The thyroid gland initiates its embryological development after the third week of development, descending from the base of the tongue to the trachea, at the expense of the thyroglossal duct, foramen caecum and thyroid isthmus.1 In all these locations, there are reports of ectopic thyroid tissue remains, generally in the midline or paramedian plane of the neck; any distant implantation can be by tumour cells. We present a case, which we believe to be unique after a review of the literature, with the development of colloid cysts in the presternal subcutaneous tissue in a patient who had undergone 2 thyroid lobectomies 12 and 2 years earlier.
The patient is a 37-year-old woman who had undergone surgery in 2002 for right nodular goitre, involving a right lobectomy with isthmectomy; the histopathology results were benign. In 2009, she was diagnosed with a left thyroid nodule that was monitored with 3 fine-needle aspiration (FNA) biopsies that revealed a colloid goitre. Given the progressive growth of the nodule (from 18 to 35mm in 3 years), left lobectomy was indicated in 2012. In both cases, the surgeries were done using a standard technique, which entails the use of a lower skin flap up to the level of the sternal jugulum. The histopathology study revealed a thyroid with nodular hyperplasia with a 1.3mm intrathyroid solitary papillary microcarcinoma, no capsular invasion, disease-free margins and absence of lymphovascular and perineural infiltration.
After ruling out radioiodine ablation, suppressive therapy was initiated with Eutirox® at 125μg, which was later increased to 175μg. During this period, TSH remained under 0.01μg/mL and thyroglobulin under 5ng/mL.
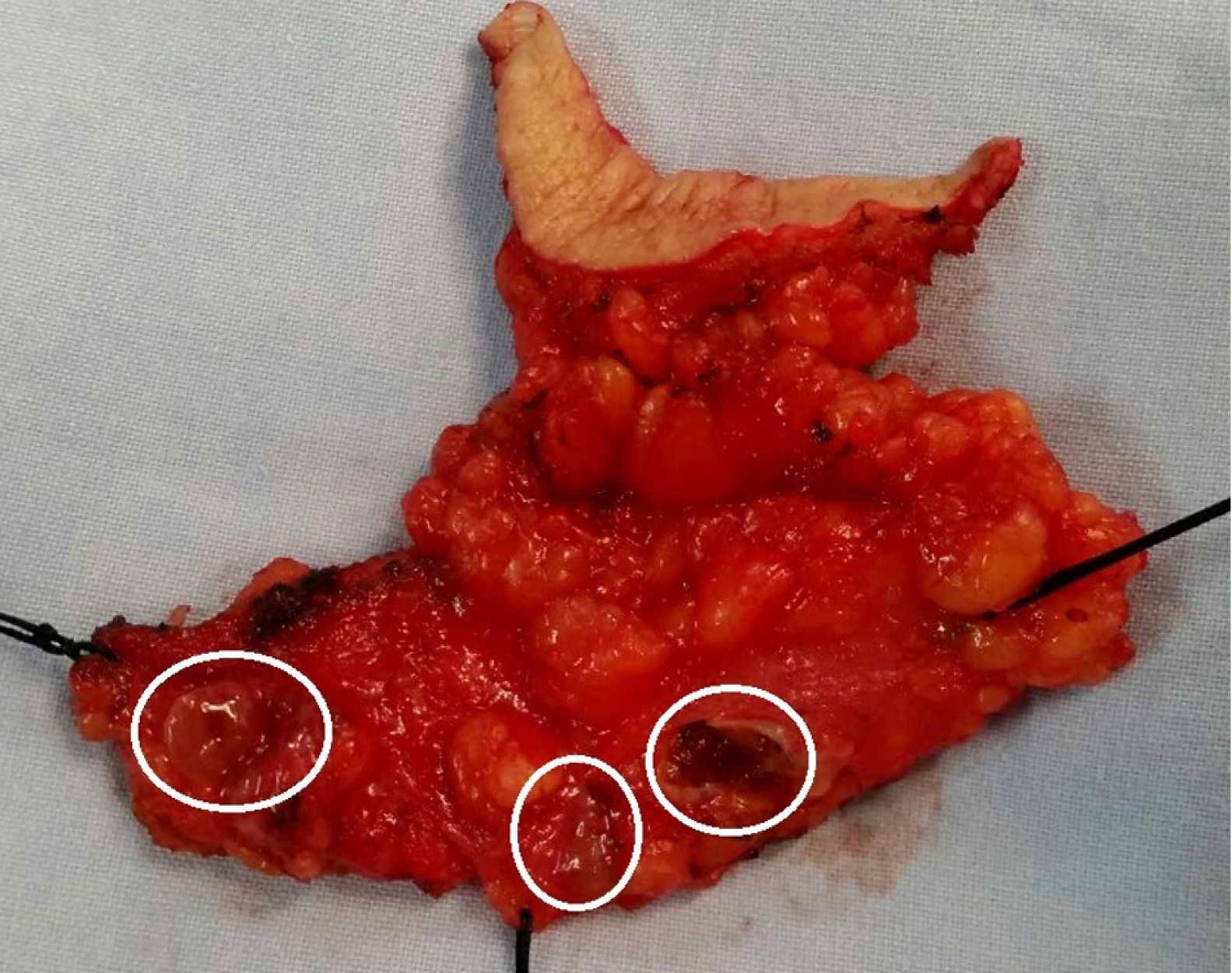
In April 2013, the patient developed symptoms of hyperthyroidism, and the Eutirox® dose was therefore lowered to 150μg. In June 2014, thyroglobulin showed a mild increase to 10ng/mL, at which time an I-131 scan detected high intensity radiotracer deposits close to the cervical scar that was interpreted as thyroid tissue. Upon physical examination, small mobile subcutaneous nodules were observed that were elastic in consistency. These nodules were located under the cervical scar and over the sternum, the largest of which was 1.5cm over the right sternoclavicular joint. The study was completed with ultrasound and cervical computed tomography, which confirmed the findings (Fig. 1). FNA biopsy of the nodule located next to the sternoclavicular joint identified thyroid colloid material. The patient underwent surgery in August 2014, and 3 colloid-looking nodules were identified in the locations described in the pre-op studies. En bloc excision was performed of the subcutaneous cell tissue of the area, including the previous scar (Fig. 2). The patient was discharged the following day without incident, and the histopathology study defined the nodules as thyroid parenchyma with no relevant histological lesions in the centre of subcutaneous cell tissue.
The appearance of thyroid tissue outside of the typical cervical distribution conditioned by its embryological development (base of the tongue, neck and mediastinum up to the diaphragm1,2) is exceptional and is almost always due to the implantation of tumour cells as a consequence of invasive procedures.3,4 In the case we present, this was our initial clinical impression given the finding of the micropapillary carcinoma in the second surgery. However, FNA that obtained colloid material ruled out that possibility. The definitive result of the pathology study, which classified them as colloid cysts, led us to believe that the subcutaneous cysts were the result of thyroid cells implanted in the lower skin flap during one of the 2 surgical interventions. The location of one of these cysts on the right sternoclavicular joint may have been due to the more extensive than usual dissection of a flap, and perhaps the implants were due to the rupture of a colloid cyst during surgery. These events, however, were not described in the surgical procedure.
FundingNo funding was received.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Colás Ruiz E, Quintáns Rodriguez A, Linacero Martin S, Celi Altamirano E, Martín Prieto L. Quistes coloides subcutáneos posquirúrgicos. Cir Esp. 2016;94:49–50.