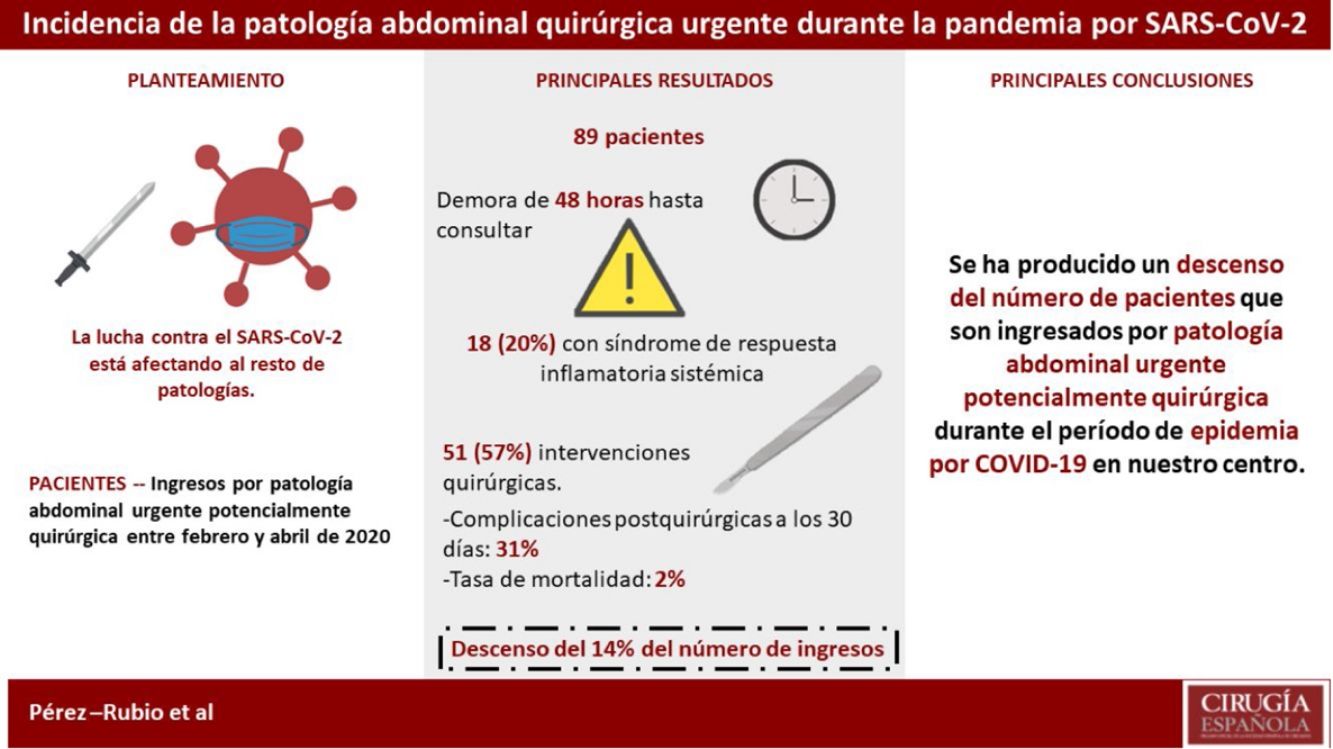
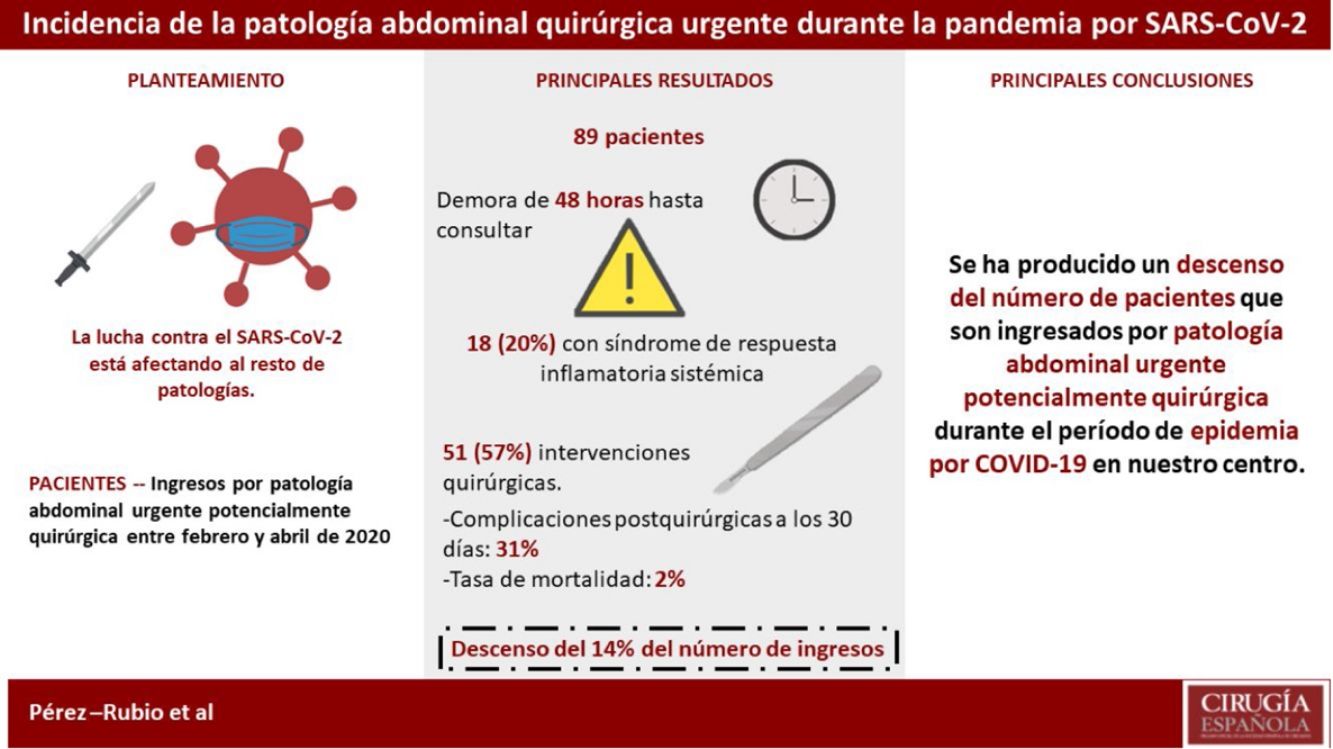
Since the appearance of SARS-CoV-2 in December 2019 in the Chinese city of Wuhan, we have experienced a reduction in admissions in our Service and a decrease in urgent surgical activity. Therefore, this study aimed to assess the incidence of potentially surgical abdominal emergency in our center during the epidemic of COVID-19.
MethodsA retrospective study was designed. It included all patients admitted for urgent abdominal pathology with potential surgical treatment in our General and Digestive Surgery Department from February 24, 2020 to April 19, 2020.
ResultsEighty-nine patients with a mean age of 58.85±22.2 were included. The median time from symptom onset to the Emergency Department (ED) visit was 48 (P25–P75=24–96) hours. On arrival at the ED, 18 (20%) patients presented with systemic inflammatory response syndrome criteria. Fifty-one (57%) surgical procedures were performed. The rate of post-surgical complications at 30 days was 31% and the mortality rate was 2%. Concerning the same period from 2017 to 2019, the mean number of admissions from the ED to our Department decreased by 14% during the epidemic period.
ConclusionThere has been a decrease in the number of patients admitted for urgent, potentially surgical, abdominal pathology during the period of the COVID-19 epidemic in our center.
Desde la aparición en diciembre de 2019 del SARS-CoV-2 en la ciudad de Wuhan, China, hemos experimentado un descenso en los ingresos en nuestro Servicio y disminución de la actividad quirúrgica urgente. Por ello, el objetivo de este estudio fue analizar la incidencia de la patología abdominal urgente potencialmente quirúrgica en nuestro centro durante la epidemia por COVID-19.
MétodosSe diseñó un estudio retrospectivo que incluyó a todos los pacientes ingresados por patología abdominal urgente potencialmente quirúrgica en nuestro Servicio de Cirugía General y del Aparato Digestivo desde el 24 de febrero de 2020 hasta el 19 de abril de 2020.
ResultadosSe incluyeron 89 pacientes con una edad media de 58,85±22,2. La mediana de tiempo transcurrido desde el inicio de los síntomas hasta la consulta en el Servicio de Urgencias fue de 48 (P25-P75=24-96) horas. A su llegada a Urgencias 18 (20%) pacientes presentaban criterios de síndrome de respuesta inflamatoria sistémica (SRIS). Se realizaron 51 (57%) intervenciones quirúrgicas. La tasa de complicaciones postquirúrgicas a los 30 días fue del 31% y la tasa de mortalidad de 2%. Con respecto al mismo período de los años 2017 a 2019, la media de ingresos desde Urgencias en nuestro Servicio descendió un 14% durante el período de epidemia.
ConclusionesSe ha producido un descenso en el número de pacientes que son ingresados por patología abdominal urgente potencialmente quirúrgica durante la epidemia por COVID-19 en nuestro centro.
Since the appearance of the SARS-CoV-2 coronavirus in the city of Wuhan, China1 in December 2019, its global expansion has been rapid and unstoppable, and the COVID-19 epidemic was declared a pandemic on March 11, 2020.2 The consequences at all levels, never seen before, have made it necessary to focus all the attention of health systems on this new disease, which has happened in Spain in areas with high incidence.
More specifically, as far as surgical specialties are concerned, this has led to a gradual cancelation of all elective surgical interventions and even their total cancelation in certain hospitals.3 In part, this has been carried out as a measure of protection against infection for these patients, especially cancer patients,4 but it has been fundamentally due to the need to dedicate all human resources in surgery departments to the care of COVID patients during the crisis and/or the conversion of operating rooms into Intensive Care Units (ICU).
In addition, due to the recommendations of health authorities and medical organizations, together with the fears of citizens themselves, a significant decrease in consultations has been observed in ambulatory care and hospital emergency services of the Spanish National Healthcare System.5 The delay in treatment of surgical pathologies, as well as the consequent loss of opportunity for early treatment, may be detrimental to the health of our patients.
Furthermore, given the high rates of infection of this disease, surgical specialties have had to use a more suitable therapeutic approach in patients who are carriers of the virus or present active infection, which may have led to a change in the final treatment decision that would have been made under normal conditions, assuming possible associated risks.
The objective of this study is to describe the incidence of potentially surgical urgent abdominal pathology at our hospital during the COVID-19 epidemic, analyzing the type of treatment, complications, disease course and patient mortality.
MethodsWe designed a retrospective study including all patients admitted for abdominal pathology potentially requiring urgent surgery at the Doctor Peset University Hospital in Valencia from February 24, 2020, the date on which the first Interterritorial Consejo of the National Healthcare System was convened to coordinate measures with the Autonomous Communities,6 until April 19, 2020.
Our study analyzed the following variables: demographic, clinical, laboratory, radiological, type of surgical intervention, need for intensive care, complications during hospitalization and postoperative complications according to the Clavien-Dindo classification,7 SARS-CoV-2 infection, days of hospitalization, readmissions and 30-day mortality. Data were obtained from digitized clinical, radiological and surgical reports. In addition, the incidence of urgent abdominal pathologies and the number of urgent admissions in the same period from 2017 to 2019 were obtained after consulting the electronic records available in the Hospital Admission Department.
The state of sepsis was defined according to the consensus conference of the American College of Chest Physicians/Society of Critical Care Medicine.8 The severity of abdominal pathologies was classified as follows: the American Association for the Surgery of Trauma (AAST) system was used for acute appendicitis,9 the classification of the World Society of Emergency Surgery (WSES) working group for acute diverticulitis,10 and the 2018 Tokyo guidelines for acute cholecystitis.11
Due to the epidemic situation, it was necessary to use a screening system capable of identifying patients suspected of having SARS-CoV-2 infection to thus act accordingly. This was implemented by the Radiodiagnostic Service starting April 5, 2020. All patients admitted to our Service underwent a low-dose radiation thoracic computed tomography (CT) scan, regardless of the type of treatment to be performed. It was not until April 21, 2020 that serological tests by immunochromatography techniques and the detection of SARS-CoV-2 nucleic acids in samples of nasopharyngeal exudate in real-time time polymerase chain reaction (RT-PCR) were included in the screening tests.
Statistical AnalysisContinuous variables were presented as mean and standard deviation (SD) or median with interquartile range (IQR) depending on whether they were parametric or non-parametric variables. The qualitative variables were expressed as frequencies and percentages. Descriptive statistical analysis was performed with SPSS® statistical software, version 22.0.0 (SPSS, Inc., Chicago, IL, USA).
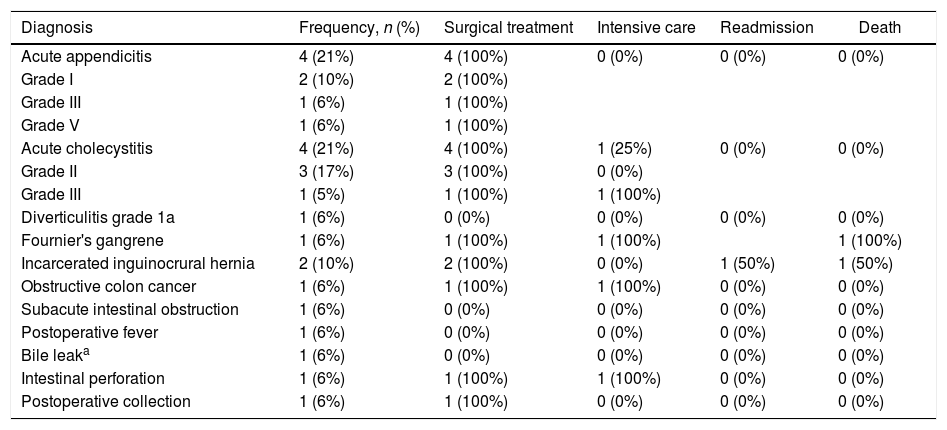
ResultsA total of 89 patients were included in the study, with a mean age of 58.85±22.2 years, 37 of which (42%) were men and 52 (58%) were women. The median time elapsed from the onset of symptoms to consultation in the Emergency Department was 48 (P25–P75=24–96) hours. Upon arrival at the emergency room, 18 (20%) patients presented criteria for systemic inflammatory response syndrome (SIRS) (Table 1).
Characteristics of patients with SIRS criteria at diagnosis between February 24 and April 18, 2020.
| Diagnosis | Frequency, n (%) | Surgical treatment | Intensive care | Readmission | Death |
|---|---|---|---|---|---|
| Acute appendicitis | 4 (21%) | 4 (100%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Grade I | 2 (10%) | 2 (100%) | |||
| Grade III | 1 (6%) | 1 (100%) | |||
| Grade V | 1 (6%) | 1 (100%) | |||
| Acute cholecystitis | 4 (21%) | 4 (100%) | 1 (25%) | 0 (0%) | 0 (0%) |
| Grade II | 3 (17%) | 3 (100%) | 0 (0%) | ||
| Grade III | 1 (5%) | 1 (100%) | 1 (100%) | ||
| Diverticulitis grade 1a | 1 (6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Fournier's gangrene | 1 (6%) | 1 (100%) | 1 (100%) | 1 (100%) | |
| Incarcerated inguinocrural hernia | 2 (10%) | 2 (100%) | 0 (0%) | 1 (50%) | 1 (50%) |
| Obstructive colon cancer | 1 (6%) | 1 (100%) | 1 (100%) | 0 (0%) | 0 (0%) |
| Subacute intestinal obstruction | 1 (6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Postoperative fever | 1 (6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Bile leaka | 1 (6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Intestinal perforation | 1 (6%) | 1 (100%) | 1 (100%) | 0 (0%) | 0 (0%) |
| Postoperative collection | 1 (6%) | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) |
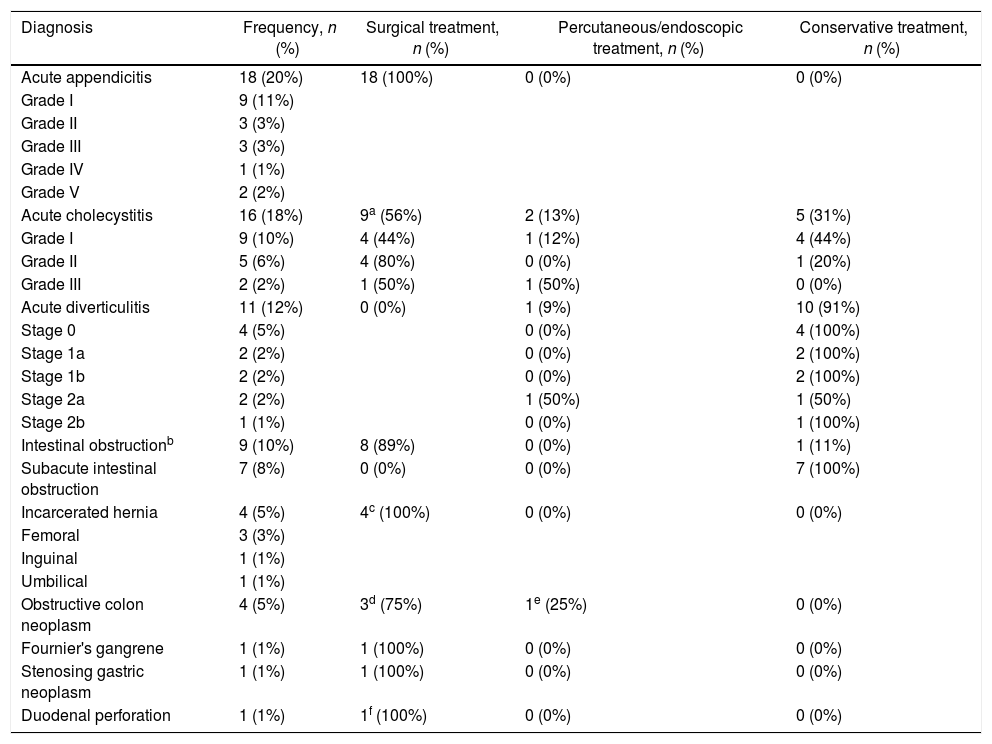
There were 51 (57%) surgical procedures, 4 (5%) percutaneous treatments, and 2 (2%) endoscopic treatments; 32 (36%) patients were treated conservatively; 88 (99%) patients included in the study consulted on their own request in the Emergency Department. One patient (1%) was admitted for COVID-19 and presented a perforated cecum during hospitalization (probably related to the administration of tocilizumab), which was treated with ileocecal resection and a protective ileostomy (Table 2).
Main clinical symptoms and treatment from February 24 to April 18, 2020.
| Diagnosis | Frequency, n (%) | Surgical treatment, n (%) | Percutaneous/endoscopic treatment, n (%) | Conservative treatment, n (%) |
|---|---|---|---|---|
| Acute appendicitis | 18 (20%) | 18 (100%) | 0 (0%) | 0 (0%) |
| Grade I | 9 (11%) | |||
| Grade II | 3 (3%) | |||
| Grade III | 3 (3%) | |||
| Grade IV | 1 (1%) | |||
| Grade V | 2 (2%) | |||
| Acute cholecystitis | 16 (18%) | 9a (56%) | 2 (13%) | 5 (31%) |
| Grade I | 9 (10%) | 4 (44%) | 1 (12%) | 4 (44%) |
| Grade II | 5 (6%) | 4 (80%) | 0 (0%) | 1 (20%) |
| Grade III | 2 (2%) | 1 (50%) | 1 (50%) | 0 (0%) |
| Acute diverticulitis | 11 (12%) | 0 (0%) | 1 (9%) | 10 (91%) |
| Stage 0 | 4 (5%) | 0 (0%) | 4 (100%) | |
| Stage 1a | 2 (2%) | 0 (0%) | 2 (100%) | |
| Stage 1b | 2 (2%) | 0 (0%) | 2 (100%) | |
| Stage 2a | 2 (2%) | 1 (50%) | 1 (50%) | |
| Stage 2b | 1 (1%) | 0 (0%) | 1 (100%) | |
| Intestinal obstructionb | 9 (10%) | 8 (89%) | 0 (0%) | 1 (11%) |
| Subacute intestinal obstruction | 7 (8%) | 0 (0%) | 0 (0%) | 7 (100%) |
| Incarcerated hernia | 4 (5%) | 4c (100%) | 0 (0%) | 0 (0%) |
| Femoral | 3 (3%) | |||
| Inguinal | 1 (1%) | |||
| Umbilical | 1 (1%) | |||
| Obstructive colon neoplasm | 4 (5%) | 3d (75%) | 1e (25%) | 0 (0%) |
| Fournier's gangrene | 1 (1%) | 1 (100%) | 0 (0%) | 0 (0%) |
| Stenosing gastric neoplasm | 1 (1%) | 1 (100%) | 0 (0%) | 0 (0%) |
| Duodenal perforation | 1 (1%) | 1f (100%) | 0 (0%) | 0 (0%) |
The cause of the obstruction was found in the small intestine, except one case of chronic benign stenosis of the sigmoid colon.
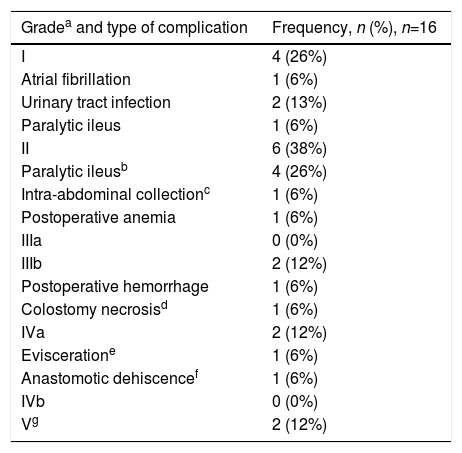
The median surgical time of the surgical procedures was 80 (P25–P75=55–110) minutes. Five (6%) patients required postoperative intensive care, with a mean stay in the ICU of 2.4±2 days. The postoperative complication rate 30 days after surgery was 31%. Six (12%) patients developed grade III or higher complications. Two (11%) patients died from postoperative complications. One of them, aged 91, experienced septic shock secondary to Fournier's gangrene. The other death was due to unknown cause in an 89-year-old woman after hospital discharge. Postoperative complications are summarized in Table 3. Median hospital stay was four days (P25–P75=2–6).
Postoperative complications between February 24 and April 18, 2020.
| Gradea and type of complication | Frequency, n (%), n=16 |
|---|---|
| I | 4 (26%) |
| Atrial fibrillation | 1 (6%) |
| Urinary tract infection | 2 (13%) |
| Paralytic ileus | 1 (6%) |
| II | 6 (38%) |
| Paralytic ileusb | 4 (26%) |
| Intra-abdominal collectionc | 1 (6%) |
| Postoperative anemia | 1 (6%) |
| IIIa | 0 (0%) |
| IIIb | 2 (12%) |
| Postoperative hemorrhage | 1 (6%) |
| Colostomy necrosisd | 1 (6%) |
| IVa | 2 (12%) |
| Evisceratione | 1 (6%) |
| Anastomotic dehiscencef | 1 (6%) |
| IVb | 0 (0%) |
| Vg | 2 (12%) |
Grade I: any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, or radiological interventions. The acceptable therapeutic regimens are: medications like antiemetics, antipyretics, analgesics, diuretics and electrolytes, as well as physical therapy. Grade II: the need for pharmacological treatment with different drugs than those permitted for grade I complications. Grado IIIa: procedure that is not done under general anesthesia. Grade IIIb: procedure under general anesthesia. Grado IVa: dysfunction of one organ (including dialysis), requiring intensive care treatment. Grado IVb: multiple organ dysfunction that requires intensive care management. Grado V: death.
The readmission rate in the first 30 days was 7%. Out of the six patients who were readmitted, two were positive for SARS-CoV-2 in the RT-PCR performed upon arrival at the emergency department on the day of readmission. In the first admission, both patients had negative RT-PCR. One patient underwent open adhesiolysis due to adherence syndrome with good postoperative evolution and was readmitted the same day of discharge due to fever without a source, finally being diagnosed with COVID-19. The other patient had been admitted to the Internal Medicine Service five days earlier due to fever and abdominal pain and discharged after negative RT-PCR for SARS-CoV-2. This patient was readmitted on the fifth day due to increased abdominal pain along with fecaluria and pneumaturia, resulting in a diagnosis of acute diverticulitis stage IIa by the World Society of Emergency Surgery (WSES).
In the study period, 18 acute appendicitis were diagnosed, and 50% presented an AAST stage≥II (which implies gangrene or perforation of the cecal appendix). All patients were operated on within 12 hours of diagnosis. Sixteen diagnoses of acute cholecystitis were made, 9 of which were treated with laparoscopic cholecystectomy, and seven (44%) had stage Tokyo≥II. Twenty-five patients were diagnosed with acute diverticulitis, 11 of which (44%) required admission. Urgent ultrasound-guided percutaneous drainage was performed in one case of acute diverticulitis, but no patient required urgent surgical intervention or another invasive procedure.
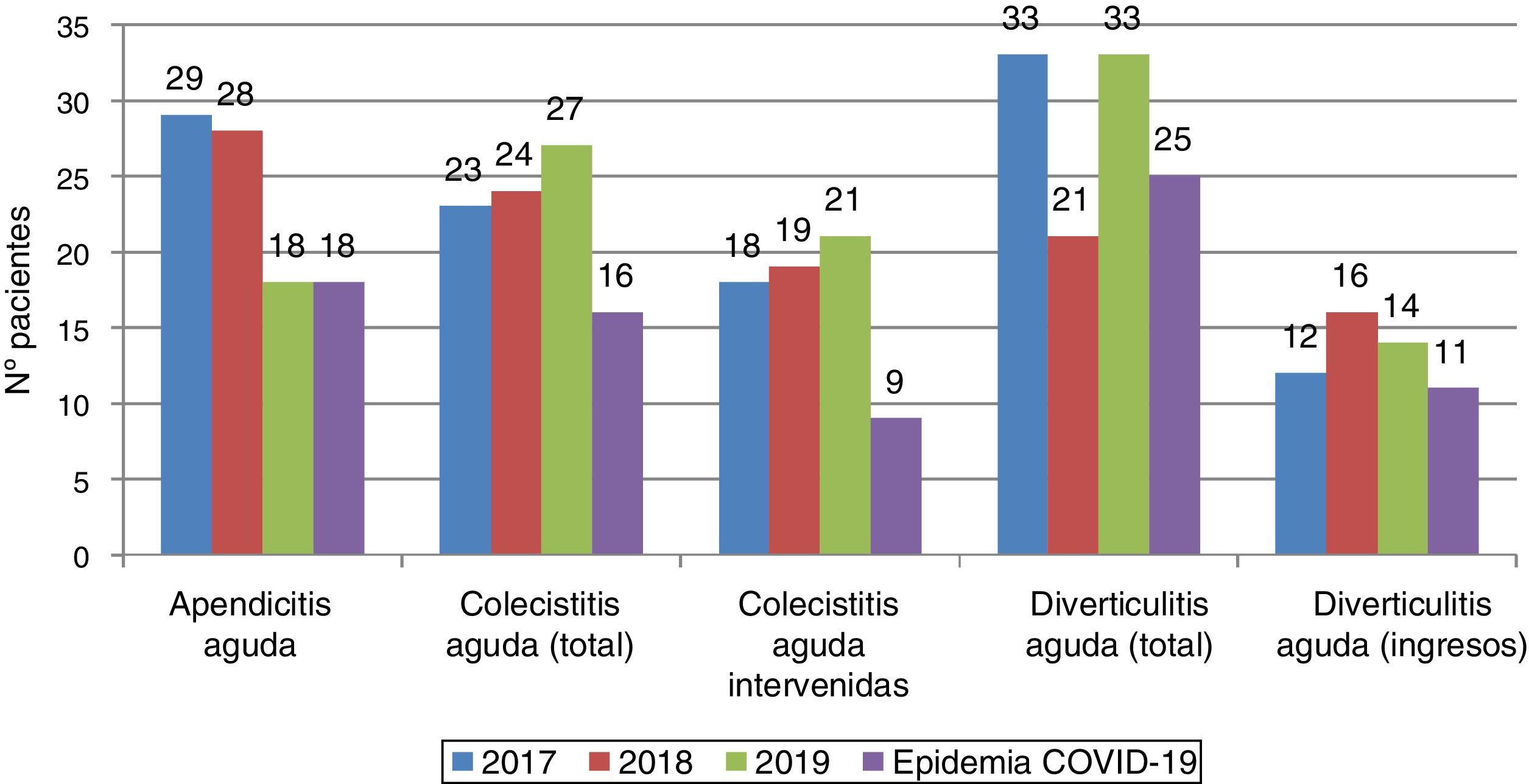
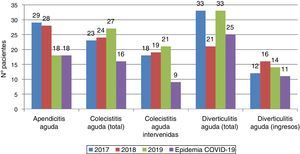
These data were compared with data of the most frequent potentially surgical pathologies in the Emergency Department of our hospital center for the same period in 2017, 2018 and 2019 (Fig. 1). The mean number of patients who required admission was 103.3±22 cases. A mean of 25±6 acute appendicitis were diagnosed, and 100% were treated by laparoscopic appendectomy. The mean number of acute cholecystitis diagnoses was 24.6±2 cases. All cases of cholecystitis required hospital admission, and 78% underwent laparoscopic cholecystectomy. A mean of 29±7 patients had a diagnosis of acute diverticulitis, with an admission rate of 48%. These figures represent a decrease of 14% in total hospital admissions, 22% in acute appendicitis diagnoses, 36% in acute cholecystitis admissions, 53% in cholecystectomies, 14% in acute diverticulitis diagnoses and 21% in admissions for diverticulitis. The rates of postoperative complications in 2017, 2018 and 2019 were 27% (Clavien-Dindo≥III 11%), 21% (Clavien-Dindo≥III 12%) and 29% (Clavien-Dindo≥III 11%), respectively. This represents a percentage increase of 13%, 32% and 6% compared to the previous three years, respectively, although with no differences in the percentage of serious postoperative complications.
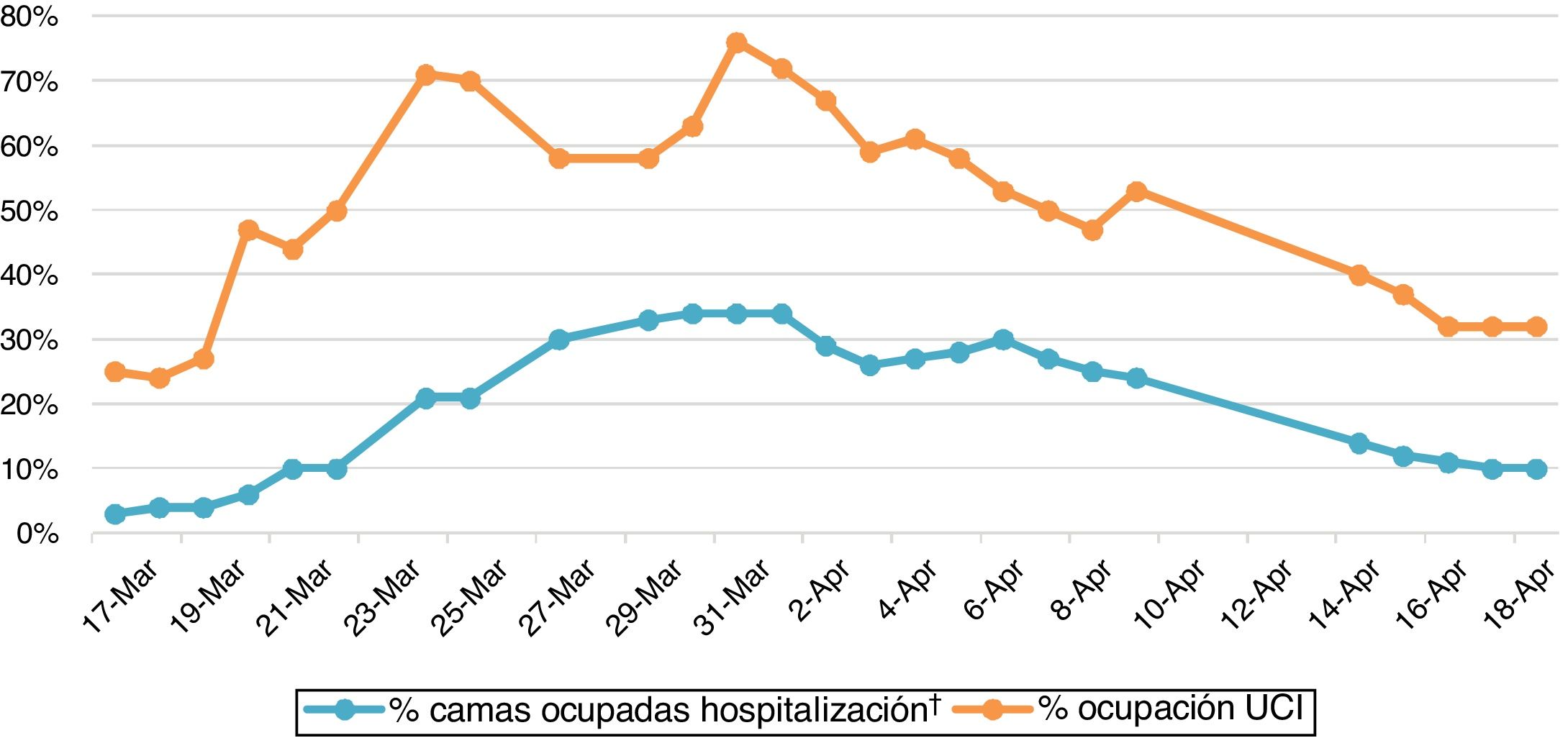
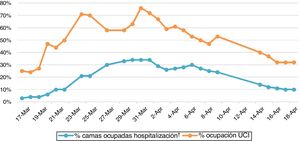
DiscussionCleary, the current COVID-19 epidemic has been a challenge for healthcare authorities, systems, hospitals, associations of all medical specialties and even for each of the professionals who work in them. As a consequence of focusing most healthcare resources on the treatment of patients affected by this disease, there is concern about not adequately managing other patients, both chronic and acute. Elective surgery has disappeared in many hospitals, and urgent surgical pathology management has been organized differently in each hospital depending on resources, healthcare pressure and instructions from health authorities. In our case, it was not until the declaration of the State of Alarm in Spain on March 14, 202012 that daily care activities were modified, as until then we were in phase I of the dynamic scale of alert phases/scenarios during the COVID-19 pandemic proposed by the Spanish Association of Surgeons.13 From that moment on, surgical activity was limited to emergencies and non-delayable cancer patients whose survival would be compromised without surgery (phase III), with ICU bed occupation by patients with confirmed diagnosis of SARS-CoV-2 infection around 25% and 10% of hospital beds. Less than a week later, the hospital was in phase IV and the occupancy of ICU and hospital beds experienced a rapid increase, reaching 76% and 34% on March 31, respectively (Fig. 2). During phase IV of the dynamic scale, surgical activity was limited to non-delayable urgent pathology. It is important to note that hospitalized patients diagnosed with COVID-19 usually remained isolated in individual rooms, so the real percentage of hospital occupancy would actually be double.
Epidemiological situation of COVID-19 at the Hospital Doctor Peset (Valencia) from March 17 to April 18, 2020.*
*Data provided by the Admissions Department (initiation of data collection: March 17, 2020).
†The actual percentage of hospital occupation would be double, as patients hospitalized with COVID-19 diagnosis remained isolated in individual rooms.
The results of our study show a 14% decrease in the number of patients who were admitted for urgent potentially surgical abdominal pathology at our hospital, and a uniform decrease was evident in both the number of total admissions as well as due to pathologies compared to previous years. Alvarez Gallego et al.5 described a decrease in activity in the emergency room of 52.7% and an increase in patients who presented peritonitis at a tertiary care hospital in the Community of Madrid. The same has occurred in other medical specialties, such as Cardiology or Neurology.14,15 The decrease in the number of cases could be due to the fact that mild cases have not been reported, as patients have suffered through the processes at home or have been treated by a Primary Care telephone consultation.
Although the median time of 2 days from the onset of the main symptom until the consultation is not excessively long, it does exceed the recommended time to initiate treatment of intra-abdominal infections.16 It should be noted that 20% of patients at that time had clinical and analytical criteria for SIRS. In the descriptive and multicenter INFURG-SEMES study analyzing the epidemiology of infections treated in hospital emergency departments between 2010 and 2011, the incidence of SIRS of abdominal origin was 15.35%, which is slightly lower than the rate observed in our study.17
Various scientific societies of surgeons have made a series of recommendations regarding therapeutic procedures during the pandemic, which contemplate the possibility of adopting a conservative approach toward certain pathologies.18 In our hospital, and based on these recommendations, treatment with intravenous antibiotic therapy was chosen in only five cases of acute cholecystitis in which the patients were candidates for urgent surgical intervention. The reluctance to opt for surgical treatment in certain groups is due to the suspicion that surgical aggression may induce an early systemic inflammatory response together with an immune alteration that could worsen the evolution of COVID-19 disease. In this context, Lei et al.19 published a retrospective study in which they described the results of 34 asymptomatic patients who underwent elective surgical procedures during the epidemic and who developed SARS-CoV-2 disease during the postoperative period. Their article suggested that surgery can accelerate and exacerbate progression of the disease, reaching a mortality rate of 20.5%. In a Spanish study, three patients underwent urgent surgical intervention with SARS-CoV-2 infection at the time of surgery or developed during the postoperative period, and the three of them died from respiratory failure.5 In our case, none of the patients undergoing surgical intervention with pre- or post-operative diagnosis of SARS-CoV-2 had any complications. In this period, our global morbidity and mortality rates were 22% and 2%, respectively.
Our study has several limitations. First of all, the sample size is small, although this is justifiable due to the recent appearance of COVID-19 disease. In addition, since it is a retrospective study with data obtained from computerized medical records, their interpretation may be subject to significant biases. We have also not analyzed the influence of the delay in starting treatment due to in-hospital diagnosis times, overloaded services, or the need to rule out COVID-19 infection. Furthermore, the epidemic status currently continues, and this study does not include the hypothetical social changes or the management protocols that may influence the actions of both patients and surgical specialists.
In conclusion, our study demonstrates a decrease in the number of patients who were admitted for urgent potentially surgical abdominal pathology during the COVID-19 epidemic at our hospital, both globally as well as by pathologies. It is essential for future studies to analyze the medium- and long-term repercussions of this exceptional situation, especially in terms of morbidity, mortality and oncological results, as these may possibly have a continued effect over time. The possible impact on the prognosis of cancer patients is a matter of concern for all medical professionals. Equally concerning is the effect on benign pathologies given that, if the current situation persists over time, increasingly frequent presentations of complicated surgical abdominal pathologies are expected.
FundingThis study has received no specific funding from public, commercial or non-profit organizations.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Pérez-Rubio Á, Sebastián Tomás JC, Navarro-Martínez S, Gonzálvez Guardiola P, Torrecillas Meroño DG, Domingo del Pozo C. Incidencia de la patología abdominal quirúrgica urgente durante la pandemia por SARS-CoV-2. Cir Esp. 2020;98:618–624.