió a 104 pacientes con diagnóstico de HRP por fractura pélvica. Se realizó angiografía, con AE en 63 casos (61%). Los grupos eran comparables en las variables analizadas. En el 70% de los pacientes del grupo A se realizó angiografía, frente al 57% del grupo B, sin diferencias en tiempo hasta la AE. Se demostró EC en la TC en 53 de los 96 pacientes en los que se hizo, lo que se confirmó mediante angiografía en el 85%. No hubo diferencias estadísticamente significativas de mortalidad entre ambos grupos.
ConclusionesSe demuestra un tiempo corto entre la admisión en Urgencias y la AE, sin relación con el momento del ingreso durante el día, y una buena correlación entre la EC en la TC y la angiografía.
Pelvic fractures with associated retroperitoneal hematoma are a therapeutic challenge. Despite proper treatment, these injuries can be very serious, with high associated morbidity and mortality rates ranging from 8.8% to more than 40% according to the sources consulted.1–5 In addition, these injuries are usually accompanied by lesions in other areas, most frequently long bone fractures (40%), abdominal (32%) and thoracic (15%) injuries.2,3,5
Many authors accept that hemorrhage occurs as a result of pelvic venous bleeding and from the trabecular bone in up to 85% of cases, while arterial bleeding is identified in 3%–10%. In the latter, angioembolization (AE) has become the treatment of choice for many groups.1,4,6,7 In recent years, several authors have questioned these low arterial bleeding figures and have estimated them at a much higher percentage (ranging between 15 and 42%2,3,8), while also supporting the therapeutic role of angiography and AE in these patients.
Contrast extravasation (CE) on computed tomography (CT) scans is an early indicator of arterial bleeding, although its absence does not exclude bleeding as there may be a vasospasm reactive to volume depletion.9 When these patients without CE are only transient responders to blood replacement therapy, many authors argue the need for AE.1,4,8,9 On the other hand, there are cases in which, in spite of CE on CT that is usually venous in origin, it would not be necessary to perform angiography or AE since patients remain hemodynamically stable after their arrival.8
Another factor to assess is the time transpired until arteriography and AE in transient responders, as the interventional radiology team is only available during work hours. Invasive external pelvic fixation, together with preperitoneal packing in non-responding patients, complicates the management algorithm, which may include complementary and non-exclusive techniques, whose use must be clearly protocolized at hospitals that treat this type of patients with certain frequency.4,10–17 Likewise, it is necessary to take into account that AE, especially when non-selective, is not free of complications, such as gluteal necrosis, wound infection, claudication, neuropathy, impotence or difficult fracture consolidation.1,12 The most frequent cause of early mortality in cases of severe pelvic fractures continues to be hemorrhage, although a delay in decision-making or in time to AE, especially on holidays, sometimes contributes to this high mortality. Hence the importance of establishing diagnostic and therapeutic algorithms based on the hemodynamic status of patients, which provides individualized and effective management of these injuries.11,18–20 This requires a multidisciplinary approach that includes anesthesiologists or intensive-care specialists, surgeons, trauma surgeons, interventional radiologists and hematologists (mass transfusion protocols).1,8,11,21
Our objective was to determine whether there have been differences in time to AE between patients admitted during hospital work hours (8 am–3 pm) and those admitted after that time, during weekends and on holidays. Our hypothesis was that angiography and AE would be more frequent during work hours, and the time transpired would be longer during off-hours, with a higher mortality in this group for similar overall severity. The secondary objectives were to assess the correlation between CE on CT scans and angiography, and the need for AE in both groups.
MethodsThis is a retrospective study comparing 2 cohorts of patients admitted to the Emergency Department between September 1993 and July 2017 with retroperitoneal hematoma associated with pelvic fracture. In the vast majority, CT was performed and later angiography was used in cases requiring it. Patients from these 2 cohorts were classified according to the time of hospital admission: patients who were admitted on weekdays between 8 am and 3 pm (group A); and patients who were admitted on the weekend, holidays or weekdays after 3 pm (group B), when there is no interventional radiologist on duty at our hospital. This study was approved by the Ethics Committee.
The groups were found to be comparable in demographic characteristics, comorbidities, mechanisms of injury, associated injuries, Revised Trauma Score (RTS) and Injury Severity Score (ISS). No complementary hemostasis techniques were evaluated, such as invasive external pelvic stabilization, which was infrequently done at our hospital until a few years ago.
We analyzed the need for AE and the median time transpired beforehand, associated abdominal surgery, need for transfusion and required blood units, intensive care unit (ICU) stay and mortality. We defined the time until AE as the time transpired between the admission to the Emergency Department and the moment when the procedure was completed by the interventional radiologist, not when the angiographic procedure began. We did not analyze whether AE was selective or not; however, and with the aim of reducing complications associated with this procedure, AE was as selective as possible according to the intervention protocol. Whenever CE was detected during angiography, AE was performed. In the absence of CE on angiography, AE was performed depending on hematoma volume, patient hemodynamic situation and the consensus of the surgical, anesthesia and interventional radiology teams on duty.
All patients who were candidates for AE underwent diagnostic femoral angiography (pelvic arteriography and selective arteriographies) in order to identify the arterial injury and plan treatment. AE was done as selectively as possible according to the angiographic findings. Depending on each case, different embolization agents were used, mainly metal coils or absorbable material (hemostatic gelatin sponge in dilution), either isolated or in combination.
The statistical analysis was carried out using the IBM SPSS Statistics program, version 19. The 2 cohorts were compared by applying the chi-squared test and Fisher's exact test for the analysis of qualitative variables. For the comparison of quantitative variables, nonparametric tests (Mann–Whitney U) were used. A P value <.05 was considered statistically significant.
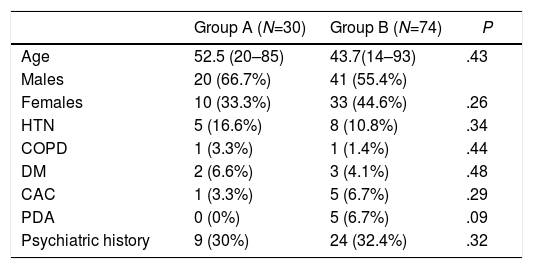
ResultsAngiography was performed in 63 (61%) of the 104 patients admitted with retroperitoneal hematoma associated with pelvic fracture during the study period; 30 patients belonged to group A and 74 to group B. The 2 groups were comparable in demographic variables, medical and psychiatric comorbidities, history of alcohol consumption and parenteral drug addiction (PDA). No statistically significant differences were found between these 2 cohorts (Table 1).
Demographic Variables and Comorbidity.
| Group A (N=30) | Group B (N=74) | P | |
|---|---|---|---|
| Age | 52.5 (20–85) | 43.7(14–93) | .43 |
| Males | 20 (66.7%) | 41 (55.4%) | |
| Females | 10 (33.3%) | 33 (44.6%) | .26 |
| HTN | 5 (16.6%) | 8 (10.8%) | .34 |
| COPD | 1 (3.3%) | 1 (1.4%) | .44 |
| DM | 2 (6.6%) | 3 (4.1%) | .48 |
| CAC | 1 (3.3%) | 5 (6.7%) | .29 |
| PDA | 0 (0%) | 5 (6.7%) | .09 |
| Psychiatric history | 9 (30%) | 24 (32.4%) | .32 |
PDA: parenteral drug addiction; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; HTN: hypertension; CAC: chronic alcohol consumption.
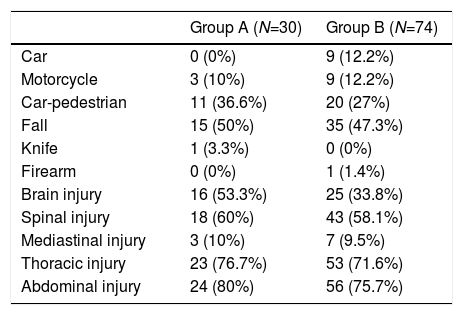
Regarding the mechanisms of injury, there was only a statistical difference in the greater frequency of car collisions occurring during holidays and outside work hours, while no differences were observed in the remaining mechanisms of injury (Table 2). The most frequent mechanism in both groups was a fall. Table 2 shows the associated injuries, which are frequent with high-energy trauma capable of causing complex pelvic fractures. In general, there was a greater presence of associated injuries in the cohort of patients admitted on holidays. The most common were intra-abdominal injuries (80% and 71.6%, respectively) and thoracic injuries (76.7% and 71.6%, respectively). Other frequent injuries were vertebral and cranial.
Mechanism of Injury and Associated Injuries.
| Group A (N=30) | Group B (N=74) | |
|---|---|---|
| Car | 0 (0%) | 9 (12.2%) |
| Motorcycle | 3 (10%) | 9 (12.2%) |
| Car-pedestrian | 11 (36.6%) | 20 (27%) |
| Fall | 15 (50%) | 35 (47.3%) |
| Knife | 1 (3.3%) | 0 (0%) |
| Firearm | 0 (0%) | 1 (1.4%) |
| Brain injury | 16 (53.3%) | 25 (33.8%) |
| Spinal injury | 18 (60%) | 43 (58.1%) |
| Mediastinal injury | 3 (10%) | 7 (9.5%) |
| Thoracic injury | 23 (76.7%) | 53 (71.6%) |
| Abdominal injury | 24 (80%) | 56 (75.7%) |
CT scans were performed in 96 of the 104 patients evaluated (92%). The omission of CT in 8 cases was due to hemodynamic instability requiring urgent surgical intervention in 2 cases, and angiography was performed in the remaining 6 cases.
In terms of management, in group A 70% of patients underwent AE, compared to 57% in group B (Table 3). On the other hand, in 12 cases (44%), AE was not performed because CE was not observed on CT or angiography.
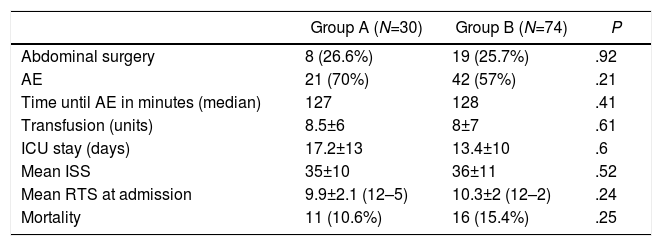
Results; Dispersion Expressed as Standard Deviation.
| Group A (N=30) | Group B (N=74) | P | |
|---|---|---|---|
| Abdominal surgery | 8 (26.6%) | 19 (25.7%) | .92 |
| AE | 21 (70%) | 42 (57%) | .21 |
| Time until AE in minutes (median) | 127 | 128 | .41 |
| Transfusion (units) | 8.5±6 | 8±7 | .61 |
| ICU stay (days) | 17.2±13 | 13.4±10 | .6 |
| Mean ISS | 35±10 | 36±11 | .52 |
| Mean RTS at admission | 9.9±2.1 (12–5) | 10.3±2 (12–2) | .24 |
| Mortality | 11 (10.6%) | 16 (15.4%) | .25 |
AE: angioembolization; ISS: Injury Severity Score; RTS: Revised Trauma Score; ICU: intensive care unit.
Approximately one in every 4 patients (27 in total) required associated abdominal surgery, performed before the AE in the majority of cases (41%), compared to 15% of patients treated surgically after AE. Other therapeutic alternatives, such as external pelvic fixation, were used in 14 cases, and preperitoneal packing was necessary in only 3 patients of our series during the period of time considered.
There were no differences between cohorts in the time elapsed until AE, transfused blood units, physiological severity at admission (RTS) or the overall anatomical severity (ISS). Regarding mean ICU stay and mortality, there were no statistically significant differences, although there was a longer hospital stay in the work-day cohort (17 versus 13 days) and higher mortality on holidays (15.4% vs 10.6%) (Table 3). As for the complications associated with AE, we identified 2 cases of gluteal necrosis and one case of paresis.
CE was observed on the CT scans of only 53 (55%) of the 96 patients in whom this test was done, and this finding was confirmed on arteriography in 45 (85%), which demonstrates an adequate sensitivity of CT for CE. In 43 cases, no CE was observed on CT, which was confirmed by arteriography in 14 (13.5%), and required AE later.
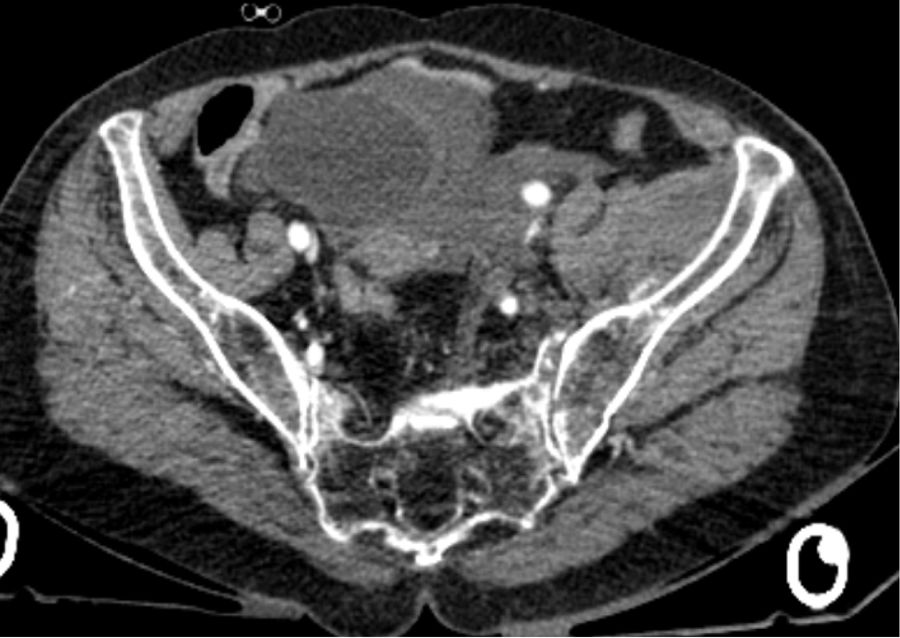
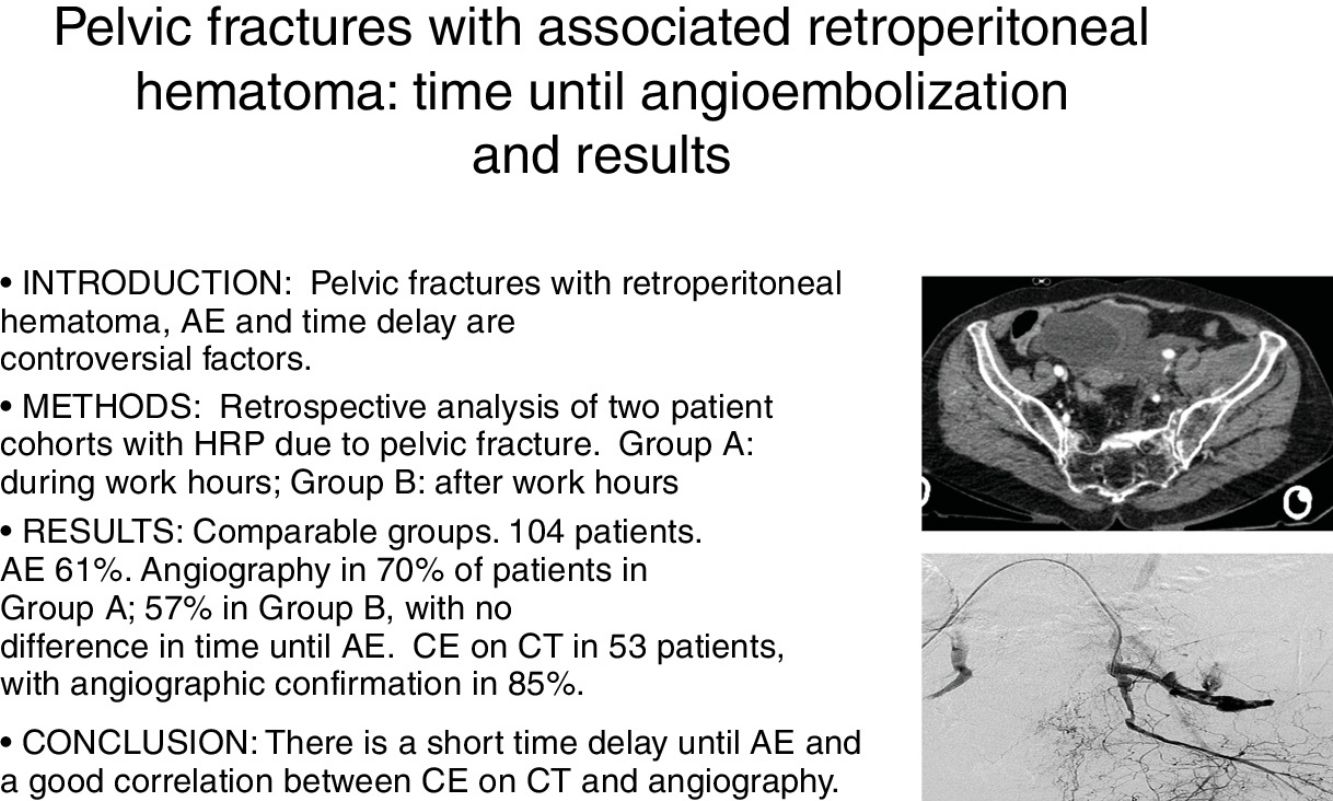
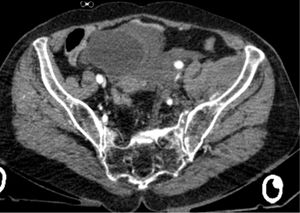
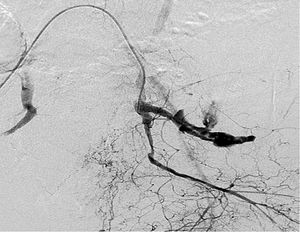
In Figs. 1 and 2, which correspond to the same patient, the presence of CE was observed on CT and subsequent correlation with CE on arteriography.
Out of the 63 patients who underwent AE, hemodynamic stability was achieved after the procedure in 76.2% of cases. In all cases, cessation of arterial bleeding was certified in the final angiography performed after the AE. The main cause of mortality was massive bleeding in 15 (55.5%) of the 27 deceased, followed by associated neurological lesions in 26%. Other causes, in order of frequency, were adult respiratory distress syndrome (ARDS), one probable myocardial contusion and sudden pulmonary thromboembolism (PTE) during transfer to the hospitalization ward.
DiscussionDespite both diagnostic and therapeutic innovations, pelvic fractures with hemodynamic instability continue to be a challenge for orthopedic and general surgeons due to the high rates of morbidity and mortality as well as the high frequency of associated injuries.1–4 Frequently, these injuries cause serious hemorrhage that are venous in origin in most cases. However, some authors defend that arterial bleeding is much more frequent than previously thought and support the early use of angiography in the management algorithm.2,3 Due to this dual hemorrhage origin, 2 treatment schemes have been proposed once the existence of injuries requiring urgent surgical intervention has been ruled out. While in the English-speaking world the tendency is to perform early AE followed by pelvic stabilization, the Central European school defends urgent surgery with packing and pelvic fixation.5,12 In cases of hemodynamic instability and non-responding patients, preperitoneal packing and invasive external pelvic fixation are recommended, while transient responders, depending on availability, can opt for preperitoneal packing or AE.5,9,14–16,21 Some studies have observed that, in patients with arterial bleeding who are candidates for AE, if the drop in blood pressure is more significant, the need for transfusion of blood products is greater9,21 and the ISS is higher.18
In cases of arterial bleeding confirmed by abdominal CT or angiography, AE is preferred. The main drawback is the delay until the completion of the procedure, which in certain hospitals and at certain times of day (work versus off-hours and holidays) implies a significant wait, even in critical situations of hemodynamic instability.1,10,11,17,18,20 Thus, Matshusima et al. show an increase in mortality after every hour of waiting from admission to AE, going from a mortality of 0%, when the AE is performed within the first hour, up to 25.3% when it is performed 3–4h after arrival.20 Therefore, when the availability of interventional radiology is limited, other alternatives such as preperitoneal packing are preferred.6,11 In addition, other factors, including delayed diagnosis and decision-making or the need for another type of surgical intervention for associated injuries, contribute to the delay in treatment, as indicated by Tesoriero et al.11 Marzi et al. emphasize that these are unstable patients who may not tolerate such time delays.15
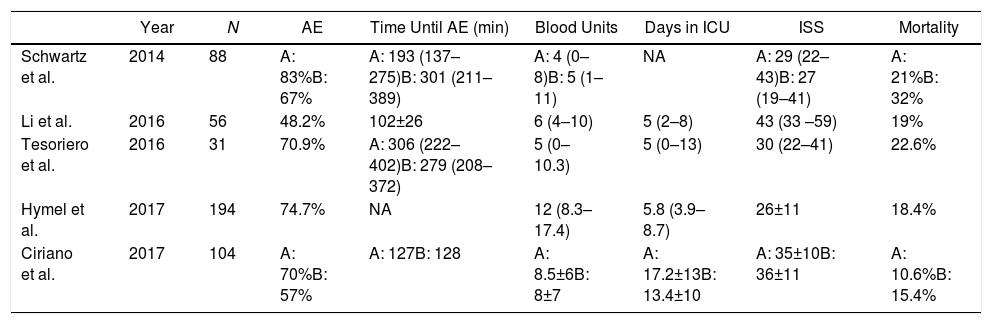
The trauma scale scores of our patients and their length of ICU stay reflect the anatomical and physiological severity of their injuries. There were no differences in the physiological severity between the 2 groups at admission (measured by the RTS, Table 3), nor in the global anatomical severity (measured by the ISS, Table 3); the results of the latter were very similar to reports by other groups (Table 4).10,13,17,20 Even so, it is not easy to compare our results globally with those of other groups, as ours is a biased study limited to patients with pelvic fractures and retroperitoneal hematoma, in whom the need to perform angiography was assessed, with or without AE.
Comparison of Recent Results From Different Study Groups.
| Year | N | AE | Time Until AE (min) | Blood Units | Days in ICU | ISS | Mortality | |
|---|---|---|---|---|---|---|---|---|
| Schwartz et al. | 2014 | 88 | A: 83%B: 67% | A: 193 (137–275)B: 301 (211–389) | A: 4 (0–8)B: 5 (1–11) | NA | A: 29 (22–43)B: 27 (19–41) | A: 21%B: 32% |
| Li et al. | 2016 | 56 | 48.2% | 102±26 | 6 (4–10) | 5 (2–8) | 43 (33 –59) | 19% |
| Tesoriero et al. | 2016 | 31 | 70.9% | A: 306 (222–402)B: 279 (208–372) | 5 (0–10.3) | 5 (0–13) | 30 (22–41) | 22.6% |
| Hymel et al. | 2017 | 194 | 74.7% | NA | 12 (8.3–17.4) | 5.8 (3.9–8.7) | 26±11 | 18.4% |
| Ciriano et al. | 2017 | 104 | A: 70%B: 57% | A: 127B: 128 | A: 8.5±6B: 8±7 | A: 17.2±13B: 13.4±10 | A: 35±10B: 36±11 | A: 10.6%B: 15.4% |
AE: angioembolization; ISS: Injury Severity Score; NA: not available; ICU: intensive care unit.
Schwartz et al.: dispersion expressed as interquartile range.
Li et al.: dispersion expressed as standard deviation for the time until AE and as interquartile range for blood units, days in ICU and ISS.
Tesoriero et al.: dispersion expressed as interquartile range.
Hymel et al.: dispersion expressed as standard deviation (ISS) and interquartile range (blood units and days in ICU).
Ciriano et al.: dispersion expressed as standard deviation.
Table 4 shows the results of several recent series of patients who have undergone angiography, including ours, although few reflect the time transpired until AE. We have observed in our series a need for AE similar to that of other groups1,6,7,17 (Table 4). However, there are groups that describe an AE rate of only 3.8%, which is much lower than descriptions in the literature, arguing that it is due to the better identification of patients who could benefit from the procedure. They also describe more selective use, reserving AE for patients with a more compromised hemodynamic state and a tendency to develop severe, persistent hypotension and tachycardia.7
Approximately one out of every 4 patients in our 2 groups required abdominal surgery, compared to 51.8% in the Li et al. study6 and 81.3% in the Tesoriero et al. study.11 There were no differences between the need for transfusion on weekdays or holidays (8.5 and 8 units, respectively), nor were their differences compared to other published studies, in which the transfused blood units ranged from 5 to 13.1,6,10,11,13,17 We had a longer mean ICU stay, between 13 and 17 days, compared to the 5–8 days reported by other groups.6,11,13,20 Our mortality rate was low (11% on working days and 16% on holidays) compared to other studies,1,6,7,9,17,20 as shown in Table 4. The series by Schwartz et al. stands out, with a mortality rate that ranged from 21% on working days to 32% on holidays.17
We believe that the main finding of our study is the rapid completion of AE, which was little more than 2h in both groups, compared to the times reported by other series (Table 4). Undoubtedly, the existence of on-call interventional radiologists dedicated to the management of these patients within a consensus multidisciplinary protocol is an essential factor to reduce mortality in this type of injuries. Fortunately, the incidence is not very significant in our setting, so the presence of the interventional radiologist is not required very often for this reason, as our data demonstrate. The lack of time differences before AE in our series can be explained, in part, by the constant simultaneous occupation of our 2 interventional radiology rooms during normal work hours, and their usual availability outside of that timeframe, which means that they are frequently not immediately available in the morning.
Finally, and as a secondary objective of our study, the good correlation between CE on CT and angiography is worthy of mention, since 85% of the patients who presented CE on CT correlated with bleeding on arteriography. This finding is dissimilar from other studies, like Juern et al., in which this correlation was much lower.19
Among the weaknesses of this study is the long period of time it covers, with important variations in both the indication for and the techniques of angiography and AE. In addition, as already mentioned, it is a study limited to patients with pelvic fracture and associated retroperitoneal hematoma, in whom the need to perform angiography has been assessed. This presupposes a certain hemodynamic control of the patients, so that our mortality rate does not reflect the overall rate of our patients treated for pelvic fractures. Therefore, it is not easy to assess the exact role of angiography and AE in reducing mortality rates in these patients without data from a multivariate study and larger patient series. Even so, our mortality figures adjusted for severity in patients who undergo angiography and AE compare favorably with those from recent series.
In conclusion, in our series of patients with pelvic fracture associated with retroperitoneal hematoma, the performance of angiography has not varied depending on the time and day of admission, and the time until CE was short. There was good correlation between CE on CT and angiography.
Conflict of InterestsThe authors have no conflicts of interests to declare.
The authors would like to thank the General and Digestive Surgery Departments and the Interventional Radiology Unit for their collaboration in the data collection/processing and the development of this article.
Please cite this article as: Ciriano Hernández P, Moreno Hidalgo A, Grao Torrente I, Ruiz Moreno C, Seisdedos Rodrigez L, Kayser Mata S, et al. Fracturas de pelvis con hematoma retroperitoneal asociado: tiempo hasta la angioembolización y resultados. Cir Esp. 2019;97:261–267.