Primary aortoenteric fistula (PAEF) is defined as an abnormal communication between the aorta and a segment of the gastrointestinal tract. It differs from secondary aortoenteric fistula, in which there is previous aortic surgery.1 Most PAEF occur in the duodenum (83%), mainly in the third and fourth portion, although it may occasionally occur in other segments of the gastrointestinal tract, such as the small intestine, colon or even appendix, although there are very few cases reported of this location in the literature.2
We present the case report of a kidney transplant recipient who developed a fistula between the donor renal artery (which presented aneurysmal dilatation) and the appendix, causing symptoms of abdominal pain and lower gastrointestinal bleeding that required emergency surgical intervention.
The patient was a 70-year-old male with a history of renal transplantation (1994) who came to our Emergency Department complaining of abdominal pain and fever for several hours. In the ER, he presented with symptoms of anal bleeding and hypovolemic shock, which responded to fluid therapy. Once the patient was stabilized, abdominal CT revealed the renal graft in the right liac fossa (RIF), and a lesion at the iliac bifurcation that seemed to correspond with a false aneurysm of the graft, measuring 3cm with gas in its interior. In the proximity, a probable loop of the small intestine or thickened appendix was visualized. The findings suggested an inflammatory process in the donor renal artery area, complicated with possible fistulization to a small intestinal loop or appendix.
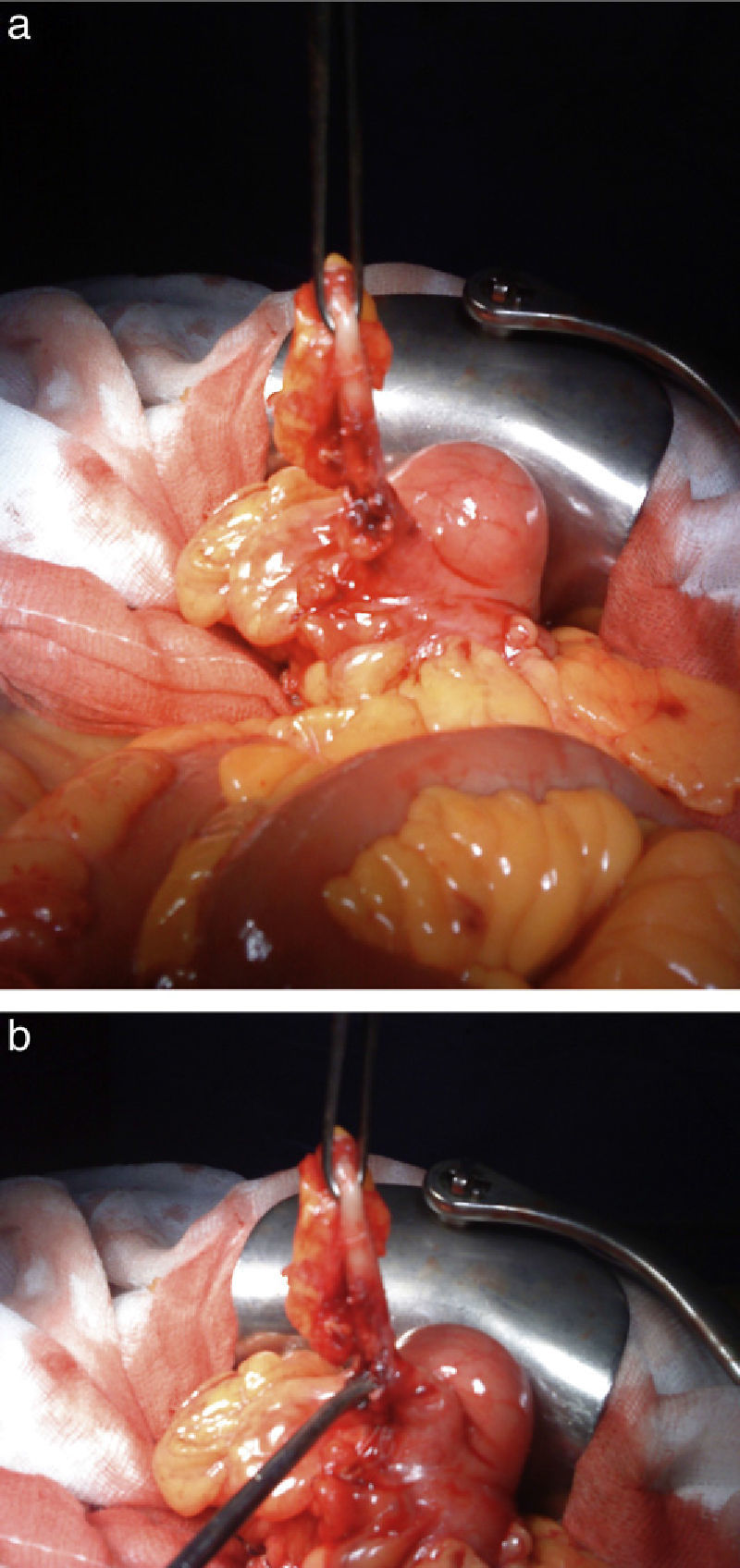
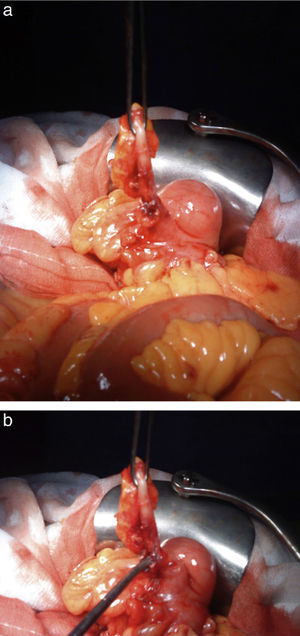
Angiography demonstrated a leak of contrast from the aneurysmal dilatation of the donor arterial anastomosis to the intestine. A covered prosthesis was positioned, excluding the aneurysm of the renal artery. Having resolved the arterial leak, a laparotomy was performed, revealing an inflammatory phlegmon in the right iliac fossa that encompassed the appendix with an orifice that corresponded with the appendix-graft fistula (Fig. 1a and b), and an appendectomy was performed. The patient had an uneventful postoperative course and was discharged on the 10th post-op day.
PAEF is defined as an abnormal communication between the aorta and a segment of the gastrointestinal tract, with no previous aortic surgery. It is a rare disease, with few cases published in the medical literature, and was first described in 1817.3,4 The main etiology is abdominal aortic aneurysm (AAA). Our patient developed an aneurysm, but in the donor renal artery. Other possible though very uncommon causes are septic aortitis, TBC, cancer or radiation.5
The diagnosis and treatment of PAEF is difficult, and only 33%–50% of cases are diagnosed preoperatively. In the series published, gastrointestinal bleeding is the most frequent symptom (61%–94%), followed by signs of infection (20%–30%) and symptoms of acute ischemia (20%–30%).6–8 Normally, the initial episodes of melenas or hematemesis resolve spontaneously, forming a kind of “sentinel bleeding” that tends to recur in periods of hours or days before the final massive bleeding. There is no diagnostic technique of choice; the combination of ultrasound and imaging tests (CT or MRI) can be a good option, although there are no published studies to support this. It is important to have a high index of suspicion based on the patient's medical history and physical examination for a correct diagnosis. It must be remembered that there are reports of mortality rates above 75% in cases of late diagnosis.9
In kidney transplants, vascular complications represent 5%–10% of all complications, especially renal artery and vein thrombosis (1.7%), renal stenosis (1.5%), lymphoceles (12%) and renal artery aneurysms. The latter is a very rare complication of renal transplantation that can lead to loss of the graft. Generally, these aneurysms are easily diagnosed by follow-up CT in kidney transplant recipients and Doppler ultrasound provides the differential diagnosis with hematomas, urinomas and lymphocele.10
Traditionally the technique of choice for treatment has been open surgery with repair of the aorta using a prosthesis (Dacron or PTFE) or extra-anatomical bypass. Endovascular procedures have increased in recent years, fundamentally in secondary aortoenteric fistulas, while in PAEF there are few cases described in the literature.11,12
The main complication of endovascular treatment is infection, although this also occurs in open surgery. On occasion, these patients present silent infections with no fever or leukocytosis. The probability of infection can be decreased if the local infection is eliminated first and the endovascular prosthesis is implanted later. These patients present high perioperative morbi-mortality. A recent review about PAEF concluded that around 2/3 of the patients died during surgery or in the first 30 days post-op.
In conclusion, we can state that endovascular treatment of primary aortoenteric fistula is an effective alternative to open surgery, especially in high-risk patients, but treating this type of patients requires adequate training and experience.
FundingFoundation grant, Hospital General in Elche, Spain.
Please cite this article as: Pérez-Legaz J, Marín-Hargreaves G, Ramírez M, Moya P, Arroyo A. Fistula reno-apendicular del injerto renal en paciente trasplantado: forma infrecuente de hemorragia digestiva baja. Cir Esp. 2013;91:397–399.