Between 35% and 55% of patients with colorectal cancer (CRC) may have recurrences of the disease. In cases of locoregional recurrence that receive medical treatment alone (chemotherapy and monoclonal antibodies), the average survival is 8 months, while the 5-year survival rate is less than 5%. In addition, these patients present a low quality of life and experience pain that is often difficult to control, depending on the location of the lesion.
The analysis of necropsies in patients with locoregional recurrence of CRC has demonstrated the absence of distant metastasis in 50% of cases1, so this group of patients could benefit from radical surgery2. The objective of the surgery is to obtain free surgical margins, or R0 resection. For oncologically correct margins, aggressive and sometimes multivisceral procedures may be necessary.
The R0 rate achieved with this type of procedure is considered higher than 50%, with a mortality rate lower than 2%, morbidity 55%, and 5-year survival between 25% and 46%3; therefore, surgical treatment could be considered the treatment of choice in this clinical situation.
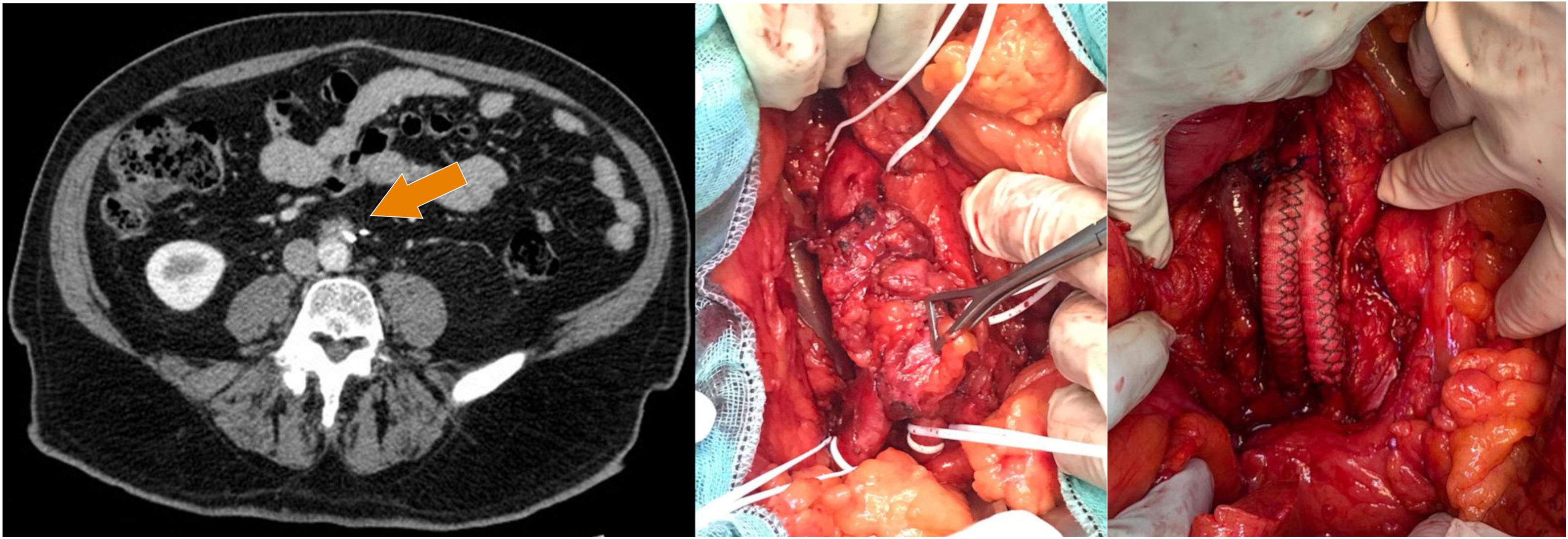
We present a case of locoregional recurrence of CRC with aortoiliac involvement. This 70-year-old male patient, who had no history of interest, had been treated with laparoscopic sigmoidectomy in 2017. The pathological analysis identified low-grade infiltrating adenocarcinoma, which was moderately differentiated (G2) and present in the adipose tissue and serosa, with perineural and angiolymphatic vascular invasion, high-grade tumor budding, and lymph node involvement (4/15) (stage pT4aN2a). The resection margins were free of tumor involvement. The patient was administered 8 cycles of XELOX adjuvant chemotherapy (capecitabine and oxaliplatin). During the 2-year follow-up, a CT scan detected a retroperitoneal lesion adjacent to the surgical clips of the inferior mesenteric artery, in contact with the anterior side of the infrarenal aorta, which we suspected to be local recurrence (Fig. 1). A PET/CT study showed hypermetabolic activity of the lesion suggestive of malignant disease, but no evidence of other lesions.
Given the diagnosis of a single lesion, the patient was considered a candidate for surgery with curative intent. Through a midline laparotomy, we accessed the infrarenal aorta and iliac arteries. A closely adhered tumor mass was observed, which affected more than 180° of the aorta surface, so we therefore decided to perform en bloc excision of the aorto-iliac segment next to the tumor. Subsequently, we conducted an end-to-end aorto-iliac bypass with a Dacron® stent (Fig. 1).
The anatomopathological analysis confirmed the diagnosis of recurrent adenocarcinoma of colorectal origin with invasion of the aortic wall (Fig. 2) and tumor-free resection margins.
There are few publications in the literature about the treatment of locoregional CRC recurrences with involvement of large vessels. We have only found isolated cases4–8 and a few short series. Abdelsattar et al.9 presented a series of 12 cases with different types of vascular involvement (7 internal iliac artery, 5 common iliac artery, 3 external iliac artery, 3 aorta, 2 internal iliac vein, 1 external iliac vein). In more than 50% of the cases, the authors achieved R0 resection, and 30-day mortality was 0. Four-year global survival and disease-free survival rates were 55% and 45%, respectively. Recently, Peacock et al.10 published a series of 11 patients with resections of the common iliac artery (4 cases), external and internal iliac arteries (3 cases), external iliac artery (2 cases), aorta and common iliac artery (one case). Eight cases had associated iliac vein resections. In one case, only venous resection was performed. The R0 resection rate was 82%, with a low rate of postoperative complications.
From the limited existing data, we can conclude that the involvement of large vessels in local CRC recurrences should not be a contraindication for surgery with curative intent, as R0 resection is possible in selected patients. Likewise, the overall survival and disease-free survival rates are comparable to those observed in cases of locoregional recurrence of CRC without vascular involvement.
FundingThe authors have received no funding for this study.
Please cite this article as: Vitiello G, Soto Carricas B, Martínez Sánchez MC, Targarona Soler E. Resección de la bifurcación aórtica en el tratamiento de la recidiva locorregional del cáncer colorrectal. Cir Esp. 2022;100:177–179.