Gastroesophageal reflux disease (GERD) is a complex entity and one of the most frequents in general population. Association of GERD with obesity is clearly defined from an epidemiological point of view, where up to 40% of patients with overweight and obesity present reflux. Most of the risk factors associated to GERD are shared and especially frequent in patients with obesity. The pathophysiology that explain this correlation is complex and multifactorial, and includes both aspects related to physiology of motility, and anatomic changes. The malfunction of the lower esophageal sphincter, the greater transdiaphragmatic pressure gradient, pathological accumulation of fat and the high rate of hiatal hernia that comes with overweight will be the main factors that explain this correlation. Other factor like pathological eating habits or obesity related diseases have also an important role. In summary, it is the sum of the factors more than just one of them what would explain the pathophysiology of GERD in obese population.
La enfermedad por reflujo gastroesofágico (ERGE) es una patología compleja y de las más frecuentes en la población general. La asociación con la obesidad está claramente definida desde un punto de vista epidemiológico, hasta un 40% de los pacientes con sobrepeso y obesidad presentan patología de reflujo. Muchos de los factores de riesgo de la ERGE son compartidos y especialmente frecuentes en pacientes con obesidad. La fisiopatología que explica esta correlación es compleja y multifactorial, e incluye aspectos relacionados con la fisiología de motilidad, así como alteraciones anatómicas. Las alteraciones del esfínter esofágico inferior, el aumento del gradiente transdiafragmático, los acúmulos patológicos de grasa y la elevada tasa de hernia de hiato que aparece con el sobrepeso serán los principales factores que explican esta correlación. También otros factores como alteraciones en la ingesta o patologías asociadas se han visto que tienen un peso importante. En resumen, se trata de una suma de factores más que de un solo factor el que explicaría la fisiopatología del ERGE en la población con obesidad.
Gastroesophageal reflux disease (GORD) is one of the most common gastrointestinal conditions in the general population.1,2 It has been reported that a significant proportion of the general population presents weekly symptoms of GORD, and this drives proton inhibitor drugs to be one of the most widely consumed families of medications. It is a complex disease and difficult to diagnose because there are different criteria, and because the symptoms are greatly discordant with the exploratory findings.3
Physiology and pathophysiology of gastro-oesophageal reflux diseaseIn order to understand the pathophysiology of this disease, it is necessary to first understand the physiology of the distal oesophagus and the gastro-oesophageal junction. The oesophagus measures approximately 25 cm and is composed of smooth and striated muscles. In the cervical oesophagus there is only striated muscle, smooth in the abdominal and in the rest both are present. During swallowing, the coordination of these muscles propels the bolus towards the stomach.4
Antireflux mechanisms are necessary to preserve the oesophageal mucosa from contact with the acidic pH of the gastric contents, to facilitate the correct advancement of the bolus and because the thoracic pressure is negative, unlike the abdominal pressure, which is positive, being the gradient of up to 10 mm Hg. In the abdominal oesophagus, the smooth muscLOS of the distal oesophagus, together with the lower oesophageal sphincter (LOS), constitute one of the intrinsic antireflux mechanisms. Other extrinsic mechanisms are the diaphragmatic or crural sphincter, the angle of His, the phrenoesophageal ligament and the mucosal rosette of the esophagogastric junction (OGJ).5
The LOS is formed by circular smooth muscles that have a maintained tone that keeps the sphincter closed. The coordination of the swallowing and propulsive movements of the oesophageal muscles, together with the controlled opening of the LOS, allows the passage of food and prevents the retrograde passage of the bolus, as well as the gastric acid content.5
The main abnormality observed in GORD is a dysfunction of the OGJ and its antireflux mechanisms.6 When there is inadequate relaxation of the LOS that allows acid to pass into the oesophagus, reflux symptoms begin. Despite this apparently simple explanation, the barrier function of the OGJ is influenced by multiple factors, such as the position of the person, respiratory movements, gastric contents, etc.
Pathogenesis of gastroesophageal refluxMultiple mechanisms have been described in the pathogenesis of GORD, all of them interconnected but with no determination of which of them is the most significant. The different studies that evaluate this pathophysiology generally focus on assessing one or another of them. There are few studies that assess them more globally.7 Essentially, GORD is the result of the failure of antireflux mechanisms that protect the oesophagus from harmful gastric contents.8
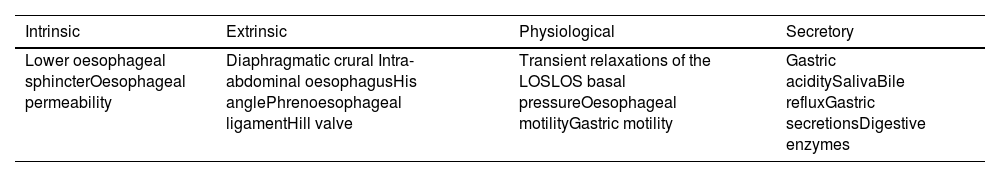
The pathophysiological mechanisms of reflux can be divided into intrinsic, extrinsic, physiological and secretary (Table 1).
Main physiopathological mechanisms.
| Intrinsic | Extrinsic | Physiological | Secretory |
|---|---|---|---|
| Lower oesophageal sphincterOesophageal permeability | Diaphragmatic crural Intra-abdominal oesophagusHis anglePhrenoesophageal ligamentHill valve | Transient relaxations of the LOSLOS basal pressureOesophageal motilityGastric motility | Gastric aciditySalivaBile refluxGastric secretionsDigestive enzymes |
Adapted from Banting et al.8
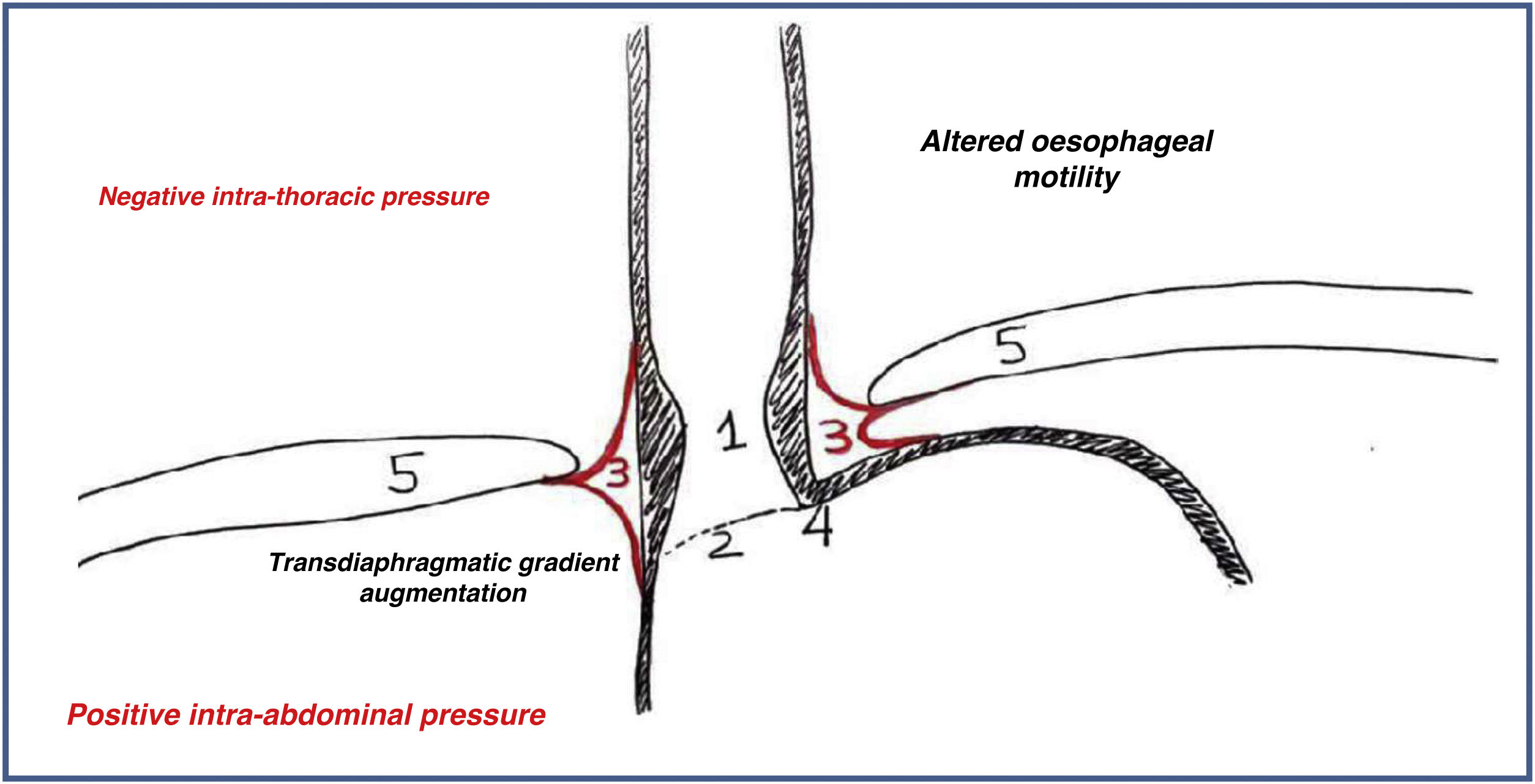
Of all the previously described mechanisms, there is consensus in recognising that the most significant are those detailed below (Fig. 1):
- -
Weakness of the LOS. The lack of tone of the LOS makes it easier for gastric acid to return to the oesophagus.
- -
Altered frequency of transient relaxations of the LOS. This appears in the vast majority of patients suffering from GORD without associated anatomical alteration. It is defined as a relaxation of the LOS independent of the swallowing process, not accompanied by peristalsis, together with diaphragmatic inhibition, and together with persistence of relaxation of the LOS after swallowing.
- -
Anatomical alterations of the OGJ
Alteration of the Hill valve or oesophagogastric flap is a generally poorly recognised cause. It is formed by the intra-abdominal extension of the angle of His that rests on the lower gastric curvature and allows the unidirectional passage of the bolus.
Hiatus hernia is a fundamental mechanism in the appearance of GORD. The movement of the OGJ towards the thorax disrupts the LOS and its functionality. Furthermore, the change in extrinsic pressures hinders the other intrinsic mechanisms and facilitates the return of gastric contents towards the oesophagus.
- -
Oesophageal motility disorders. Dysfunction of oesophageal peristalsis is directly related to the severity of oesophagitis. The level of acid exposure of the oesophagus is directly related to its altered or weak motility.9
- -
Alterations in gastric motility or emptying
Other risk factors that have been associated with the appearance of reflux have also been described, among which the following stand out4:
- -
Family history.
- -
Pregnancy.
- -
Low educational level.
- -
Tobacco.
- -
Alcohol.
- -
Obesity.
- -
Diabetes.
- -
Cardiovascular comorbidities.
- -
Psychiatric comorbidities.
- -
Gastrointestinal comorbidities.
- -
Anticholinergic drugs.
- -
Nitrate
- -
Hiatus hernia.
- -
Oesophageal dysmotility.
- -
Delayed gastric emptying.
Obesity is one of the great epidemics of the 21 st century. The correlation between obesity and GORD is of great relevance due to the high prevalence of symptoms related to this disease in overweight and obese patients,10 and because they can significantly condition the indication for bariatric surgery, both in the indication itself and in the surgical technique. The pathophysiological mechanisms are not clearly defined, but we can find that obesity is clearly related to many of the predisposing factors to GORD.9
Changes of motilityIn overweight patients, alteration of the LOS is not always observed; in fact, some studies reveal a greater tone of the LOS as a compensatory mechanism in cases of overweight.8 These findings are also contradictory in the literature, since some series describe precisely the opposite.11
In contrast, a greater number of episodes of transient relaxation of the LOS has been observed. This higher rate of transient relaxation episodes has been associated with both body mass index (BMI) and abdominal circumference. Greater fat consumption stimulates the production of secretin and cholecystokinin that promote relaxation of the LOS.
The alteration of oesophageal motility, evaluated by high-resolution manometry, shows that up to a quarter of patients with obesity may present some type of alteration, mainly in the form of emptying obstruction.12 Associated diseases, alterations in intake and other factors may be responsible for this finding.8
With all these findings, systematic manometric studies in patients who are candidates for bariatric surgery have not been shown to have an indication.13 Although symptoms suggestive of GORD have been correlated with a higher incidence of pathological studies, there is still not enough evidence to systematically indicate them in this population.
Bariatric surgery causes alterations in motility to a greater or lesser extent depending on the technique performed. A debate is opened here about whether the presence of preoperative symptoms, the surgical technique to be performed and/or other factors to be determined may be sufficient reason to require these studies prior to surgery.10
Anatomical alterationsObesity is correlated with a larger abdominal circumference, and this causes an increase in intra-abdominal pressure and transdiaphragmatic gradient, both factors clearly related to the appearance of GORD. Furthermore, it is important to remember that there is a clear association of a higher prevalence of hiatus hernia in overweight patients.
The transdiaphragmatic pressure gradient does not correlate with BMI, but rather with the distribution of excess adiposity.14 Central obesity (larger waist circumference) is a critical factor in the development of a greater transdiaphragmatic pressure gradient. This factor is also correlated with slowed oesophageal transit. Patients with peripheral fat distribution do not show as much correlation with the appearance of GORD.
Hiatus hernia can appear in up to 40% of obese and overweight patients.15 This anatomical alteration disables the main intrinsic and extrinsic antireflux mechanisms. In this sense, the high correlation between both entities means that the use of preoperative upper gastrointestinal endoscopy is systematically recommended.16
The anatomical changes in the His angle11 in overweight patients, mainly mediated by the accumulation of fat, modify this angulation and, together with the other anatomical and functional factors previously described, cause a greater predisposition to GORD.
Other factorsHormonal changes that correlate with excess weight and altered diet in obese patients also appear to play a role in the pathogenesis of GORD. Elevated leptin levels seem to correlate with greater severity of GORD. On the other hand, ghrelin levels correlate inversely.8,11 The excess fat consumption that usually appears in patients with obesity increases the secretion of cholecystokinin, which induces relaxation of the LOS and increases episodes of transient relaxation of the same. Also, increased consumption of carbonated drinks, fats and other less healthy foods alter gastrointestinal motility, reducing gastric emptying and facilitating reflux episodes.
Among the predisposing factors to GORD, it has been described that diseases such as diabetes or alterations in intake are clear risk factors. Up to 25% of overweight and obese patients have type 2 diabetes as part of their metabolic síndrome.17 Sleep apnoea has also been correlated with a higher frequency of GORD. The exact pathophysiological mechanisms are unknown. Reflux episodes in these patients are characteristically more frequent at night, so it is suspected that they may possibly be correlated with pressure changes in the chest and abdomen that appear during periods of apnoea.
There is also a correlation between obesity and the abuse of substances such as alcohol and tobacco, both clear risk factors for GORD.17 Likewise, obesity is also more frequent in population groups with a lower level of education and income.
SummaryThe pathophysiological relationship between obesity and GORD is a multifactorial, complex entity, many pathophysiological factors of which remain unknown. The increased prevalence of GORD in overweight patients can be explained by both anatomical and functional alterations. It is the sum of factors rather than one factor above another, with excess weight and abnormal fat accumulation being the triggering issues of this entire chain.
Conflict of interestsThe authors have no conflict of interests to declare
Please cite this article as: García Ruiz de Gordejuela A, Ibarzabal Olano A, Petrola Chacón CG, González López Ó. Aspectos fisiopatológicos de la obesidad que favorecen la aparición de Enfermedad por reflujo gastroesofágico. Cir Esp. 2023. https://doi.org/10.1016/j.ciresp.2022.12.007