Parastomal hernias (PH) are the most common complication after creating a stoma, appearing in up to 48% of cases.1 There is a clear lack of information in the literature regarding the treatment of parastomal hernias requiring urgent treatment (UPH). Currently, we do not have studies that specifically evaluate the results and characteristics of UPH management. There are indirect data in certain registries that analyze the incidence of UPH in groups of patients treated for PH2 or the risk factors for morbidity, mortality and recurrence in PH surgery, where UPH seems to be a factor associated with reoperation or death in the first 30 postoperative days,3 or where age over 70 may increase the risk of morbidity and mortality in the context of UPH.4 There is also no guidance on the best way to treat UPH in published PH management guidelines.5 When faced with a PH requiring urgent treatment, most surgeons probably base their decisions on the indirect data mentioned above and other ‘data’ learned during our ‘teacher-apprentice’ training. These are difficult to quantify and the result of experience, such as avoiding the use of a non-absorbable synthetic mesh in most cases if there is ischemia or intestinal resection.6
In this context, we present the experience of our hospital in the management of UPH over a period of 12 years (2007–2019). We have conducted a descriptive analysis of a series of 24 patients with UPH. Our aim is to provide an interesting assessment of a surgical condition about which there is practically no specific data in the literature.
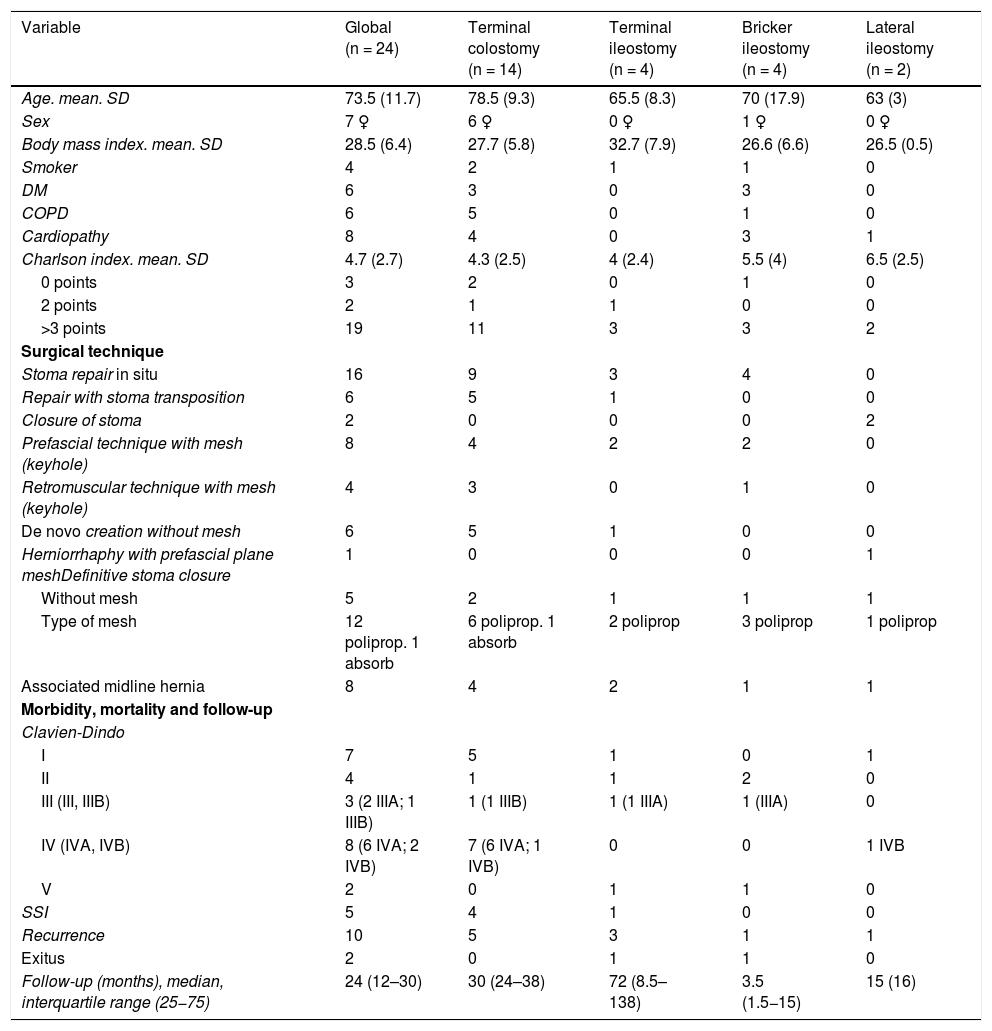
During the study period, 244 ostomies were treated in the emergency room for different reasons, 41 of which (16.8%) were PH, and 24 (9.8%) of these required urgent surgery (Table 1). UPH may have a low incidence in the context of ostomy-related emergencies. However, once in the emergency room, a high percentage of these hernias require surgical intervention. In our cases, urgent surgery was necessary in 58.5%. Most of the UPH involved definitive colostomies (14 cases [58.3%]), although other definitive ostomies were also treated, such as terminal ileostomies and Bricker-type ileostomies, and even temporary ostomies such as lateral ileostomies. The majority of the patients were male, with high comorbidity (Charlson index >3 points in 19 [79.1%] patients) and a mean age over 70 years. A high Charlson index and age over 70 are associated with high mortality.4,7 A total of 2 deaths were observed. We believe that this percentage was high (8.3%) and probably associated with age and present comorbidities. However, these cases corresponded to a lower mean age group and less frequent ostomies, such as terminal ileostomy or Bricker-type ileostomy. The surgical technique selected for UPH repair was mainly in situ (16 [66.6%] patients) without transposition of the stoma; in the 2 cases of lateral temporal ileostomy, the stoma was permanently closed. Non-absorbable synthetic mesh (polypropylene) was used in 12 (50%) cases, regardless of the type of stoma and if the surgery was at least clean-contaminated. The decision to place the mesh may be influenced not only by the type of surgery but also by the need to concomitantly repair an associated midline incisional hernia, which was observed in 8 (33.3%) patients. The surgical site infection (SSI) rate was high (5 patients; 20.8%), which can be expected in emergency surgery that are clean-contaminated at the very least. According to the Clavien–Dindo classification,8 all patients experienced some type of postoperative complication; more than half started with grade III, that is, requiring surgical or radiological intervention and being life-threatening complications requiring treatment in intermediate or intensive care units, and finally mortality. The recurrence of PH was high, affecting 10 (41.6%) patients after a median follow-up of 24 months (IQR: 12–30). This demonstrates the classic high rate of recurrences described after surgery for PH,9 which is probably elevated in this series because urgent surgeries have a high rate of postoperative complications.
Descriptive characteristics of urgent parastomal hernia.
| Variable | Global (n = 24) | Terminal colostomy (n = 14) | Terminal ileostomy (n = 4) | Bricker ileostomy (n = 4) | Lateral ileostomy (n = 2) |
|---|---|---|---|---|---|
| Age. mean. SD | 73.5 (11.7) | 78.5 (9.3) | 65.5 (8.3) | 70 (17.9) | 63 (3) |
| Sex | 7 ♀ | 6 ♀ | 0 ♀ | 1 ♀ | 0 ♀ |
| Body mass index. mean. SD | 28.5 (6.4) | 27.7 (5.8) | 32.7 (7.9) | 26.6 (6.6) | 26.5 (0.5) |
| Smoker | 4 | 2 | 1 | 1 | 0 |
| DM | 6 | 3 | 0 | 3 | 0 |
| COPD | 6 | 5 | 0 | 1 | 0 |
| Cardiopathy | 8 | 4 | 0 | 3 | 1 |
| Charlson index. mean. SD | 4.7 (2.7) | 4.3 (2.5) | 4 (2.4) | 5.5 (4) | 6.5 (2.5) |
| 0 points | 3 | 2 | 0 | 1 | 0 |
| 2 points | 2 | 1 | 1 | 0 | 0 |
| >3 points | 19 | 11 | 3 | 3 | 2 |
| Surgical technique | |||||
| Stoma repair in situ | 16 | 9 | 3 | 4 | 0 |
| Repair with stoma transposition | 6 | 5 | 1 | 0 | 0 |
| Closure of stoma | 2 | 0 | 0 | 0 | 2 |
| Prefascial technique with mesh (keyhole) | 8 | 4 | 2 | 2 | 0 |
| Retromuscular technique with mesh (keyhole) | 4 | 3 | 0 | 1 | 0 |
| De novo creation without mesh | 6 | 5 | 1 | 0 | 0 |
| Herniorrhaphy with prefascial plane meshDefinitive stoma closure | 1 | 0 | 0 | 0 | 1 |
| Without mesh | 5 | 2 | 1 | 1 | 1 |
| Type of mesh | 12 poliprop. 1 absorb | 6 poliprop. 1 absorb | 2 poliprop | 3 poliprop | 1 poliprop |
| Associated midline hernia | 8 | 4 | 2 | 1 | 1 |
| Morbidity, mortality and follow-up | |||||
| Clavien-Dindo | |||||
| I | 7 | 5 | 1 | 0 | 1 |
| II | 4 | 1 | 1 | 2 | 0 |
| III (III, IIIB) | 3 (2 IIIA; 1 IIIB) | 1 (1 IIIB) | 1 (1 IIIA) | 1 (IIIA) | 0 |
| IV (IVA, IVB) | 8 (6 IVA; 2 IVB) | 7 (6 IVA; 1 IVB) | 0 | 0 | 1 IVB |
| V | 2 | 0 | 1 | 1 | 0 |
| SSI | 5 | 4 | 1 | 0 | 0 |
| Recurrence | 10 | 5 | 3 | 1 | 1 |
| Exitus | 2 | 0 | 1 | 1 | 0 |
| Follow-up (months), median, interquartile range (25−75) | 24 (12–30) | 30 (24–38) | 72 (8.5–138) | 3.5 (1.5−15) | 15 (16) |
SD: standard deviation; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease.
UPH surgery seems to be rare; however, it may be associated with serious complications and high postoperative mortality,10 as well as a high rate of recurrences. We have presented our experience over a period of time at a high-volume hospital. We believe that this experience is of interest to better understand certain specific data about this condition in an urgent care context. However, it is essential to register cases related to UPH in registries such as EVEREG,11 which is endorsed by the Spanish Association of Surgeons, as it is necessary to obtain information on a larger scale about this elusive urgent condition. This could contribute to future prevention and treatment guidelines.
FundingThis study has not been funded by public or private organizations.
Please cite this article as: Verdaguer M, Jofra M, Rodrigues V, Rosselló-Jiménez D, López-Cano M. Hernia paraestomal. Reparación urgente. Cir Esp. 2021;99:619–620.