Pelvic floor dyssynergia (PPD) is a common cause of outlet obstruction constipation. Treatment for this condition is based on pelvi-perineal re-education (PPR). The aim of this study was to evaluate the results of PPR on patients with PPD.
MethodsPatients with the diagnosis of PPD were included. The study was conducted between 2010 and 2011. PPR was performed by specialised kinesiologists. Prior and after treatment a constipation questionnaire was performed (KESS) (scale from 0 to 39 points, a higher score is associated with more symptom severity). KESS score before and after PPR were compared. Mann–Whitney–Wilcoxon rank sum test for paired samples was used for statistical analysis, P value <.05 was considered as significant.
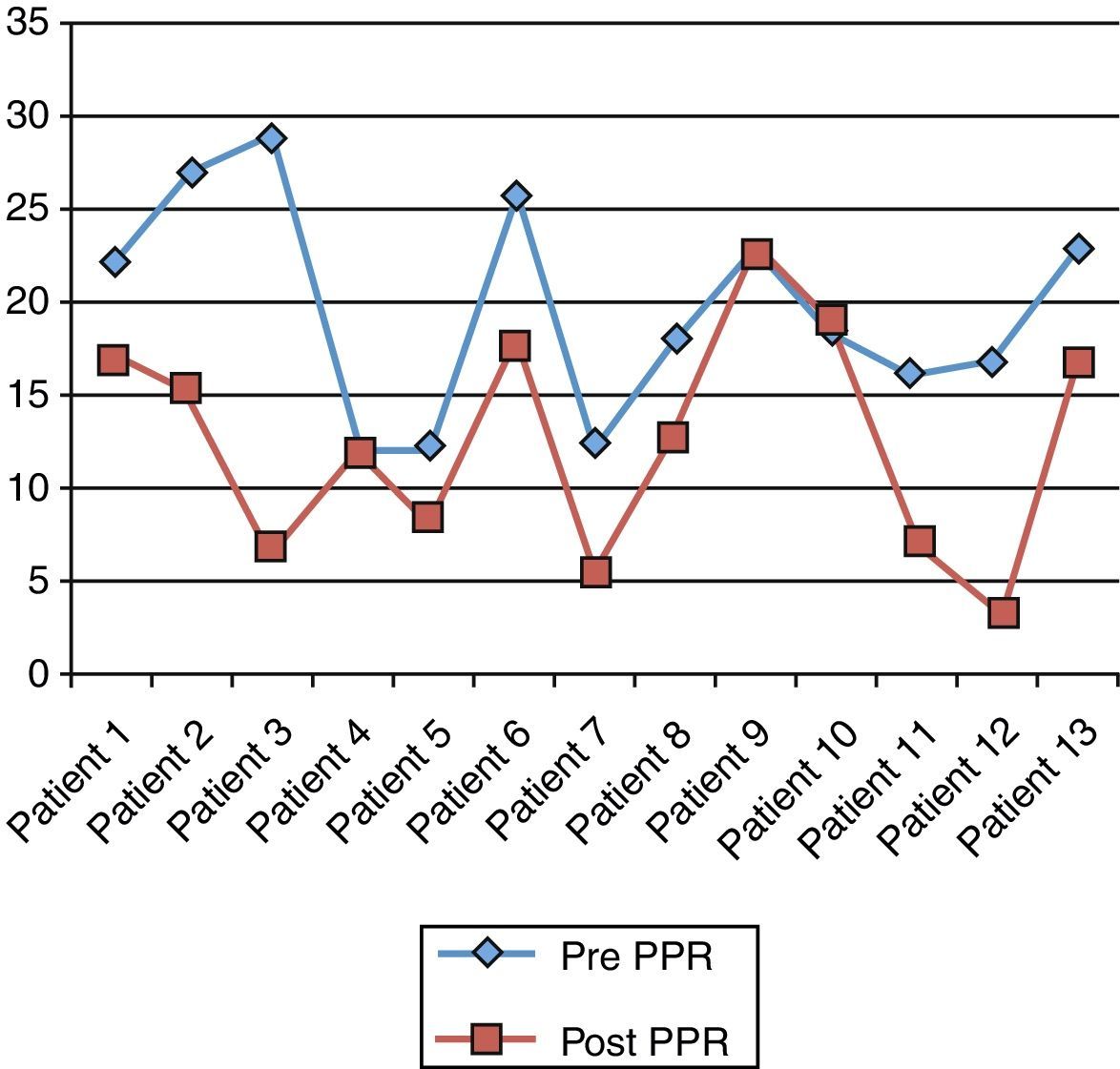
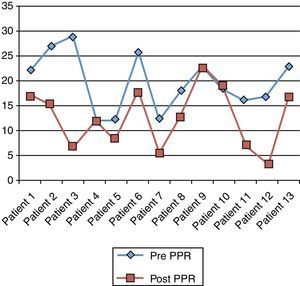
ResultsThirteen patients were included (11 women), and mean age was 44.3 years (range: 18–76). Mean total KESS score prior and after PPR were 19.6 (SD: 5.8) and 12.6 (SD: 6.3), respectively (P=.002).
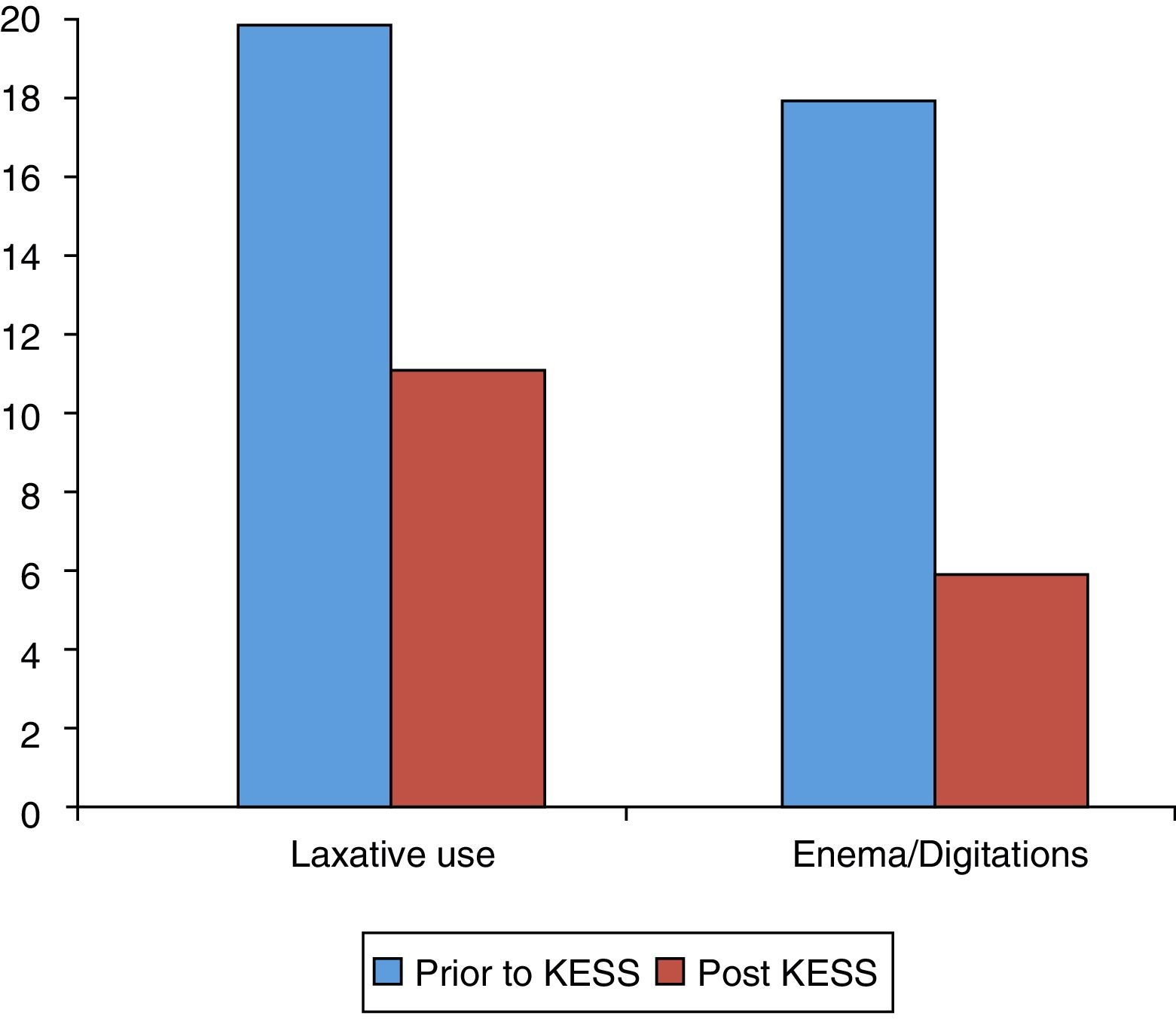
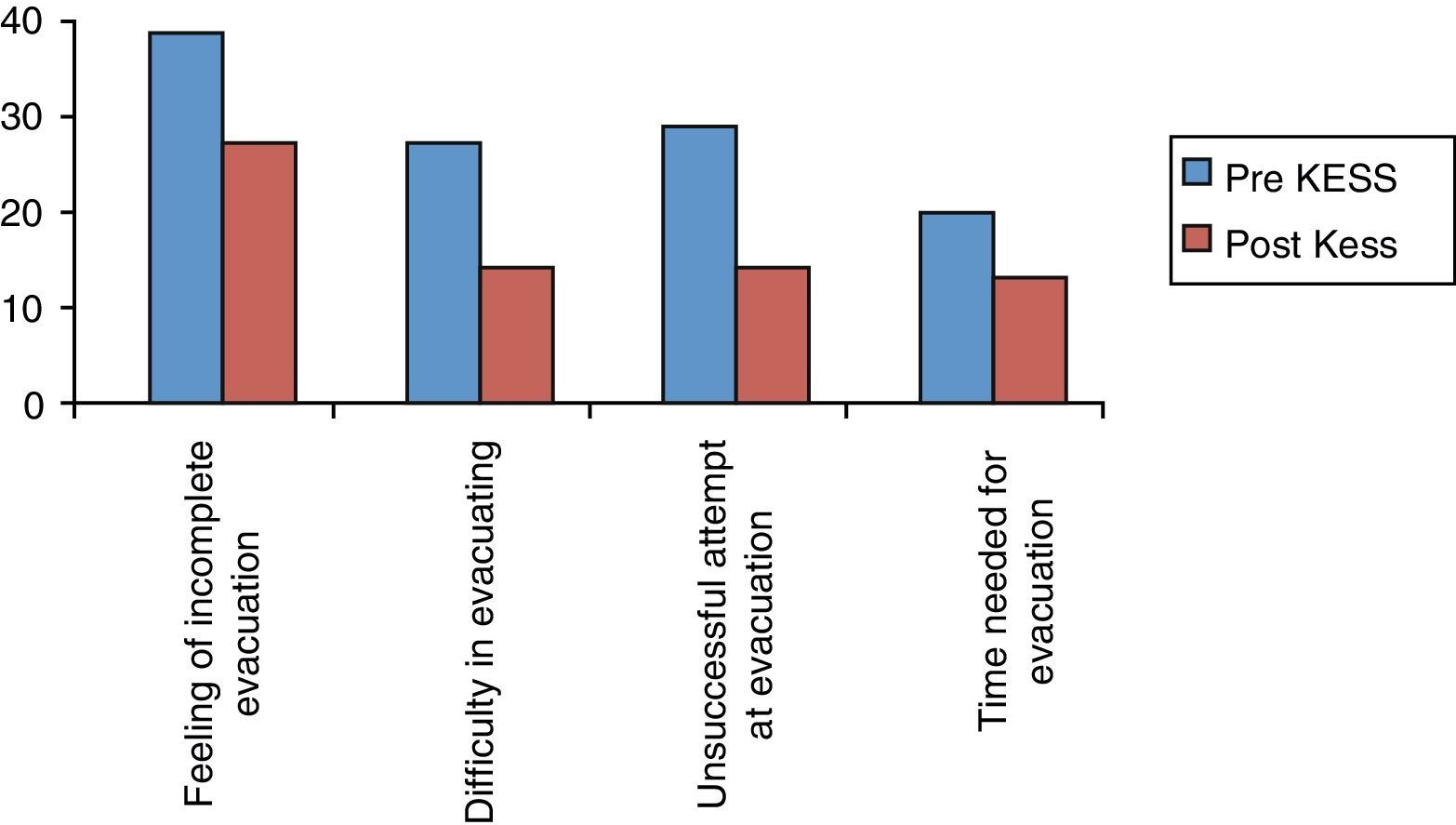
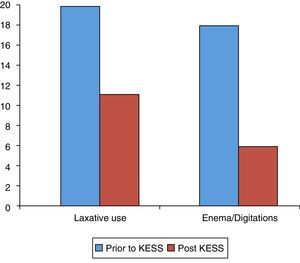
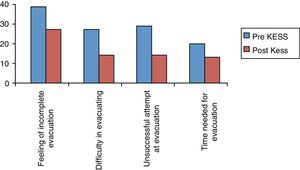
Frequency of bowel movements, stool consistency, abdominal pain, and abdominal bloating did not present statistically significant changes before and after treatment. Use of laxatives, enemas and/or digitations, as well as unsuccessful evacuation, feelings of incomplete evacuation improved significantly. Total evacuation time (before 1.53 vs after 1; P=.012) and difficult evacuation causing painful efforts (before 2.08 vs after 1.07; P=.001) also decreased significantly.
ConclusionPPR in patients with PPD significantly improves the symptoms of obstructive constipation, mainly with respect to mechanical assistance and difficult evacuation.
La disinergia del piso pelviano (DPP) es una causa frecuente de estreñimiento por obstrucción defecatoria. El tratamiento de esta enfermedad esta basado en la rehabilitación pelviperineal (RPP). El objetivo de este estudio es evaluar los resultados de la RPP en pacientes con DPP.
MétodosSe incluye a pacientes con DPP a quienes se les realizó RPP entre el año 2010 y el 2011. Se aplicó previamente a las sesiones y al término de ellas un cuestionario de estreñimiento (KESS) (escala de 0 a 39 puntos: a mayor puntuación mayor sintomatología). Se compararon los resultados del cuestionario KESS, de forma previa y posterior a la RPP. Análisis estadístico mediante Mann-Whitney-Wilcoxon para muestras pareadas; se consideró significativo p<0,05.
ResultadosSe incluyó a 13 pacientes (11 mujeres), edad promedio: 44,3 años (r: 18-76). La puntuación promedio del KESS previa y posterior al tratamiento fue de 19,6 (DE: 5,8) y de 12,6 puntos (DE: 6,3), respectivamente (p=0,002). La frecuencia evacuatoria, consistencia de las deposiciones, dolor abdominal y distensión abdominal no varían significativamente con el tratamiento. La necesidad del uso de enemas, laxantes o digitación, así como la evacuación no exitosa o incompleta disminuyeron en forma significativa. Asimismo, el tiempo total de evacuación (pre: 1,53 vs. post: 1; p=0,012) y la percepción de dificultad para evacuar (pre: 2,08 vs. post: 1,07; p=0,001) mejoraron significativamente.
ConclusionesLa RPP en pacientes con DPP mejora significativamente los síntomas de la obstrucción defecatoria, principalmente con relación a la asistencia mecánica y percepción de dificultad defecatoria.
Constipation is a common complaint. It is defined as a reduction in bowel movements, straining or an increased stool consistency,1 as currently defined by the ROMA III2 criteria.
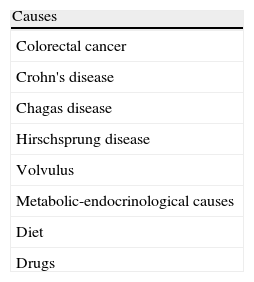
Most patients who present these symptoms will improve with medical treatment. Patients who do not respond to this treatment require an aetiological study and specific treatment. Secondary causes must be ruled out in this patient group. If symptoms and signs present which are suspicious of organic disease, a colonoscopy must be performed. Once secondary causes have been ruled out (Table 1), persistent chronic constipation is diagnosed. This may be divided into 4 groups: (a) slow transit constipation; (b) outlet obstruction; (c) functional GI disorder; (d) mixed disorder.
One of the most frequent aetiologies in the outlet obstruction group is pelvic floor dyssynergia.3 This consists of paradoxical contraction or non-relaxation of the pelvic muscles (most commonly the puborectalis muscle) during evacuation. Treatment of this disease is based on pelvi-perineal re-education (PPR).4 There are 3 essential aspects involved: muscular biofeedback, rectal biofeedback, and behavioural therapy/evacuation techniques. The aim of biofeedback is to correct abdominal, rectal, and pelvic floor dyssynergia and also improve rectal sensitivity.
Muscular biofeedback activity is measured by intracavitary electrodes. Muscular activity appears on a monitor which the patient observes. The images generate feedback for the patient based on their efforts. Rectal feedback consists of a technique aimed at improving rectal sensitivity and accommodation using an intrarectal ball which is filled until it provokes a need to evacuate, working on accommodation and sensitivity through gradual volumes. Behavioural therapy/evacuation techniques involve reinforcing correct evacuation technique, together with diaphragm exercises, abdominal muscle contraction, correct positioning of the legs and trunk during evacuation and monitoring fibre and liquid intake habits.
The aim of this study was to evaluate the short term results of PPR on patients with PPD in a consecutive series of patients at a specialised centre.
MethodsA prospective study protocol was undertaken by the members of the Centro de Especialidades de Piso Pelviano de Clínica Las Condes (CEPP-CLC) (Las Condes Clinic Pelvic Floor Specialist Centre). Patients presenting constipation that met the ROMA III criteria and with a clinical diagnosis of obstructive constipation were included in the study. Imaging was performed (conventional defaecography or magnetic resonance) to confirm and evaluate the aetiological diagnosis of obstructive constipation. PPD patients meeting the ROMA III criteria and whose diagnosis had been confirmed via dynamic imaging were included. This patient group was referred to PPR in the CEPP-CLC under the care of specialised kinesiologists. The PPR protocol consisted of muscular biofeedback, rectal biofeedback, pelvic floor muscle training, and behavioural therapy and evacuation techniques which were adapted to the needs of each patient.
The proposed treatment was for 12 sessions, with the following input:
- -
A preliminary evaluation.
- -
Ten sessions of kinetic work, initially two-weekly and subsequently once a week for periods of between 8 and 10 weeks.
- -
A final evaluation. This was made 30 days after the last treatment session.
A standardised and validated questionnaire on constipation (KESS)5,6 was completed prior to and on completion of the sessions to evaluate treatment results. The KESS consists of 11 questions, each with a Likert score scale of 0 to 3 or 0 to 4 points. Total score varies between 0 and 39 points: the higher the score the more severe the symptoms.
The questionnaire consists of a question about the duration of constipation, 4 questions regarding obstructive constipation symptoms, 2 regarding stool frequency and consistency, 2 regarding extraordinary methods used for evacuation and 2 regarding general gastrointestinal symptoms. All responses, except for constipation duration, were compared between the two stages.
Personal interviews during the first and last session took place with 2 kinesiologists from the CEPP-CLC team who conducted the questionnaire.
Question variables and total results score from the KESS questionnaire were compared prior and subsequent to PPR. Statistical analysis was performed using the Mann–Whitney–Wilcoxon method for paired samples. The significance value was P<.05. The values are expressed in median and interquartile (IQR) range, depending on distribution.
ResultsThe study period included 13 patients, 11 women (85%) and 2 men (15%), with mean age of 44.3 (range: 18–76). Eleven patients (85%) had their diagnosis confirmed by defaecography, and by magnetic resonance and 2 (15%) had their diagnosis confirmed by conventional defaecography. These patients received an average of 10 sessions during an 8–12-week period.
Regarding symptom duration, 69% of the patients presented symptoms for more than 5 years and of these, 33% had had symptoms for over 20 years. All patients had at least one bowel movement a week, the majority at least occasionally suffered from abdominal pain, abdominal bloating, and hard stools.
A significant reduction was observed regarding the total KESS score. Prior to treatment the median was 18 points (r.i: 16–23) and after treatment it was 13 points (r.i: 7–17; P=.002; Fig. 1).
A breakdown of the questionnaire findings revealed a tendency towards improvement with treatment with regard to frequency of evacuation (P=.34), stool consistency (P=.11), presence of abdominal pain (P=.12) and abdominal bloating (P=.13). Results were not, however, statistically significant.
A reduction in the use of laxatives was observed. Prior to treatment 62% of the patients made chronic use of laxatives compared with 31% after treatment. (P=.02). Furthermore, use of enemas or digitations fell from 69% to 23% after PPR (P=.009) (Fig. 2).
Eighty-five percent of the patients presented unsuccessful attempts at evacuation prior to PPR, which dropped to 38% (P=.003) after treatment. Thirty-one percent of the patients regularly or always suffered from painful straining on evacuation and this dropped to 8% after treatment (P=.001). Of the 77% patients who regularly had a feeling of incomplete evacuation, only half continued to have this feeling after treatment (P=.005). The percentage of patients requiring manual evacuation fell from 38% to 8%.
Finally, the time needed to evacuate decreased in the majority of patients (73%) from up to 30min prior to PPR, to 10min after treatment (P=.012) (Fig. 3).
DiscussionIn 1987, the first series of patients treated with biofeedback with positive results was published4 which determined the start of a series of studies in this regard. When we reviewed the literature, we observed that the terms used to define this entity are varied and the results obtained are fairly diverse,3,4 mainly due to a lack of uniformity in the diagnostic criteria regarding inclusion, treatment protocol, and treatment success definition.
The main value of this work is objective measurement (KESS) of the significant improvement of symptoms when a PPR regime was applied in a specialised centre in the short term follow-up of patients diagnosed with PPD.
Reference is made to biofeedback in the literature as treatment for PPD but kinetic treatment for patients in specialised centres not only just consist of biofeedback but also rectal muscle treatment, and a more complete therapy which includes evacuation technique reinforcement and the correction of bad habits. The most correct term to use would be pelvi-perineal “rehabilitation” or “re-education”.
Several studies have demonstrated efficacy in constipated adults of between 44% and 90%.3,7,8 However, many studies analyse a heterogeneous group of constipated patients who lack strict selection criteria which could explain the wide variability of success.
In our study we observed a significant reduction in most symptoms typically related to obstructive constipation, mainly the use of mechanical assistance and the perception of difficult evacuation. This concurs with the findings described in the literature.7,8
However, other general symptoms such as frequency and consistency of stools tended to improve, but not significantly. Several publications have described an improvement in the actual symptoms of obstructive constipation and in part in the general symptoms of frequency of bowel movements, abdominal bloating, and abdominal pain.9
This could probably be due to the fact that PPR is focused on correcting pelvic floor and rectum coordination, which is physiopathologically the problem in cases of obstructive constipation. However, obstructive constipation and slow transit disorders coexist in some patients.3 These patients present disorders of the pelvic floor and rectum, as well as the rest of the colon with motility and reflex disorders, which are not corrected by PPR.9
Although in this study only short term results were analysed, Battaglia et al.’s study shows the results from a year follow-up, with the observation that 50% of patients with PPD continued to maintain the beneficial effects of PPR after completion of follow-up.9
In order to obtain an improvement of general symptoms in these patients, alternative treatments to PPR have been suggested, such as the use of polyethylene glycol and educational sessions. In a comparative study, between PPR and the administration of polyethylene glycol together with educational sessions, an increase in bowel movement frequency occurred in both groups. However, PPR improved the sensation of incomplete evacuation, use of enemas, and suppositories, as well as the episodes of abdominal pain.10
In the study carried out by Heymen et al., two groups were compared with the application of PPR (electromyography feedback), diazepam, and placebo in patients previously doing exercises which involved the pelvic floor muscles. This study showed that only the group which applied electromyographic feedback showed any improvement of symptoms related to constipation after 3 months follow-up.11
Regarding the advantages of PPR, we must note that it is well tolerated by patients because, in general, no adverse effects regarding its application have been described. In our series there were no problems in relation to its administration. One of the limitations of this type of treatment is that it is only offered in a few centres on a national level and is therefore a form of treatment which is currently restricted to reference centres.
The study's major limitations were the low patient number and short term follow-up.
To conclude, in this study, PPR in PPD patients significantly improved the symptoms of obstructive constipation in short term follow-up.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Wainstein C, Carrillo K, Zarate AJ, Fuentes B, Venegas M, Quera R, et al. Resultados de la rehabilitación pelviperineal en pacientes con disinergia del suelo pélvico. Cir Esp. 2014;92:95–99.