Neuroendocrine tumors (NET) include various entities, including gangliocytic paragangliomas. Paragangliomas are rare tumors composed of 3 cell types: spindle, endocrine, and ganglion.1–5 The identification of these 3 components, whose proportion varies among tumors, is essential for its diagnosis. They are most frequently located in the duodenum, usually in the periampullary region, and their prognosis is generally good after excision. At diagnosis, 10% present lymph node involvement and 1% liver metastases.4,6
We describe the case of a 69-year-old woman with no relevant history who reported epigastralgia. Fibrogastroscopy revealed a lesion in the second part of the duodenum near the papilla compatible with a NET. Endoscopic ultrasound showed a well-defined, homogeneous, hypoechoic lesion measuring about 16 × 9 mm in the mucosa, with preservation of deep planes and mild dilatation of the Wirsung duct of up to 3.3 mm; no pathological lymphadenopathies were observed. The endoscopic appearance suggested a possible gastrointestinal stromal tumor or a leiomyoma. The pathological study of the endoscopic biopsy demonstrated invasion of the submucosa and the lamina propria by a G2 NET (Ki67 4%). Due to the characteristics of the lesion, endoscopic excision was ruled out.
An octreotide scan was performed, which showed no evidence of accumulation of the radiotracer to indicate a mass with somatostatin receptors. Abdominal CT scan with intravenous contrast showed a nodule measuring about 17 mm in the periampullary region, which was causing minimal ectasia of the common bile and Wirsung ducts. The scan also ruled out the presence of lymph node dissemination or distant metastasis (Fig. 1).
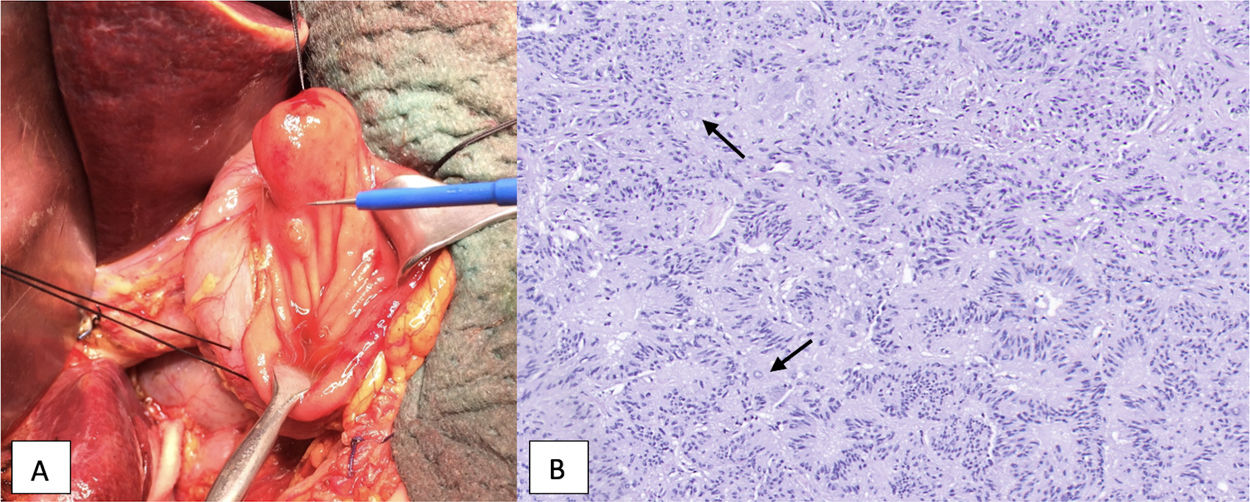
As it was a small tumor with a low proliferative index (Ki67) and no distant spread, transduodenal ampullectomy was performed with reanastomosis of the Wirsung and bile ducts to the duodenal mucosa. Intraoperative pathological analysis confirmed free resection margins. The definitive analysis identified the tumor as a gangliocytic paraganglioma measuring 17 × 12 mm located in the ampulla of Vater, with free margins and no signs of angiolymphatic or perineural invasion (Fig. 2).
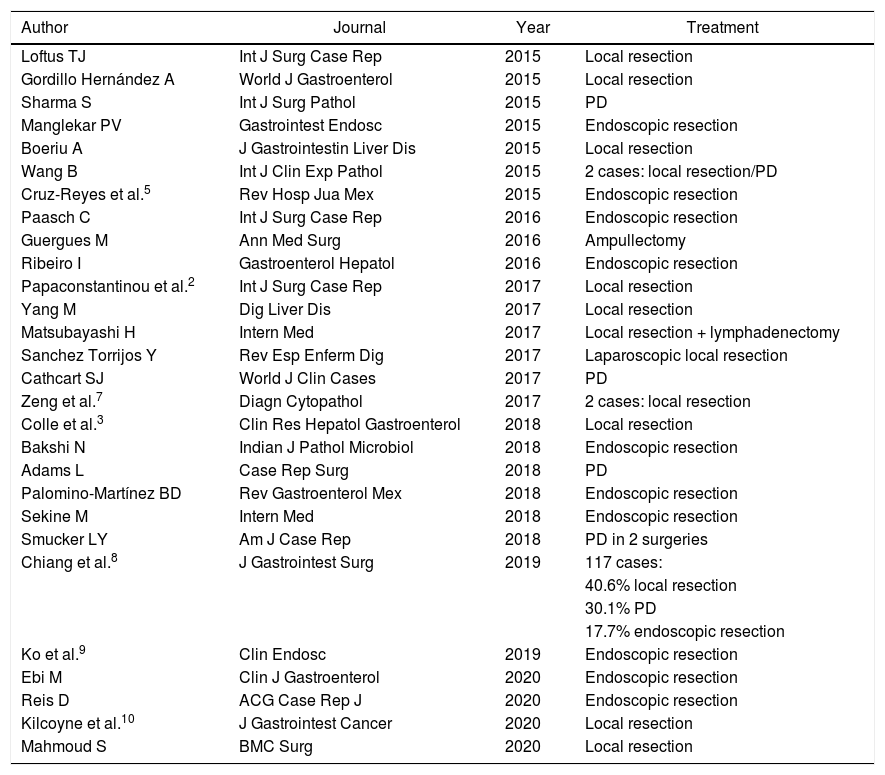
Juxtapapillary gangliocytic paraganglioma: A) macroscopic view; B) microscopic view (hematoxylin–eosin stain). Neuroendocrine cell sample (nests of elongated cells forming cords or pseudoglandular structures, in palisade), cells with differentiation to Schwann cells and ganglion cells (larger, with ample cytoplasm, large and vesicular nucleus; marked with an arrow).
Patient progress was satisfactory, leading to discharge on the seventh postoperative day. In the long-term follow-up, the patient has been asymptomatic and has had no evidence of recurrence 2 years after the procedure.
Periampullary paragangliomas usually appear in the fifth or sixth decades of life, with a slight predisposition among males (1.7:1).3 They are usually detected as an incidental finding during endoscopy or an imaging test,1 or, in symptomatic cases, in the form of gastrointestinal bleeding, abdominal pain or anemia.1–4 Gastrointestinal bleeding occurs due to ulceration of the overlying mucosa. Obstructive jaundice secondary to ampullary paragangliomas has been described but is rare.1,6
Non-functioning paragangliomas, as in this case, are difficult to diagnose preoperatively due to the lack of specific symptoms. They are often difficult to differentiate from other NET because they share morphological and immunohistochemical characteristics. Their differentiation is important because, although NET generally have a good prognosis, paragangliomas have an even more favorable prognosis and can benefit from less aggressive treatment. Both entities express chromogranin and synaptophysin.7 Finding the expression of pancreatic polypeptide, progesterone receptors, vimentin and GATA-3 in the immunohistochemical analysis is useful to diagnose paragangliomas, since NET do not express them.4,7 They can also be confused with gastrointestinal stromal tumors.2
Paragangliomas can be sessile or pedunculated tumors. On ultrasound, they appear like a solid, homogeneous and hypoechoic mass. Abdominal CT is useful for characterizing the lesion and is used for the extension study. As previously mentioned, the definitive diagnosis is histological and immunohistochemical.
Treatment consists of complete tumor excision with free margins. Table 1 shows the articles published on the subject from 2015 to 2020 (inclusive) and the treatment that was used on each occasion. As shown, endoscopic resection can be a safe and appropriate procedure in selected cases. When this approach is not possible, surgical resection is indicated, which is usually the most frequently performed treatment. Predictive factors for lymph node metastasis include tumor size greater than 2 cm, age (young patients are at higher risk) and deep tumors that go beyond the submucosal layer.3 Follow-up of these patients is recommended because, despite the benign nature of these tumors, cases of local recurrence have been described and the lesions have metastatic potential.1
Articles about paraganglioma published between 2015 and 2020.
| Author | Journal | Year | Treatment |
|---|---|---|---|
| Loftus TJ | Int J Surg Case Rep | 2015 | Local resection |
| Gordillo Hernández A | World J Gastroenterol | 2015 | Local resection |
| Sharma S | Int J Surg Pathol | 2015 | PD |
| Manglekar PV | Gastrointest Endosc | 2015 | Endoscopic resection |
| Boeriu A | J Gastrointestin Liver Dis | 2015 | Local resection |
| Wang B | Int J Clin Exp Pathol | 2015 | 2 cases: local resection/PD |
| Cruz-Reyes et al.5 | Rev Hosp Jua Mex | 2015 | Endoscopic resection |
| Paasch C | Int J Surg Case Rep | 2016 | Endoscopic resection |
| Guergues M | Ann Med Surg | 2016 | Ampullectomy |
| Ribeiro I | Gastroenterol Hepatol | 2016 | Endoscopic resection |
| Papaconstantinou et al.2 | Int J Surg Case Rep | 2017 | Local resection |
| Yang M | Dig Liver Dis | 2017 | Local resection |
| Matsubayashi H | Intern Med | 2017 | Local resection + lymphadenectomy |
| Sanchez Torrijos Y | Rev Esp Enferm Dig | 2017 | Laparoscopic local resection |
| Cathcart SJ | World J Clin Cases | 2017 | PD |
| Zeng et al.7 | Diagn Cytopathol | 2017 | 2 cases: local resection |
| Colle et al.3 | Clin Res Hepatol Gastroenterol | 2018 | Local resection |
| Bakshi N | Indian J Pathol Microbiol | 2018 | Endoscopic resection |
| Adams L | Case Rep Surg | 2018 | PD |
| Palomino-Martínez BD | Rev Gastroenterol Mex | 2018 | Endoscopic resection |
| Sekine M | Intern Med | 2018 | Endoscopic resection |
| Smucker LY | Am J Case Rep | 2018 | PD in 2 surgeries |
| Chiang et al.8 | J Gastrointest Surg | 2019 | 117 cases: |
| 40.6% local resection | |||
| 30.1% PD | |||
| 17.7% endoscopic resection | |||
| Ko et al.9 | Clin Endosc | 2019 | Endoscopic resection |
| Ebi M | Clin J Gastroenterol | 2020 | Endoscopic resection |
| Reis D | ACG Case Rep J | 2020 | Endoscopic resection |
| Kilcoyne et al.10 | J Gastrointest Cancer | 2020 | Local resection |
| Mahmoud S | BMC Surg | 2020 | Local resection |
PD: pancreaticoduodenectomy.
In patients with lesions of low malignant potential such as paragangliomas, with no evidence of extension of the disease on imaging tests, less aggressive surgical techniques, should be considered, such as ampullectomy. This should always be done in association with intraoperative pathological study of margins and distant tumor extension studies. In these cases, depending on the intraoperative or definitive findings, we should consider a possible change in surgical strategy to a more extensive surgery, such as pancreaticoduodenectomy, although this presents more complications and sequelae.
Please cite this article as: Lucas Guerrero V, González Costa A, Romaguera Monzonis A, Bejarano González N, García Borobia F. Estrategia de manejo quirúrgico en tumores de bajo potencial maligno de localización ampular. Presentación de un caso de paraganglioma gangliocítico. Cir Esp. 2021;99:621–623.