Central venous catheters for hemodialysis provide reliable access for dialysis in end-stage patients with chronic kidney disease1 using a less invasive, percutaneous approach. Iatrogenic injury to venous vessels can occur during placement of these catheters. Rupture or perforation of the superior vena cava (SVC) is an uncommon but potentially fatal complication.
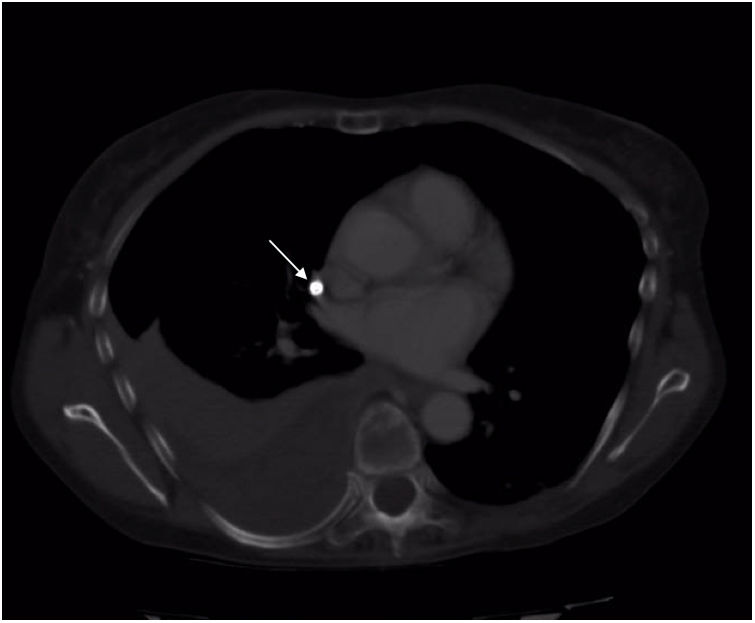
We present the case of a 59-year-old woman with a history of hypertension, dyslipidemia, secondary hyperparathyroidism and adult polycystic liver disease with stage V chronic kidney disease requiring dialysis. She was admitted for the placement of a tunneled catheter through the right jugular vein, after which she suddenly began to have pleuritic chest pain. Given the clinical manifestations, contrast medium was introduced through the catheter under fluoroscopic control, which showed extravasation to the right hemidiaphragm. We decided to perform computed tomography angiography (CT angiogram) (Fig. 1), which showed that the catheter had perforated the vein at the right jugular-subclavian junction, with associated hemothorax. The patient was transferred to the intensive care unit for monitoring and evacuation of the hemothorax through a chest tube, while remaining hemodynamically stable. After multidisciplinary assessment by vascular surgery and thoracic surgery specialists, a video-assisted surgical procedure was performed (Fig. 2A) with two ports: one optical trocar, and one minithoracotomy.
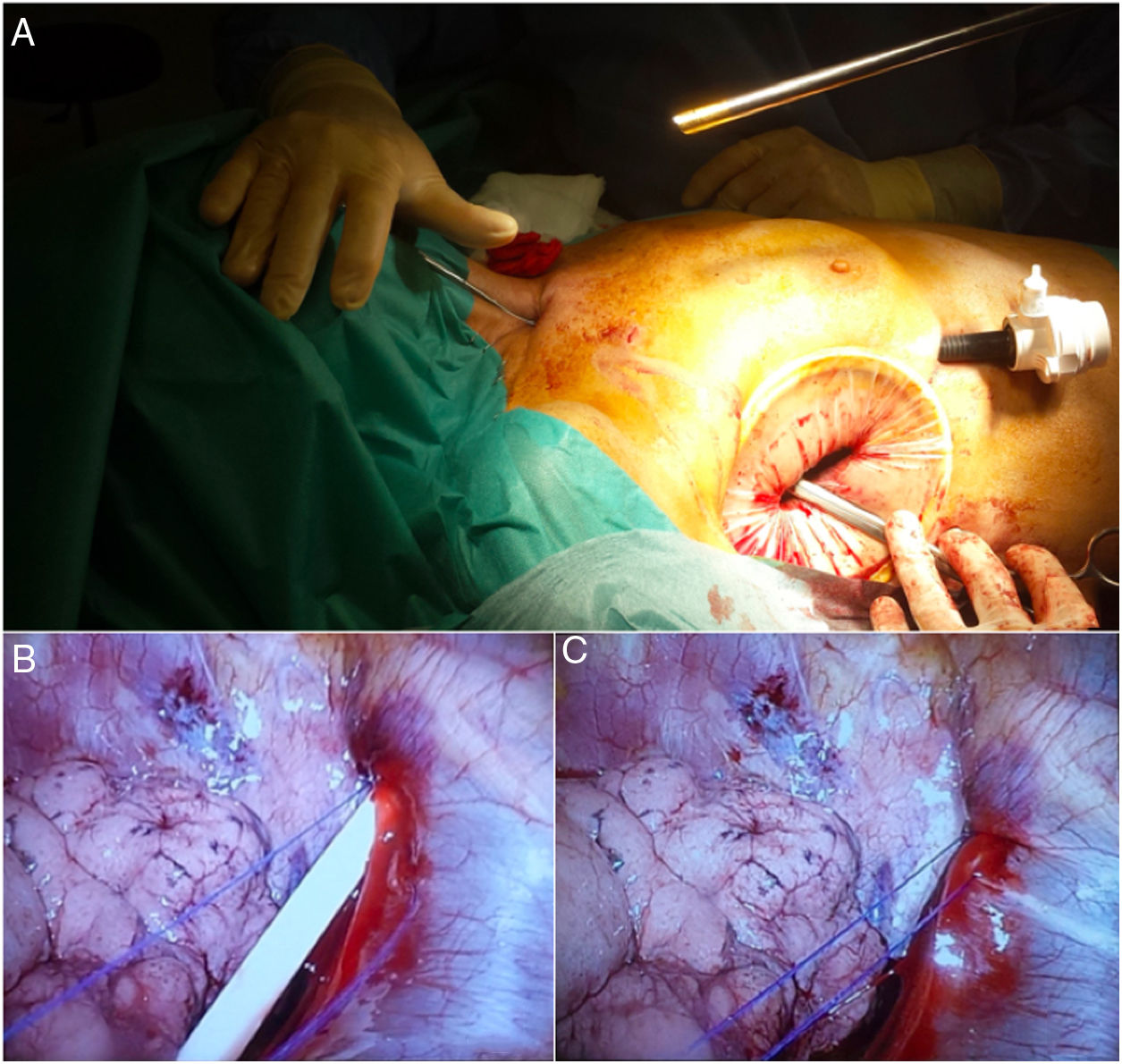
(A) Minithoracotomy in the right-side 5th intercostal space and trocar access for optics in the right-side 7th intercostal space, (B) Exit point of the central venous catheter through the lateral vena cava at its confluence with the innominate vein trunk, right subclavian vein and right jugular vein. Prolene®3/0 sutures proximal and distal to the perforated catheter prior to its removal, (C) Closure of the defect after removal of the catheter.
Once the extravasation point was located, hemostatic control was established using Prolene® 3/0 sutures proximal and distal to the perforated catheter. This allowed for it to be removed proximally, with closure of the defect (Fig. 2B and C). After confirmation of hemostasis, placement of Surgicel® on the venous suture and evacuation of the hemothorax, we proceeded with chest tube insertion and closure of the assistance minithoracotomy.
The patient progressed well. The thoracic drain tube was removed on the 2nd postoperative day, and the patient was discharged from the intensive care unit on the 4th day. After follow-up in the hospital without incidents, she was discharged on the 7th postoperative day.
Although the placement of central venous catheters is a therapeutic possibility in patients in need of dialysis, the technique is not without risks. Venous vessel rupture is an uncommon but possible and potentially life-threatening complication, especially when the SVC is compromised. To prevent these complications, ultrasound-guided catheter insertion has been shown to increase the safety of the procedure.2,3
The manifestations of SVC perforation, such as hemothorax or cardiac tamponade, will lead to the need for urgent treatment to save the patient’s life when they cause hemodynamic instability. However, it is possible to adapt both the time of the intervention and the technique when the clinical situation allows it. The diagnosis is based on the injection of contrast through the catheter under radiological control, which shows evidence of extravasation,2,4,5 or by means of high-resolution imaging tests (CT angiography). In addition, transesophageal/transthoracic bedside ultrasound is an alternative in unstable patients that provides diagnostic confirmation and facilitates the initiation of therapeutic measures (pericardiocentesis).2,4,6
The aim of treatment is to repair the injured vessel and recover cardiac function, when compromised.4 Open SVC repair requires median sternotomy, which is an aggressive and complex alternative for many of our patients.5,7 To reduce the morbidity associated with this approach, therapeutic alternatives such as the endovascular approach4,8 have been described, with the placement of stents providing good results. Likewise, in certain stable patients with no signs of cardiac tamponade, conservative management could be a therapeutic modality.9 In the case of cardiac tamponade, pericardiocentesis should have priority over the vessel repair.4
Although endovascular repair is a therapeutic alternative in patients with ruptured SVC, the location of the injury may determine its chances of success. In our case, given the confluence of the jugular vein with the subclavian vein in the perforation area, the VATS approach was considered the first therapeutic option in a hemodynamically stable patient with no signs of cardiac tamponade.
Based on our review of the literature, this is the third case report7,10 that includes VATS as a therapeutic option in the treatment of SVC rupture. Although it has been considered contraindicated in unstable patients, Cheli et al.10 associated the traditional thoracotomy approach with the use of 30° optics due to the inability to visualize and access the bleeding point. Kuzniec et al.7 presented the repair of a ruptured SVC using VATS in a stable patient as the first approach to treatment, with good results.
In our opinion, and although the experience is limited, VATS for the repair of a ruptured SVC secondary to the insertion of a central venous catheter in stable patients without cardiac tamponade is an alternative that provides direct visualization of the affected hemithorax in order to control the bleeding point, remove the venous catheter, directly repair the SVC and evacuate the hemothorax with good results.
The authors would like to thank the Vascular Surgery Department for their time, dedication.
Please cite this article as: Sánchez Matás C, Manresa Manresa F, Andrades Sardiña D, López Villalobos JL, Bataller de Juan ME. Abordaje toracoscópico de perforación iatrogénica de vena cava superior por catéter de diálisis. Cir Esp. 2020;98:364–366.