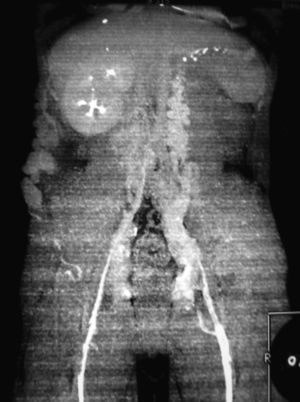
Thrombotic problems are uncommon in childhood, although neonates and infants are more predisposed to presenting them,1 both due to a deficient inhibition of thrombin activity and a relative inefficacy of thrombolysis.2 We present the case of a young man with a complete thrombosis of the left renal vein and inferior vena cava in the neonatal period and that was diagnosed with the absence of inferior vena cava after the appearance of a subcutaneous venous cord in the right flank (Figs. 1 and 2).
A 16-year-old man consulted due to an increase in volume of a subcutaneous venous cord in the right flank that he had since his neonatal period. During that period he had presented sever respiratory distress, bilateral suprarenal hemorrhage and left renal venous thrombosis with subsequent renal atrophy that caused him to undergo a nephrectomy at one year of age. During his first weeks of life he had needed aggressive supportive measure in an Intensive Care Unit and prolonged venous catheterization; the venous cord had appeared at this time. A cavography performed at this time revealed a complete thrombosis of the inferior vena cava with important collateral circulation in the right superficial venous system of the abdominal wall and the left azygos system. The patient recovered progressively and had showed a complete recovery without any further follow-up.
In our department a complete physical examination was performed (Fig. 1) and in a magnetic angioresonance imaging and computed phlebotomography (Fig. 2) an absence of the inferior vena cava and both iliac veins was observed, showing venous return on the right side from the femoral vein through the varicous vein up to the ipsilateral axillary vein and on the left side from the femoral vein through the paravertebral veins to the azygos and hemiazygos system. The patient remains asymptomatic and without signs of venous insufficiency, and a conservative approach with follow-up was recommended.
During the neonatal period, venous thromboses are almost exclusively represented by renal vein thrombosis. In the last 30 years the epidemiology of renal vein thrombosis has changed in developed countries, where almost 50% of cases occur in premature newborns,3 mostly male. The incidence of symptomatic renal thrombosis in newborns is very low (2.2 of every 100000 births), and its association with a complete occlusion of the inferior vena cava is even more uncommon (only 25% of symptomatic cases).1 The appearance of collateral veins that drain in the azygos system, such as our case, with occlusion of the inferior vena cava has rarely been described in the literature.
The classical presentation of renal vein thrombosis is the presence of a palpable abdominal mass, macroscopic hematuria and thrombopenia, although some of these signs might not be present at the time of diagnosis. Some neonates can present with anuria or arterial hypertension. In almost all patients a Doppler ultrasound should be systematic to confirm the diagnosis,4 although in some cases of vena cava thrombosis diagnosis is difficult and other tests such as cavography or plebotomography are needed, as in our case, to determine the location of the occlusion and the trajectory of the collateral circulation.1
When the diagnosis is early, conservative treatment with thrombolysis using r-TPA or fibrinolytics such as heparin or a combination of both (r-TPA and heparin) can be used.5 Thrombectomy was used in the past but has recently been abandoned.1 In our case the diagnosis was made much later after a good collateral circulation had been established, and therefore there was no need for therapy.
Please cite this article as: Canelles E, Bruna M, Artigues I. Cordón venoso subcutáneo en pared abdominal como manifestación de trombosis de vena cava inferior. Cir Esp. 2013;94:275–276.