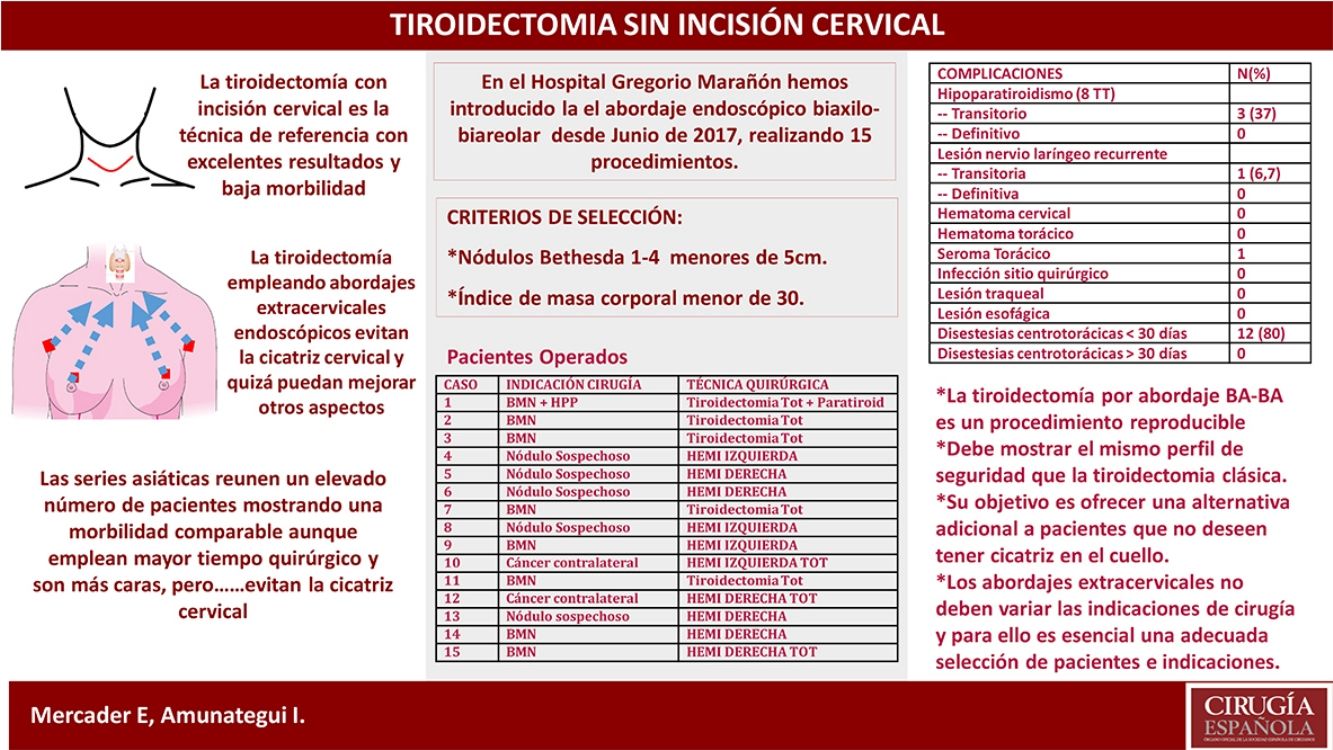
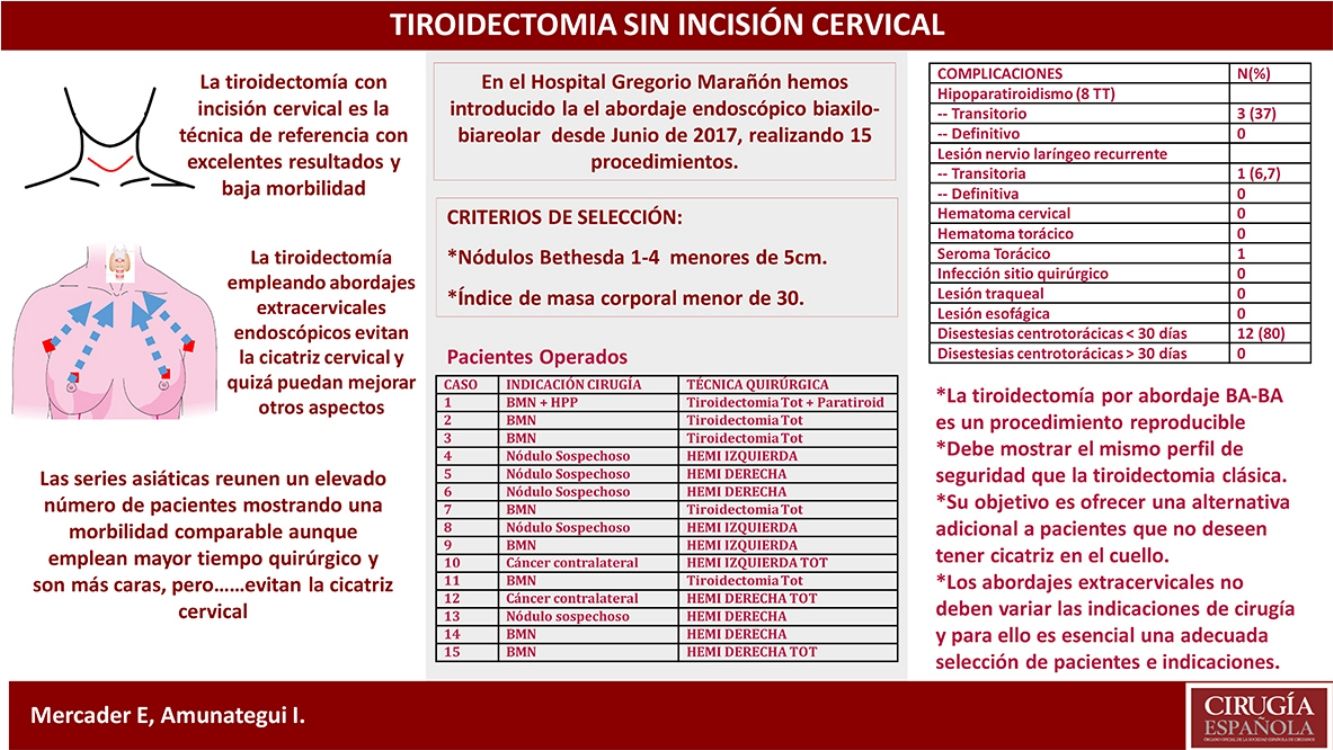
The extracervical approach for thyroidectomy remains widely unknown in our country. Its main aim is to avoid a cervical scar while maintaining the same safety profile of conventional thyroidectomy. The objective is to communicate our experience after the first 15 cases using the endoscopic bilateral axillo-breast approach (BABA) and to review critical points described in literature.
MethodsBetween June 2017 and June 2018, 15 endoscopic thyroidectomies were performed using the BABA extracervical approach, locating incisions in axillary folds and areolar borders. Indications were benign goiter and suspicious nodule (Bethesda 3 and 4).
ResultsAll 15 cases (12 patients) were treated using the extracervical endoscopic technique. We performed 5 total thyroidectomies, 7 hemithyroidectomies and 3 completion thyroidectomies. Mean surgical time for total thyroidectomy was 285min and 210min for hemithyroidectomy. The average hospital stay was 1.67 days. With a mean follow-up of 7.73 months, rates of transient and definitive hypoparathyroidism were 37% and 0%, and transient recurrent nerve palsy occurred in one case. Anterior chest paraesthesia rate was 80%, which were mild and resolved within the first month. The degree of cosmetic satisfaction is very high.
ConclusionOur experience with endoscopic bilateral axillo-breast approach thyroidectomy is short but satisfactory. It is a reproducible procedure that requires extensive experience in endocrine and endoscopic surgery. Extracervical approaches are an alternative for selected patients who are especially concerned about cervical scarring and are not intended to displace conventional thyroidectomy, which is the current gold standard. Our Scientific Society should explore these approaches to establish coherent indications and limitations.
El abordaje extracervical para tiroidectomía es poco conocido en nuestro país. Su principal fin es evitar la cicatriz cervical, manteniendo el perfil de seguridad de la tiroidectomía convencional. El objetivo es comunicar nuestra experiencia tras los primeros 15 casos empleando el abordaje endoscópico biaxilo-biareolar (BA-BA) así como revisar los puntos críticos descritos en la literatura.
MétodosEntre junio de 2017 y junio de 2018 se realizaron 15 tiroidectomías endoscópicas empleando abordaje extracervical BA-BA, ubicando incisiones en pliegues axilares y bordes areolares. Las indicaciones fueron bocio benigno y nódulo sospechoso (Bethesda 3/4).
ResultadosLos 15 casos (12 pacientes) se abordaron completamente por BA-BA. Se realizaron 5 tiroidectomías totales, 7 hemitiroidectomías y 3 totalizaciones. El tiempo quirúrgico medio para tiroidectomía total fue de 285min y para hemitiroidectomía, de 210min. El tiempo medio de ingreso fue de 1,67 días. Con un seguimiento medio de 7,73 meses, la tasas de hipoparatiroidismo transitorio y definitivo fueron del 37% y del 0% y se produjo parálisis recurrencial transitoria en un caso. Tasa de disestesias centrotorácicas del 80%, leves y resueltas en el primer mes. El grado de satisfacción cosmética es muy elevado.
ConclusiónNuestra experiencia empleando el abordaje BA-BA es corta pero satisfactoria. Es un procedimiento reproducible que requiere experiencia en cirugía endocrina y endoscópica. Los abordajes extracervicales son una alternativa para pacientes seleccionados con especial preocupación por la cicatriz cervical y no pretenden desplazar a la tiroidectomía convencional, el gold estandard actual. Nuestra sociedad científica debe explorar estos abordajes para sentar indicaciones y limitaciones coherentes.
Remote access thyroidectomy procedures aimed at avoiding cervical scars after thyroidectomy have recently appeared on the scene of Spanish endocrine surgery. These techniques first appeared in Asia, where cervical scars have a deleterious social impact.1–4
Although direct cervical endoscopic approaches have previously been developed in Europe, such as the video-assisted thyroidectomy by Miccoli,5–8 conventional thyroidectomy (ConT) remains the gold standard, with very low morbidity rates and whose only permanent sequela is the visible cervical scar.
Today, the role of extracervical endoscopic approaches (bilateral axillo-areolar, transoral with vestibular or transaxillary approach) in our setting has yet to be defined. Their clearest advantage is the avoidance of cervical scars, an issue that concerns our patients, although it has yet to be resolved whether this technique provides other advantages.
The implementation of these approaches requires an experience in endocrine and laparoscopic surgery. At the very least, these techniques should be required to meet the safety profile of ConT.9–12
Our unit decided to explore these procedures by selecting a safe, reproducible and economically feasible approach: the endoscopic bilateral axillo-breast approach (BABA). The use of this technique is widespread in Asia, and series with large patient groups have reported excellent results.10,11
The aim of this article is to communicate our first impressions after the implementation of the BABA endoscopic approach, as well as to compare certain key points with reports by experienced authors.
MethodsWe designed a descriptive study based on prospectively collected data from a cohort of 15 cases with thyroid pathology who underwent partial or total thyroidectomy (TT) between June 2017 and June 2018 by the endoscopic BABA approach.
The entire cohort was diagnosed following the standard protocol of our unit: ultrasound with FNA of the dominant or most suspicious nodule in accordance with the ACR TI-RADS calculator and the Bethesda system.13,14
The selection criteria to indicate the BABA approach were: (1) Bethesda 1–4 nodules measuring less than 5cm; and (2) body mass index (BMI) <30. Excluded from the study were patients with oncological diagnosis, Graves Basedow's disease and patients with previous open surgery. Sex and age were not conditioning factors, nor was the coexistence of parathyroid pathology.
Patients who met the requirements for this approach gave their signed informed consent.
Demographic and diagnostic data were collected, as were data for surgical variables, including: technique, operative time, data related to nerve monitoring, number of visualized parathyroid glands and technical complications. Postoperative variables included: rate of hypoparathyroidism and recurrent paralysis, postoperative hematoma and the need for reoperation, central thoracic dysesthesia and infectious complications. Likewise, definitive anatomic pathology results and the need for re-admission were recorded.
Statistical StudyThe SPSS program v21 (IBM, SPSS, Chicago, IL, USA) was used to calculate descriptive statistics: median±range.
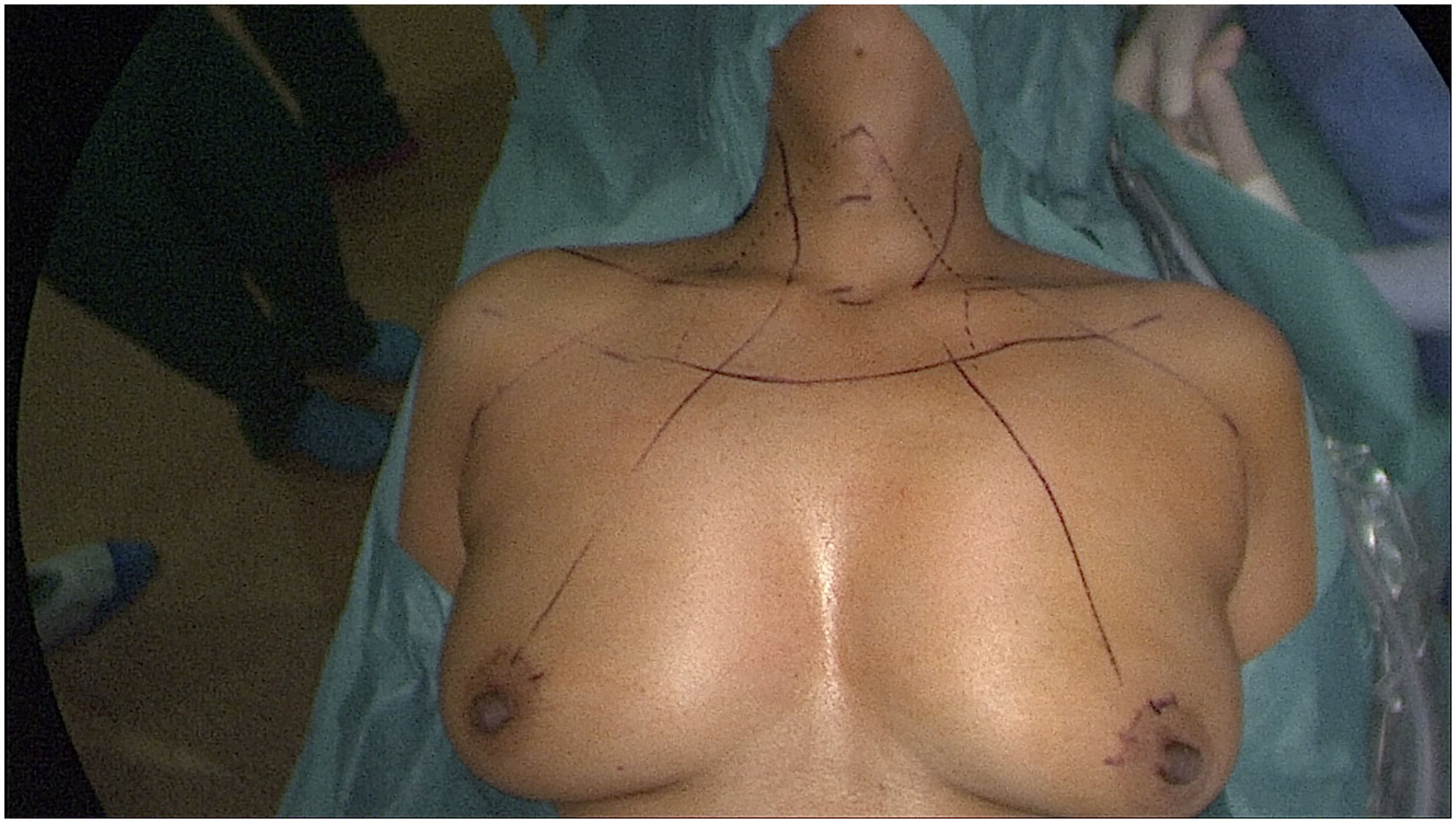
Description of the ProcedureUnder general anesthesia, the patient is placed in the supine position. A TriVantage™ endotracheal tube for nerve monitoring (Medtronic, Jacksonville, USA) is used and the main anatomical references are marked (Fig. 1). An adrenaline solution is injected in the future subcutaneous pathways. For both TT and hemithyroidectomy, 4 trocars are placed: two 5mm trocars in the axillae and two 10–11mm on the edge of the areolae.
With blunt dissection, subcutaneous tunnels are created that converge at the suprasternal notch, and CO2 is insufflated at 7mmHg. Under endoscopic vision, the subplatysmal space is dissected to the thyroid cartilage. When there is enough working space, the surgery proceeds in a manner similar to conventional thyroidectomy, dividing the isthmus first and proceeding medial to lateral, caudal to cranial. Neuromonitoring is routinely used (NIM® 3.0 system Medtronic, Jacksonville, USA), following international protocols for intermittent monitoring.15 Due to its high negative predictive value, an absolute value of V2 >200μV was considered a safety criterion. With a potential less than 100μV after lobectomy, the procedure is completed, in case of TT, given the risk of possible recurrent paralysis.16
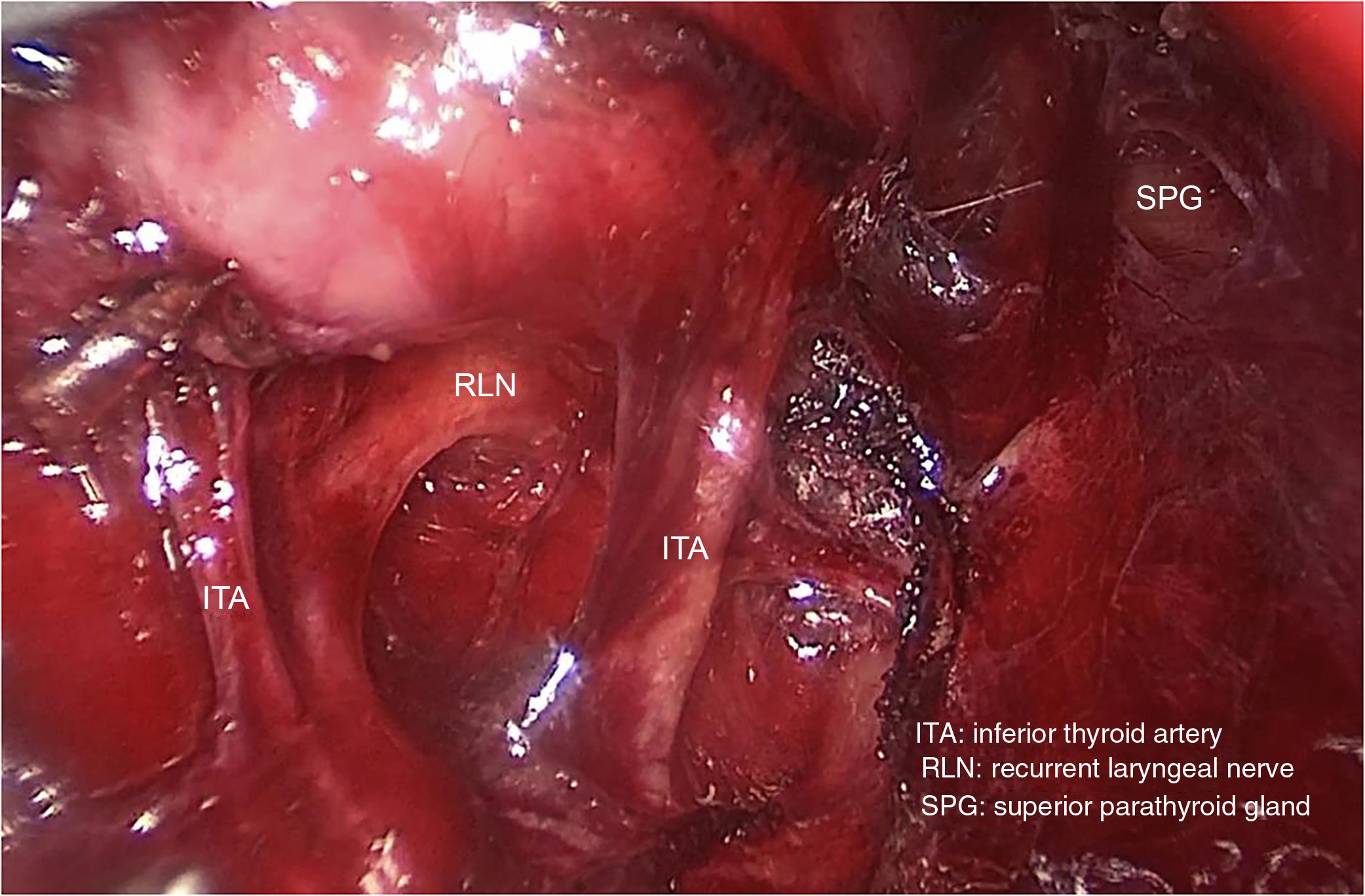
During dissection, the parathyroid glands, RLN and EBSLN are identified and avoided. Finally, 20cc of 0.25% bupivacaine are administered in the subplatysmal space. Drains are not used, and a compression bandage is applied over the flap.
Oral tolerance and ambulation are initiated 6h later. All cases are managed with analgesia based on NSAIDs. Depending on pain control and calcemia, the patients are discharged 24–48h later. It is recommended to keep the dressing on the flap for 3 days to favor skin/fascia adhesion.
ResultsBetween June 2017 and June 2018, 15 thyroidectomies were performed on 12 patients using the BABA endoscopic approach.
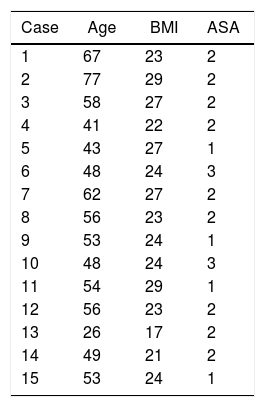
All the patients were women with a mean age of 52 and a mean BMI of 24.69kg/m2 (Table 1).
Demographic Data of the Series.
| Case | Age | BMI | ASA |
|---|---|---|---|
| 1 | 67 | 23 | 2 |
| 2 | 77 | 29 | 2 |
| 3 | 58 | 27 | 2 |
| 4 | 41 | 22 | 2 |
| 5 | 43 | 27 | 1 |
| 6 | 48 | 24 | 3 |
| 7 | 62 | 27 | 2 |
| 8 | 56 | 23 | 2 |
| 9 | 53 | 24 | 1 |
| 10 | 48 | 24 | 3 |
| 11 | 54 | 29 | 1 |
| 12 | 56 | 23 | 2 |
| 13 | 26 | 17 | 2 |
| 14 | 49 | 21 | 2 |
| 15 | 53 | 24 | 1 |
ASA: assessment of anesthetic risk according to the American Society of Anesthesiologists score; BMI: body mass index.
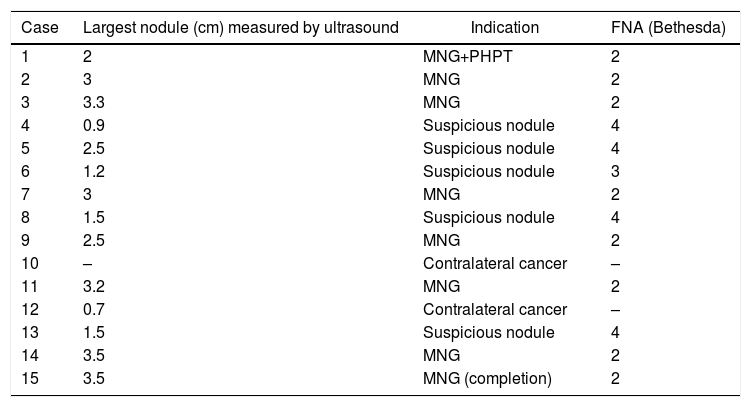
The most frequent indication for surgery was benign nodular pathology (7 cases), one of which presented associated localized hypercalcemic primary hyperparathyroidism. The second most frequent indication was a suspicious thyroid nodule (Bethesda 3/4) (5 cases). Three completion hemithyroidectomies were performed: 2 due to differentiated contralateral cancer and deferred thyroidectomy in a case of bilateral MNG due to intraoperative signal loss. The measurements of the dominant nodules, FNA results and diagnoses are shown in Table 2.
Preoperative Thyroid Pathology Data.
| Case | Largest nodule (cm) measured by ultrasound | Indication | FNA (Bethesda) |
|---|---|---|---|
| 1 | 2 | MNG+PHPT | 2 |
| 2 | 3 | MNG | 2 |
| 3 | 3.3 | MNG | 2 |
| 4 | 0.9 | Suspicious nodule | 4 |
| 5 | 2.5 | Suspicious nodule | 4 |
| 6 | 1.2 | Suspicious nodule | 3 |
| 7 | 3 | MNG | 2 |
| 8 | 1.5 | Suspicious nodule | 4 |
| 9 | 2.5 | MNG | 2 |
| 10 | – | Contralateral cancer | – |
| 11 | 3.2 | MNG | 2 |
| 12 | 0.7 | Contralateral cancer | – |
| 13 | 1.5 | Suspicious nodule | 4 |
| 14 | 3.5 | MNG | 2 |
| 15 | 3.5 | MNG (completion) | 2 |
MNG: multinodular goiter; PHPT: primary hyperparathyroidism; FNA: fine-needle aspiration.
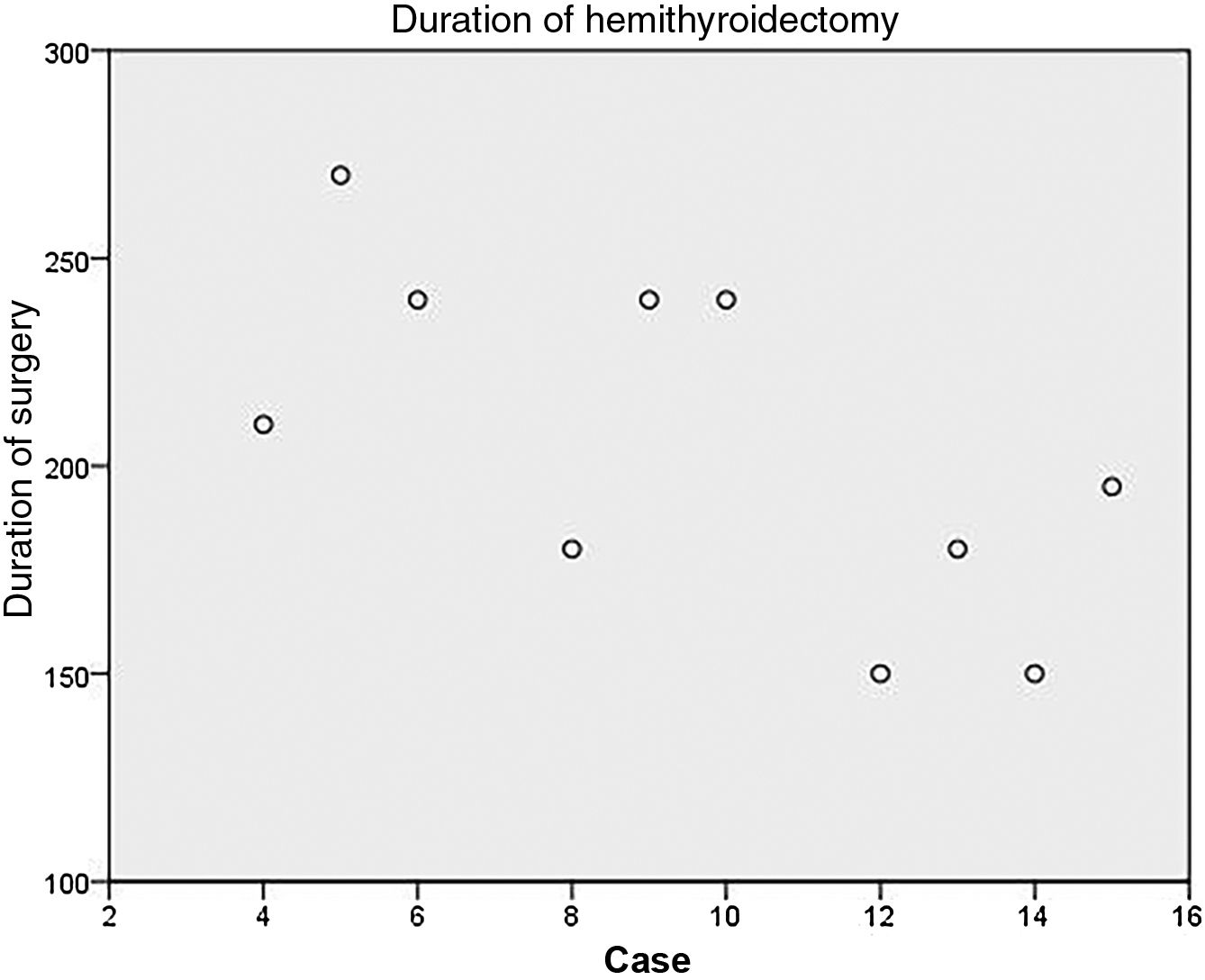
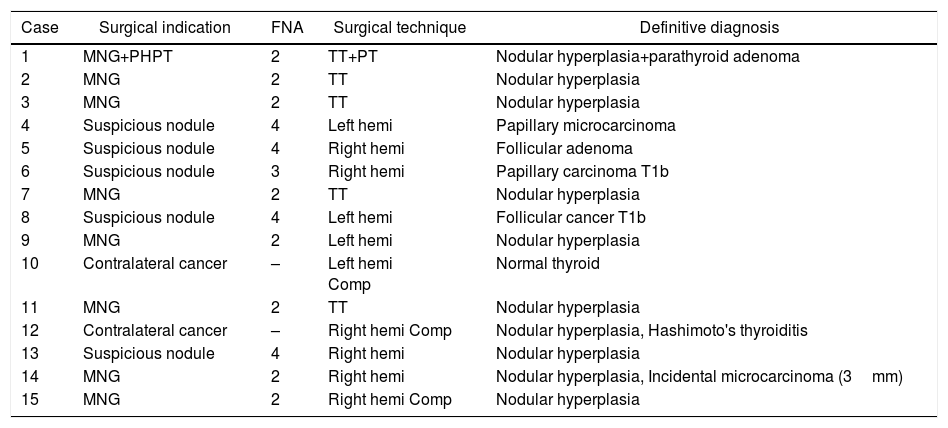
The techniques are described in Table 3. Patient number 1 underwent associated left upper parathyroidectomy. The mean duration of TT was 285min (270–300min), extended hemithyroidectomy 210min (150–270min) and that of completion hemithyroidectomy 195min (150–240min).
Summary of Preoperative Data, Surgical Technique Used and Definitive Diagnosis.
| Case | Surgical indication | FNA | Surgical technique | Definitive diagnosis |
|---|---|---|---|---|
| 1 | MNG+PHPT | 2 | TT+PT | Nodular hyperplasia+parathyroid adenoma |
| 2 | MNG | 2 | TT | Nodular hyperplasia |
| 3 | MNG | 2 | TT | Nodular hyperplasia |
| 4 | Suspicious nodule | 4 | Left hemi | Papillary microcarcinoma |
| 5 | Suspicious nodule | 4 | Right hemi | Follicular adenoma |
| 6 | Suspicious nodule | 3 | Right hemi | Papillary carcinoma T1b |
| 7 | MNG | 2 | TT | Nodular hyperplasia |
| 8 | Suspicious nodule | 4 | Left hemi | Follicular cancer T1b |
| 9 | MNG | 2 | Left hemi | Nodular hyperplasia |
| 10 | Contralateral cancer | – | Left hemi Comp | Normal thyroid |
| 11 | MNG | 2 | TT | Nodular hyperplasia |
| 12 | Contralateral cancer | – | Right hemi Comp | Nodular hyperplasia, Hashimoto's thyroiditis |
| 13 | Suspicious nodule | 4 | Right hemi | Nodular hyperplasia |
| 14 | MNG | 2 | Right hemi | Nodular hyperplasia, Incidental microcarcinoma (3mm) |
| 15 | MNG | 2 | Right hemi Comp | Nodular hyperplasia |
MNG: multinodular goiter; Hemi: hemithyroidectomy; PHPT: primary hyperparathyroidism; FNA: fine-needle aspiration; PT: parathyroidectomy; Comp: completion thyroidectomy; TT: total thyroidectomy.
No conversion to open surgery was required in any case. There were also no major hemorrhagic complications. Anatomic pathology data are shown in Table 3.
The mean hospital stay was 1.67 days (1–3 days). Although a specific pain assessment scale was not used, information from drug administration records did not differ from the usual amount administered in conventional thyroidectomy. No narcotic pain medication was necessary.
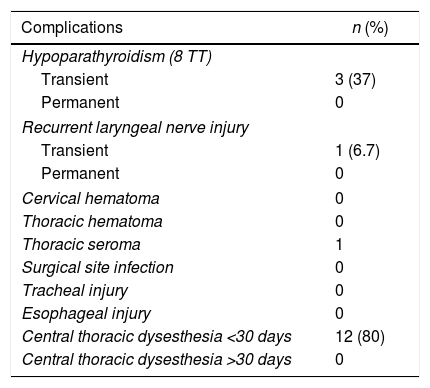
With a mean follow-up time of 7.73 months (2–14 months), postoperative morbidity is shown in Table 4.
Complications of the BABA Approach.
| Complications | n (%) |
|---|---|
| Hypoparathyroidism (8 TT) | |
| Transient | 3 (37) |
| Permanent | 0 |
| Recurrent laryngeal nerve injury | |
| Transient | 1 (6.7) |
| Permanent | 0 |
| Cervical hematoma | 0 |
| Thoracic hematoma | 0 |
| Thoracic seroma | 1 |
| Surgical site infection | 0 |
| Tracheal injury | 0 |
| Esophageal injury | 0 |
| Central thoracic dysesthesia <30 days | 12 (80) |
| Central thoracic dysesthesia >30 days | 0 |
TT: total thyroidectomy.
Complications related to the approach included: (a) clinically significant seroma in a patient that spontaneously reabsorbed in the first 2 weeks; and (b) 12 of the 15 patients (80%) presented central thoracic dysesthesias, all of which —except one—were mild in nature, did not require pharmacological treatment or only low doses of NSAIDs. The duration did not exceed 3 weeks, except in the aforementioned case, which presented significant hyperesthesia for almost 4 weeks.
There were no cases of cervical hematoma or reoperations. In addition, no cases of superficial or deep infection were observed. We detected no complications associated with the use of gas. There were no readmissions. Although a specific patient satisfaction survey was not used, the subjective perception of the surgical team when interviewing patients during follow-up is that all of them were very satisfied and would recommend this procedure.
DiscussionToday, ConT is the gold standard technique for thyroid disease, with a mortality of 0.065% and a low rate of complications in specialized units.17
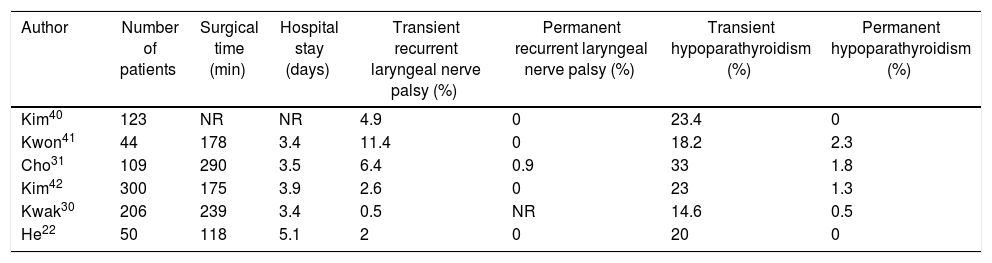
The only permanent sequela after this procedure is the cervical scar. This has led to extracervical approaches being developed in Asian countries, where extensive experience has shown favorable results, especially with the robotic version of this technique (Table 5).
Asian Experience With the BABA Approach.
| Author | Number of patients | Surgical time (min) | Hospital stay (days) | Transient recurrent laryngeal nerve palsy (%) | Permanent recurrent laryngeal nerve palsy (%) | Transient hypoparathyroidism (%) | Permanent hypoparathyroidism (%) |
|---|---|---|---|---|---|---|---|
| Kim40 | 123 | NR | NR | 4.9 | 0 | 23.4 | 0 |
| Kwon41 | 44 | 178 | 3.4 | 11.4 | 0 | 18.2 | 2.3 |
| Cho31 | 109 | 290 | 3.5 | 6.4 | 0.9 | 33 | 1.8 |
| Kim42 | 300 | 175 | 3.9 | 2.6 | 0 | 23 | 1.3 |
| Kwak30 | 206 | 239 | 3.4 | 0.5 | NR | 14.6 | 0.5 |
| He22 | 50 | 118 | 5.1 | 2 | 0 | 20 | 0 |
This is the first characteristic to highlight: these are not new techniques, but new approaches. The BABA approach requires acquiring new knowledge for the creation of subcutaneous tunnels to access the thyroid, but once the work space is created, the technique is very similar to ConT. The anatomic view is familiar; therefore, it is a reproducible technique that allows surgeons to apply their experience in thyroid surgery. Although the location of the trocars provides adequate triangulation, endoscopic maneuverability will be the main difficulty we encounter, so a good background in endoscopic surgery is necessary.
Adequate patient selection is essential during the learning curve. In no case should the approach condition the indication or technique. Therefore, foreseeable difficulties should be avoided, such as those associated with obese patients, Graves-Basedow disease and pathologies with preoperative oncological diagnosis due to the possibility of associated central lymphadenectomy, a procedure that is not accessible during the learning curve. We included 5 patients with suspicious lesions (Bethesda 3/4), whose indication was diagnostic thyroidectomy, and if completion was required, this was able to be done with the same approach. Completion procedures were necessary in 2 patients with differentiated cancers. In case number 4, no completion was performed, in accordance with consensus guidelines.18 In addition, one patient (number 9) had a type 1 loss of signal during the initial lobectomy that was not recovered, so the contralateral thyroidectomy was postponed. This patient presented vocal cord paresis for 30 days and had a subsequent completion procedure (case 15). The reoperations were performed by the BABA approach after a 3-month wait, and we have not observed any special technical difficulties.
The oncological indication is not a contraindication at hospitals with experience, and there are Korean series with more than one thousand patients. They are limited to low risk papillary cancer measuring less than 4cm, with or without lymphadenectomy. The suspicion of RLN or visceral invasion are contraindications. The results do not seem to find differences in complete resection, and there are still no series with a sufficiently long follow-up, although Chai does not find significant differences in recurrence after 40.2 months in papillary thyroid carcinomas measuring 3–4cm.19–22
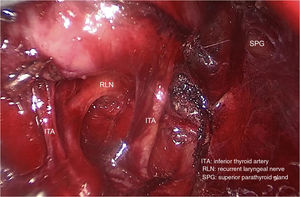
Conventional laparoscopic surgery material with 4K imaging systems provides excellent image quality (Fig. 2). We have systematically used intermittent nerve monitoring adapted to endoscopic devices. The systematic review by Diogini about neuromonitoring in endoscopic surgery reported that only 30% monitor the vagus and 25% the EBSLN.23 In our experience, dissection of the vascular bundle and vagus nerve monitoring are not an added difficulty.
We have also observed no subcutaneous emphysema or anesthetic complications related to the administration of subcutaneous CO2, such as hypercapnia, pneumothorax or hemodynamic disorders,24 although it is true that we work with low CO2 pressures (6–7mmHg) as a preventive measure, as recommended by Ochiai et al.25
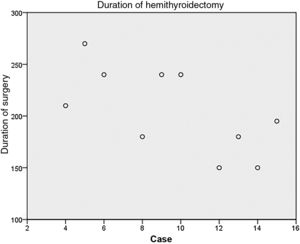
The surgical time is much longer and statistically significant in all the studies, from 1.5 to 2 times longer than ConT. In the series by Kim, the operative time for ConT was 82min, compared to 130min for an endoscopic BABA and 190min for the robotic technique. Even in hospitals with experience, these times have not been reduced, and future reductions seem unlikely.11,19,26,27 In our series, the TT time was 2.5 times longer than ConT (285min vs 105min), similar to hemithyroidectomy, and they are much higher than those of referral hospitals. Operative times are expected to start falling after 35–0 cases. However, in hemithyroidectomies, we have already observed a decreasing trend (Fig. 3).
We instilled the area of the subcutaneous flap with a local anesthetic. The effect of this maneuver improves pain control and the consumption of postoperative analgesics the first 48h after the intervention, in keeping with the study by Lee.28,29
We have not had cases of reoperation for hematoma related to asphyxia. The Korean series do not describe an increase in the incidence of postoperative hematoma, but given the greater dissection space where blood can accumulate, very active monitoring is necessary.19,26,30
In the immediate or deferred postoperative evaluation, several points are of interest:
- -
Postoperative pain was adequately controlled with NSAIDs. Some studies have even suggested a lower consumption of analgesics in the BABA approach, but our findings generally coincide with most of the literature.22,31
- -
Our mean hospital stay was 1.67 days, which is no different than in ConT. In Asian series, the hospitalization time is much longer (2.8–3 days), perhaps due to more complex procedures or cultural issues.26,27
- -
The rate of hypoparathyroidism was similar to ConT. Three of the eight patients with total thyroidectomies (in either one or two surgeries) had transient hypoparathyroidism (37%). All three recovered in the first 6 weeks. The 3 cases were also the first procedures performed (cases 1, 2 and 3) and were perhaps due to not having performed meticulous parathyroid dissection. From the fourth case on, none of the patients presented hypoparathyroidism. These same results are observed in the literature.10,27
- -
The rate of definitive recurrent paralysis was 0%, and we had one case of transient recurrent laryngeal nerve palsy in a particularly complicated left nerve (one injury out of 20 nerves at risk). It is in these situations where we have most noticed the limitation in maneuverability, which must be compensated with a meticulous surgical technique. The robotic approach provides a significant improvement in ergonomics, easing this difficulty. Although it is true that in Kim's series there is no significant difference observed between the endoscopic and robotic techniques in the rate of injury due to transient or permanent recurrence (3.8% vs 4.5%, P=.677, and 0.3% vs 0.7%, P=1), other authors have observed differences in the rate of recurrent palsy in oncological pathology, but without reaching statistical significance. On the other hand, although the robotic approach implies an increase in the cost per procedure, there are studies that highlight a shorter recovery time of the parathyroid function and the recurrent laryngeal nerve, in cases of injury, in the interventions performed using a robotic approach vs ConT. Likewise, there is literature that suggests a subjective improvement in voice quality and, perhaps, swallowing compared to ConT.26,27,32–34
- -
Regarding the rate of central thoracic dysesthesia, 2 prospective studies conducted by Kim have found alterations in sensitivity in 41.2% of patients with a resolution time of 3 months.35,36 In our series, we asked our patients specific questions, and 80% reported some type of dysesthesia, usually mild and short in duration, except for one patient, with significant dysesthesia lasting one month. After reviewing the video of said surgery, we observed accidental injury to the pectoral fascia during the creation of the subcutaneous tunnel. This was the cause of the pain, and we believe that it is a critical technical point.
No other alterations have been described in the soft tissues used for access. Yu et al.37 reviewed the interferences caused by the approach on imaging studies used to evaluate breast pathologies, finding no interferences during either diagnosis or breast surgery. This is logical considering that the plane of dissection is always subcutaneous.
Finally, satisfaction with the cosmetic outcome was very high in all the patients we have treated. This is the essence of extracervical approaches, and all the studies agree on their superiority to ConT.38,39
In our initial experience, thyroidectomy with the BABA approach is a reproducible procedure that requires surgical teams with experience in endocrine and endoscopic surgery. It would be difficult to say that remote-access thyroidectomy is superior to ConT, as the results of the latter are excellent and the former is technically more demanding. Its aim is to offer an alternative option to patients who do not want a neck scar. Extracervical approaches should not vary the indications for surgery and should have the same safety profile and results as ConT; therefore, proper patient section and indication are essential. The future of these approaches in our country is still uncertain, but we think there is a place for this and other approaches, although it has yet to be defined. In these decisions, our scientific society should play an active role to lay the foundations for its progression and limits.
FundingThis study has received no funding.
Conflict of InterestsEnrique Mercader, Iñaki Amunategui and José Luis Escat Cortés collaborate with Medtronic Ibérica S.A. as medical consultants.
The authors would like to thank Dr. William B. Inabnet, III and his team at Mount Sinai Hospital, Nueva York, for his generosity.
Please cite this article as: Mercader Cidoncha E, Amunategui Prats I, Escat Cortés JL, Grao Torrente I, Suh H. Tiroidectomía sin incisión cervical por abordaje endoscópico biaxilo-biareolar. Primeras impresiones tras su introducción en una unidad especializada. Revisión de la literatura. Cir Esp. 2019;97:81–88.