Conceptually, ‘telemedicine’ is the exchange of clinical information at a distance that uses information and communications technology (ICT), and whose objective it is to improve patient health.1 A distinction must be made from ‘telehealth’, which also encompasses everything related to ‘teletraining’ (webinars, teleconferences, etc) in which healthcare workers, patients and/or health-related administrators participate, and any user can use to improve their own or collective health using apps, big data or cloud computing services.2
Telemedicine services can be done in real time (synchronous) or delayed (asynchronous). Teleconsultations can be carried out with patients or among medical professionals, either over the phone or using videoconference systems. It enables users to view images, photos of lesions, histological preparations, or even electrocardiograms, etc. Radiological studies can be interpreted remotely, generally in delayed images obtained in situ by ultrasound, CT, and MRI devices. In our setting, these services are already being implemented and enable remote assessment of reports and images by multidisciplinary teams dedicated to specific diseases, which avoids patients having to move from their homes, especially if rural or very distant. COVID-19 has been a great catalyst in telemedicine in recent weeks for consultations, and its implementation (which, by the way, has been very poorly planned) has nevertheless been very effective.
‘Telementoring’, which provides remote guidance of techniques that are difficult to implement, is especially important now that the mobility of medical professionals is limited and, as in recent months, rotations have been suspended (both for residents as well as non-expert surgeons) along with the possibility of going to other hospitals to witness in situ how innovative techniques are implemented and conducted. As with telemedicine, it requires technology in order to observe how the procedure is performed and to interact with experts and, although it is unquestionable that 5G technology could optimize transmission speed and signal stability, it can now be conducted regardless.3 Graphics can also be used to provide indications on the screen, and the greater the possibilities for interaction through image, voice and sound, the better the telecommunication, thereby transmitting more information. We have been able to experiment for more than 6 months in our hospital with the PROXIMIE4 platform founded by Nadine Hachach-Haram, Head of Clinical Innovation at Guy’s and St Thomas’ NHS Foundation Trust. Using augmented reality, this platform enables surgeons to interact and share practical knowledge remotely (through closed monographic sessions, video atlas, webinars, etc) using a cell phone, laptop or tablet. It is essential for the expert or mentor to have experience and demonstrated ability, while knowledge and previous basic skills are likewise fundamental for the apprentice.3
Sometimes synchronous telementoring is difficult, and it is under these circumstances that guidance video-based coaching (VBC) is another option to be considered. Every effort should be made to structure the activity, with pre-established objectives and actions, and postoperative instructions and evaluations should not be done more than 2–3 days before and after surgery.
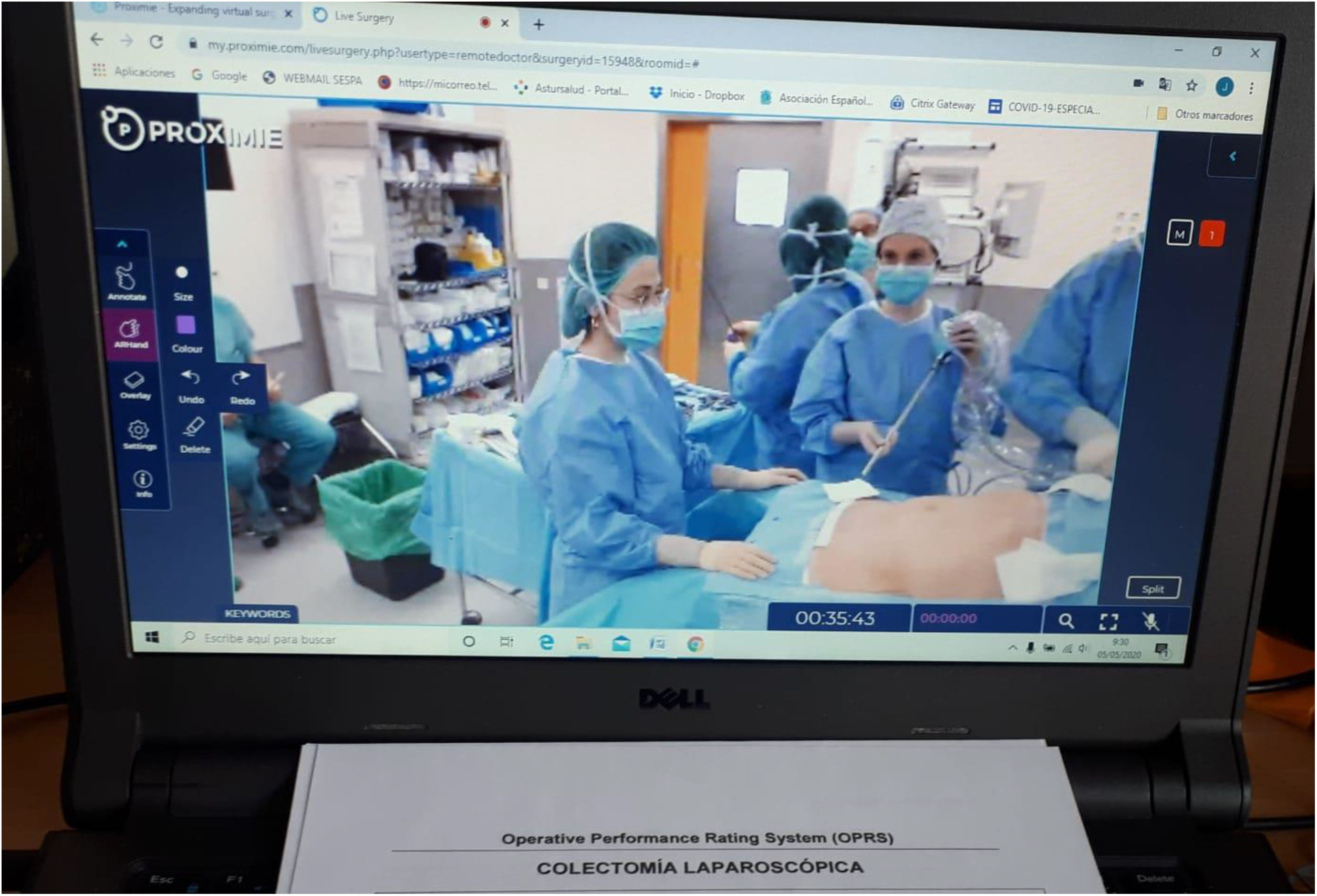
Until now, no structured objective evaluation has been proposed in the Spanish residency (MIR) program for our specialty, and the only evaluation can be considered the least demanding possible: a portfolio listing the number of procedures in which the resident has participated, as well as the training and research completed. Media that currently offer us platforms (such as the one mentioned) make ‘telematic evaluations’ of surgical practice possible. These can be done by applying objective evaluation systems as they have been carried out in situ at the ABS for years, with the validation included.5 According to a survey carried out in our service, it seems that this would be well received by current residents, the majority of whom already have experience with Structured Objective Clinical Evaluation (SOCE) in their undergraduate training. Given our accumulated experience with SOCE in experimental minimally invasive surgery, we have recently begun to carry out telematic evaluations in the operating room for year-5 residents (MIR5) with PROXIMIE (Fig. 1).5,6
Therefore, telemedicine (as a selective care option in the consultation), teleconsultations between medical centers to assess cases of a certain complexity, telementoring for the incorporation of innovative procedures, and telematic evaluation for better prepared surgeons, are all challenges to consider. These are all factors to be assessed in order to obtain something positive from our recent pandemic experience and, above all, to develop new pathways for improved patient care, management, training and research activities.
Please cite this article as: Rodríguez García JI, Contreras Sáiz E, García Munar M, García Flórez L, Granero Trancón J. Telemedicina, telementorización y evaluación telemática en cirugía. ¿Es su momento después de la COVID-19? Cir Esp. 2021;99:474–475.