Overweight and obesity are a public health problem and in 1997 obesity was recognized as a global epidemic by the World Health Organization (WHO). Overweight and obesity affect almost 60% of adults and one in three children in Europe according to the most recent WHO report. Objectively, gastroesophageal reflux disease (GERD) is defined as the presence of characteristic esophageal mucosal damage assessed by endoscopy and/or the demonstra-tion of pathological acid exposure by reflux monitoring studies. The prevalence of GERD is increased in obese patients
In overweight and obese patients, the clinical symptoms of GERD are especially present in the supine position and this correlates with more frequent episodes of nocturnal reflux in the 24-h pH monitoring, there is also an increase in the number of refluxes with content acid. In the population with symptoms, digestive endoscopy detects data of erosive esophagitis in 50% of patients, while 24-h pH-impedanciometry diagnoses 92% of patients with non-erosive reflux disease (NERD)
The presence of persistent GERD in the mucosa affects esophageal motility and patients may develop ineffective esophageal motility-type disorders, so we will review the interpre-tation of the functional tests that determine motility, which is esophageal manometry, and those that determine reflux gastroesophageal, acid and non-acid, which is the pH measure-ment with or without 24-h impedanciometry.
El sobrepeso y la obesidad son un problema de salud pública y en 1997 la obesidad fue reconocida como una epidemia global por la Organizacio’n Mundial de la Salud (OMS). El sobrepeso y la obesidad afectan a casi un 60% de los adultos y a uno de cada 3 niños del territorio europeo según el informe más reciente de la OMS. De forma objetiva, la enferme-dad por reflujo gastroesofágico (ERGE) se define como la presencia de un daño mucoso esofágico característico evaluado por endoscopia y/o la demostración de una exposición al ácido patológica mediante estudios de monitorización del reflujo. La prevalencia de la ERGE está aumentada en los pacientes con obesidad
En los pacientes con sobrepeso y obesidad, la sintomatología clínica de la ERGE se presenta especialmente en posición en supino y esto se correlaciona con episodios más frecuentes de reflujo nocturno en la pHmetría de 24 h; existe también un incremento en el número de reflujos con contenido ácido. En la población con sintomatología la endoscopia digestiva detecta datos de esofagitis erosiva en un 50% de los pacientes, mientras que la pH impedanciometría de 24 h diagnostica el 92% de los pacientes con enfermedad por reflujo no erosiva (ERNE).
La presencia de ERGE persistente en la mucosa afecta la motilidad esofágica y los pacientes pueden desarrollar trastornos de tipo motilidad esofágica ineficaz, por lo que revisaremos la interpretación de las pruebas funcionales que determinan la motilidad, que es la manometría esofágica, y las que determinan el reflujo gastroesófagico, ácido y no ácido, que es la pHmetría con o sin impedanciometría de 24 h.
The pathogenesis of gastro-oesophageal reflux disease (GORD) is complex and involves changes in reflux exposure, oesophageal epithelial resistance, and visceral sensitivity.1 Under normal circumstances, the passage of gastric contents into the oesophagus is prevented by the oesophagogastric junction (OGJ), which forms an anti-reflux barrier. The OGJ is made up of several anatomical structures that play an important role in maintaining the anti-reflux barrier. The lower oesophageal sphincter (LOS) and the crural diaphragm (CD) constitute the intrinsic and extrinsic sphincter, respectively. Under normal conditions the two sphincters overlap and are anchored to each other by the phrenoesophageal ligament.1
Incompetence of the anti-reflux barrier- 1
Transient lower oesophageal sphincter relaxation "TLOSR": TLOSR is the major mechanism underlying gastro-oesophageal reflux (GOR). Most reflux episodes occur during TLOSR episodes. TLOSRs are episodes of complete and prolonged relaxation of the LOS, not triggered by swallowing and accompanied by CD inhibition.2,3 A set of manometric criteria for TLOSRs have been proposed: a main criterion, relaxation of the LOS for more than 10 s in the absence of swallowing 4 s before and 2 s after LOS relaxation and several additional criteria, presence of reflux by means of manometry-impedance monitoring, oesophageal shortening, single cavity phenomenon, crural diaphragm inhibition, relaxation of the upper oesophageal sphincter (UOS) without subsequent swallowing, and secondary peristalsis.2
- 2
Hypotension of the LOS and GOR induced by abrupt increases in intragastric pressure in the context of a hypotensive LOS (<10 mmHg (<10 mmHg).1,2
- 3
Anatomical abnormalities of the OJG. In patients with hiatal hernia, the function of the crural diaphragm is compromised by its axial displacement and atrophy secondary to dilatation of the diaphragmatic hiatus. In addition, the presence of a hiatal hernia leads to a decrease in the intraluminal pressure of the OJG favouring reflux episodes.2
- 4
Impaired oesophageal clearance. Prolonged exposure of the oesophageal mucosa to gastric juice correlates with the severity of erosive oesophagitis and the presence of Barrett's oesophagus.4 The two main causes of prolonged reflux exposure and impaired oesophageal clearance are defects in oesophageal peristalsis and saliva production. Impaired oesophageal emptying and retrograde flow phenomena of reflux gastric contents are also present in patients with hiatal hernia.5
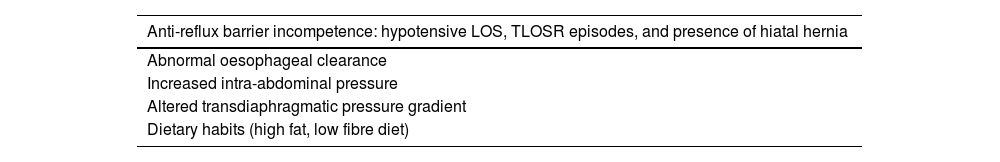
In patients with obesity, an increase in intra-abdominal pressure has been identified in patients with obesity, due to the transmission of gravitational force from the adipose tissue to the abdominal cavity favouring reflux episodes through abrupt increases in intragastric pressure.5 The gastric volume of obese patients is higher than in the normopese population, which could favour reflux episodes of higher volume. Another theory is that obese patients may have slowed gastric emptying, due to neural and humoral mechanisms, and that this favours the presence of GORD.5 Obese patients have a higher incidence of hiatal hernia, with figures of up to 50%, which is also associated with an increased risk for GORD.6 It has been shown that TLOSR is more common in obese patients than in normal weight patients, and in one published series of patients in up to 51% of obese patients manometry revealed dysmotility.6 The underlying mechanisms of GORD in obese patients are described in Table 1.
Underlying mechanisms of GORD in obese patients.
| Anti-reflux barrier incompetence: hypotensive LOS, TLOSR episodes, and presence of hiatal hernia |
|---|
| Abnormal oesophageal clearance |
| Increased intra-abdominal pressure |
| Altered transdiaphragmatic pressure gradient |
| Dietary habits (high fat, low fibre diet) |
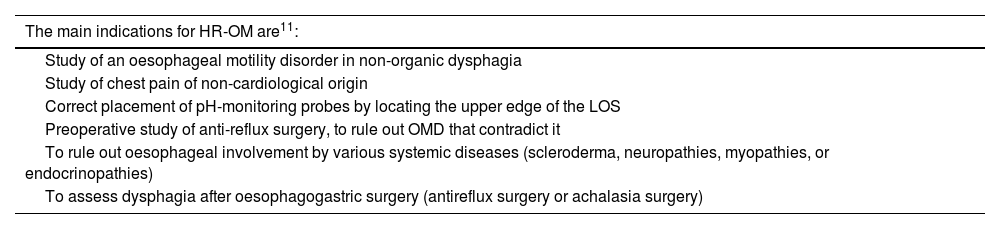
Oesophageal manometry is the technique for studying and quantifying the contractile motor activity of the oesophagus and is therefore the technique of choice for the diagnosis of oesophageal motility disorders (OMD). HR-OM assesses oesophageal motility patterns by measuring the amplitude of the contractile events of the oesophagus and its sphincters in relation to time by means of pressure sensors located along the catheter.7 HR-OM probes have 36 pressure sensors spaced 1 cm apart. These sensors collect dynamic information and, using computer software, it is transformed into spatio-temporal graphs called oesophageal pressure topography (OPT).7 A standardised protocol is used to interpret OPT as described in Chicago Classification v 4.0.8 The indications for HR-OM are described in Table 2.
Indications for high-resolution oesophageal manometry.
| The main indications for HR-OM are11: |
|---|
| Study of an oesophageal motility disorder in non-organic dysphagia |
| Study of chest pain of non-cardiological origin |
| Correct placement of pH-monitoring probes by locating the upper edge of the LOS |
| Preoperative study of anti-reflux surgery, to rule out OMD that contradict it |
| To rule out oesophageal involvement by various systemic diseases (scleroderma, neuropathies, myopathies, or endocrinopathies) |
| To assess dysphagia after oesophagogastric surgery (antireflux surgery or achalasia surgery) |
The study starts with the patient in the supine position, after intubation of the manometry catheter via the transnasal route. Once the catheter is in place, a 60-second stabilisation period is required, followed by 3 deep breaths to confirm placement and the passage of at least 3 sensors from the distal end of the catheter into the gastric chamber. The resting pressure is then recorded for 30 s to identify anatomical landmarks: the upper oesophageal sphincter (UOS) and lower oesophageal sphincter (LOS), the respiratory inversion point (RIP) and the baseline OJG pressure. This is followed by 10 swallows of 5 ml water or saline. The protocol is completed with the patient supine and with the multiple swallow test, by administering 5 liquid swallows of 2 ml with 2–3 seconds between each swallow.9 The aim of this test is to assess peristaltic reserve. Once this part is completed, the patient is placed upright, and the resting pressure is performed again for 30 s. Five liquid swallows of 5 ml are performed with at least 30 s between each swallow and finished with the 200 ml liquid overload test, to determine the presence of brief obstructive or hyperpressive patterns in case of impaired motility or relaxation of the LOS.10
Manometric study of swallowingTo assess and classify swallowing, certain parameters have to be calculated on the OPT: the integrated relaxation pressure (IRP), a measure of LOS relaxation of swallowing. Oesophageal contractile function through the distal contractile integral (DCI), which measures the strength of oesophageal contraction, distal latency (DL), a measure of time to identify premature or spastic waves, and peristaltic integrity, which describes the presence or absence of fragmented peristaltic waves. The HR-OM allows for the assessment of intra-oesophageal pressurisation patterns. Oesophageal pressurisation occurs when swallowed fluid is trapped between two contracting oesophageal segments.8Table 3 shows the classification of OMDs.
Chicago Classification v4.0 for oesophageal motility disorders.
| Oesophagogastric junction outflow tract obstruction | ||
|---|---|---|
| Median IRP above upper limit of normal | ||
| Achalasia type I | 100% failed peristalsis | |
| Achalasia type II | 100% failed peristalsis and ≥20% of swallows with pan-oesophageal pressurisation | |
| Achalasia type III | Absence of peristalsis and ≥ 20% swallows with premature waves (distal latency <4.5 s) | |
| Oesophagogastric junction outflow tract obstruction | Evidence of oesophageal peristalsis | |
| Disordered oesophageal peristalsis | ||
| Median IRP within normal limits | ||
| Absent contractility | 100% failed peristalsis | |
| Ineffective oesophageal motility | ≥50% of swallows with failed waves or >70% of swallows with ineffective waves (weak or fragmented) | |
| Distal oesophageal spasm | ≥20% of swallows with premature waves (DL < 4.5 s) | |
| Hypercontractile oesophagus | ≥20% of swallows with hypercontractile waves (DCI>8000mmHg*s*cm) | |
| Normal | ||
| Normal oesophageal motility | None of the above criteria | |
The OGJ has unique characteristics that make manometric assessment challenging. First, the OGJ pressure comprises the pressure of the LOS and the CD. Second, its morphology is influenced by the anatomical integrity of the OGJ, which is affected in the presence of a hiatal hernia, and the arrangement of the LOS and CD is dynamic, one manometric recording can identify from the overlap of both elements to the presence of an overt hiatal hernia. Third, the OGJ shows marked radial and axial asymmetry in pressure morphology.7 Finally, when the LOS and CD are separated, the RIP, which is where the pressure change occurs during inspiration from negative intrathoracic pressure to positive intragastric pressure, can be located above the LOS or between the CD and LOS. There is evidence that the relative location of the RIP to the LES is more associated with pathological oesophageal acid reflux exposure than the presence and size of the hiatal hernia.7,8
The Chicago Consensus version 4 classifies the OGJ into three subtypes according to morphology8:
- •
Type 1, absence of hiatal hernia: overlapping LOS and CD, separation <1 cm.
- •
Type 2, hiatal hernia with the RIP proximal to the CD: separation of the LOS and CD>1 cm and RIP between CD and LOS.
- •
Type 3, hiatal hernia with the IRP proximal to the LOS: separation of the LOS and CD>1 cm and RIP above the LOS.
HR-OM and impedance allows simultaneous assessment of oesophageal movements through HR-OM and the transit of the swallowed bolus by means of impedance without the need for radiological studies.11 Good correlation has been demonstrated in the measurement of bolus transit and oesophageal clearance measured by impedance versus videofluoroscopy considered the gold standard.12 The basic principle of impedance measurements is to evaluate the resistance to the passage of an alternating current between two electrodes. The resistance to the passage of the current is influenced by the conductive medium.13 During saline swallowing, as it is a good conductor, the impedance decreases as the bolus progresses, returning to its baseline value once the bolus is cleared, allowing assessment of whether the bolus transit is complete or incomplete or whether it is retained.14
Manometry in GORDHR-OM should always be requested for GORD prior to placement of the pH-monitoring probe to locate the LOS and its correct placement. HR-OM allows the identification of GORD-associated OMD and correct differential diagnosis with other oesophageal diseases that may present the same symptoms as GORD, such as achalasia or other primary OMD. In addition, an HR-OM should be requested in all patients who are candidates for surgical and/or endoscopic anti-reflux techniques to confirm the diagnosis and assess peristaltic reserve.15 Up to one third of patients classified as refractory GORD do not have GORD and present with other disorders, most commonly functional heartburn, but they sometimes present findings compatible with achalasia or rumination syndrome.16
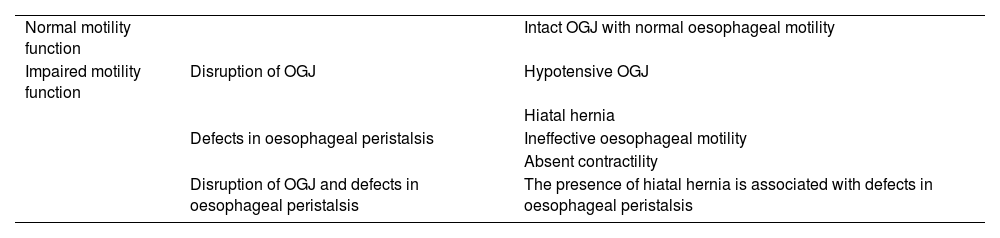
According to the international consensus on the classification of motility disorders in GORD, two motor phenotypes are identified in GORD,17 which are described in Table 4.
Motility phenotypes of GORD.
| Normal motility function | Intact OGJ with normal oesophageal motility | |
| Impaired motility function | Disruption of OGJ | Hypotensive OGJ |
| Hiatal hernia | ||
| Defects in oesophageal peristalsis | Ineffective oesophageal motility | |
| Absent contractility | ||
| Disruption of OGJ and defects in oesophageal peristalsis | The presence of hiatal hernia is associated with defects in oesophageal peristalsis |
Hypomotility-type oesophageal disorders are the most common of the GORD-associated MODs, although spastic disorders (OH and DOS) have also been associated with pathological exposure of the oesophagus to gastric reflux. Up to 38% of patients diagnosed with DOS have pathological acid exposure according to the largest published series,18 and 43% of patients with OH have typical GORD symptoms.19
The international consensus on the classification of motility disorders in GORD proposes a three-step algorithm to characterise oesophageal motility function in the context of GORD study and assessment prior to antireflux surgery. The first step is to assess the integrity of the OGJ, the second step is to assess oesophageal body motility function, and finally to assess the contractile reserve by means of provocative tests.17 The presence of a contractile wave following the multiple swallow test with contractile force, as assessed by DCI (mmHg), greater than the mean of the 10 liquid swallows indicates the presence of contractile reserve and a lower risk of post-fundoplication dysphagia.20 The solid swallow test is another complementary test used to assess contractile reserve. Contractile reserve is considered present if the strength of the peristaltic wave generated after swallowing the solid (a piece of bread or biscuit) is greater than the average of the 10 liquid swallows. A good correlation has been demonstrated in the assessment of contractile reserve with the multiple swallow test and solid swallows in patients meeting manometric criteria for ineffective oesophageal motility. The increased risk for developing post-fundoplication oesophageal symptoms in patients without contractile reserve in both tests has also been confirmed.10–20 The solid swallow test is complementary to the multiple swallow test in assessing peristaltic reserve and predicting the risk of developing post-fundoplication dysphagia.21
Manometric findings in overweight/obese patientsIn patients with obesity, increased abdominal girth plays a key role in the pathophysiological mechanisms of GORD. Obese patients have disruptions in both the barrier effect of the OGJ and oesophageal peristalsis. A negative association between BMI, LOS pressure and the intra-abdominal segment of the LOS has been demonstrated. Overweight and obese patients more frequently present with hypotensive LOS and disrupted OGJ in the form of hiatal hernia.22 Obese patients have higher intragastric pressure than non-obese patients23; and there is a positive correlation between BMI and intragastric pressure. The gastro-oesophageal pressure gradient is also found to be increased in overweight or obese patients compared to normopese patients.24 Obese patients have a higher number of TLOSR episodes during the postprandial period (2 h after a meal), 7 episodes compared to 2 episodes in the control group.25 In the supine position, patients with obesity often have an IRP above the limit of normal, which, when changing position to upright, becomes within the normal range. In a recent study, 75% of patients with a diagnosis of oesophagogastric junction outflow obstruction (OGJOO) with elevated supine IRP, after evaluation of IRP in both positions, a diagnosis of OGJOO was excluded. The hypothesis for this increase in supine IRP values is that the effect of gravity on abdominal fat increases intra-abdominal pressure and pressure on the OGJ.23 In a cohort of 147 patients with obesity underwent HR-OM and OMD was identified in up to 34%, according to the Chicago classification version 3.26 A total of 18.4% had a manometric diagnosis of OGJOO, 7.5% of HO, 4.1% of DOS, 2% of IOM, and 1.4% of fragmented peristalsis.27
Manometry findings in patients undergoing bariatric surgeryVertical gastrectomy or gastric sleeve is one of the most commonly used surgical techniques in bariatric surgery. Vertical gastrectomy is a restrictive technique that involves a reduction in gastric volume and gastric accommodation, which leads to an increase in intragastric pressure that favours the onset of upper GI symptoms.28 In patients undergoing vertical gastrectomy, an increase in intragastric pressure above 30 mmHg during LOS contraction after single swallows is characteristic on HR-OM.28 Hypomotility disorders in oesophageal peristalsis occur after vertical gastrectomy, with a decrease in the mean DCI of the 10 liquid swallows and an increase of more than 30% of de novo diagnosis of ineffective oesophageal motility.29
Assessment of gastro-oesophageal reflux in obese patientsIn the symptomatic population, gastrointestinal endoscopy detects erosive oesophagitis in 50% of patients, while 24 h pH-impedance monitoring diagnoses 92% of patients with non-erosive reflux disease (NERD).30
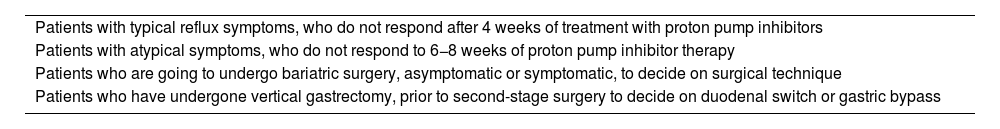
Table 5 defines the indications for 24 h pH-impedance monitoring.
Indications for 24-hr pH impedance monitoring.
| Patients with typical reflux symptoms, who do not respond after 4 weeks of treatment with proton pump inhibitors |
| Patients with atypical symptoms, who do not respond to 6−8 weeks of proton pump inhibitor therapy |
| Patients who are going to undergo bariatric surgery, asymptomatic or symptomatic, to decide on surgical technique |
| Patients who have undergone vertical gastrectomy, prior to second-stage surgery to decide on duodenal switch or gastric bypass |
Twenty-four-hour oesophageal pH monitoring in off-PPI (without proton pump inhibitor [PPI] treatment) is the diagnostic benchmark and consists of the recording of oesophageal acidity levels using a probe with acid-sensitive receptors and a computer recording the results. Table 6 describes the variables to be measured in pH monitoring.
Variables to be measured in pH monitoring.
| Number of reflux episodes with reflux below pH 4.0, normal <80 |
| Number of refluxes with duration longer than 5 min, ≤3 |
| Duration of longest reflux, <9.2 min |
| Total time of mucosal exposure to acid (minutes) |
| Percentage of time of mucosal exposure to acid, <4.2% |
| Reflux rate (reflux/hour) |
| Mean oesophageal clearance time (minutes/refluxes) |
| Assessment of symptom correlation (SI) and symptom association probability (SAP) |
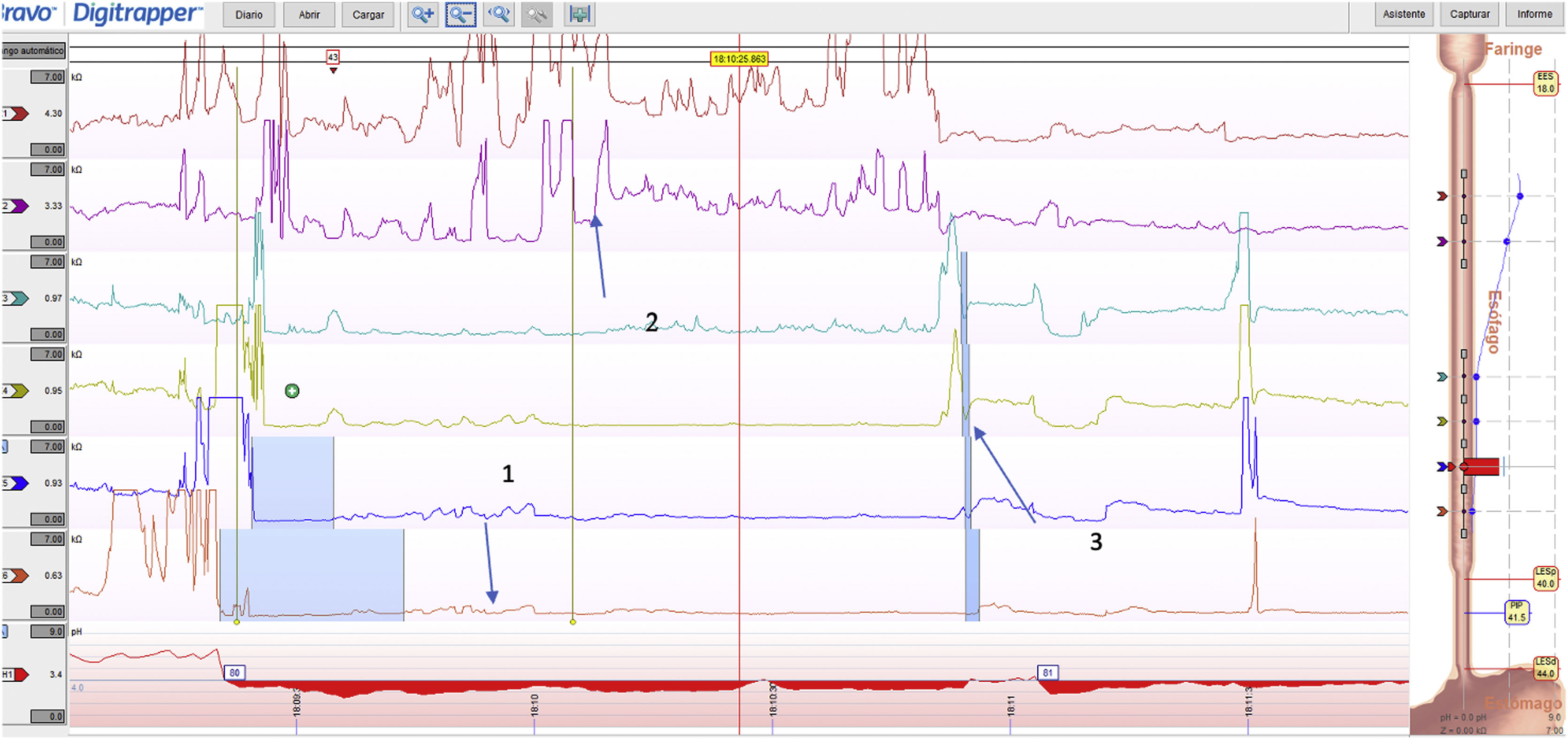
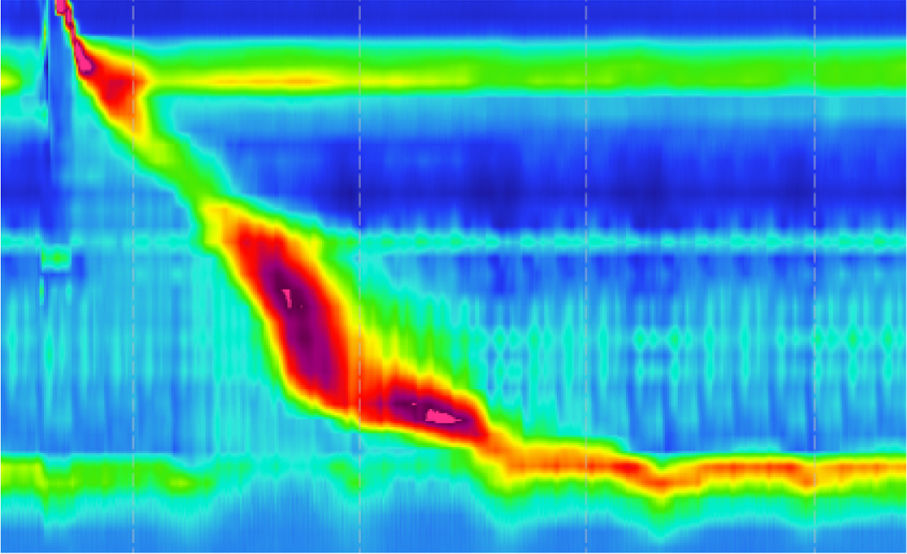
To test the pathophysiological relationship between obesity and reflux, objective data have been evaluated with pH monitoring, but these results have been contradictory because patients with obesity are more likely to have OGJ disruption31 and an increased gastro-oesophageal pressure gradient, which provides a perfect scenario for reflux to occur. There are patients with obesity who do not have reflux and are asymptomatic,32 the pH recording in the distal oesophagus in asymptomatic individuals shows the presence of occasional episodes of reflux, compatible with physiological reflux which is characterised by episodes of reflux of short duration predominantly in the standing position. A pathological reflux is shown in Fig. 1.
Pathological reflux. The numerical bar on the left shows the pH value from 0 to 8; the red line delimits a pH lower and higher than 4, to determine the episodes of pathological acid reflux with pH < 4, which corresponds to the critical point of the deleterious effect of acid and pepsin. The lower scale shows the hours during which the recording was made, and the yellow bars delimit the times at the beginning and end of meals; the time the patient was in the supine position during sleep can also be measured (green box). In this graph there is a percentage of time with a pH < 4 of 14.8%, with 100 reflux episodes, of short duration due to correct oesophageal clearance. The longest reflux lasted 3 min and a DeMeester score of 15.1.
Multichannel intraluminal impedance-pH-monitoring (pHz) has the advantage of simultaneously detecting both acid and non-acid reflux, as well as its characteristics which can be liquid, gas, or mixed and the direction of the refluxed material which can be either retrograde or antegrade. With pHz monitoring it has been shown that patients with obesity have more gastro-oesophageal reflux.33
The indications for pHz are:
- 1
To quantify and characterise oesophagogastric reflux, especially in patients with incomplete response or no response to suppressive therapy with proton pump inhibitors and who have previously undergone endoscopic study and show no disruptions.
- 2
To evaluate the patient with symptoms of atypical reflux or extra-oesophageal manifestations of reflux, such as pharyngeal globus, cough, and dysphonia.
- 3
To evaluate acid and non-acid reflux in patients undergoing bariatric surgery or after second-stage bariatric surgery.
pHz is performed technically in the same way as conventional pH-monitoring. The patient needs to fast for 6 h, an HR-OM is performed beforehand to determine how many centimetres away the upper edge of the LOS is located and 5 cm is subtracted from that measurement, because the site where peptidases are inactivated is at that height.
The characteristics to be evaluated are:
Composition of reflux: impedance monitoring helps classify reflux episodes as gas, liquid, or mixed. Air is a poor conductor and therefore has a high impedance, whereas liquid, which is a good conductor, has a low impedance.
Proximal reflux: The proximal extent of an episode is defined by the most proximal impedance measurement segment reached by the liquid component of the reflux episode. Gas reflux episodes are not assigned a proximal extent, as they typically enter the upper oesophageal sphincter and are eliminated.
Number of acid and non-acid reflux episodes: the combination of pHz defines the number of reflux episodes with change in impedance monitoring as well as the total number of episodes detected by impedance monitoring alone without pH alteration.
Reflux contact time: this determines the presence of reflux time, which is the total amount of time of refluxed material detected by impedance monitoring from the segment located 5 cm above the LOS.
Oesophageal clearance time: defined as the mean duration during which reflux is present 5 cm above the LOS.
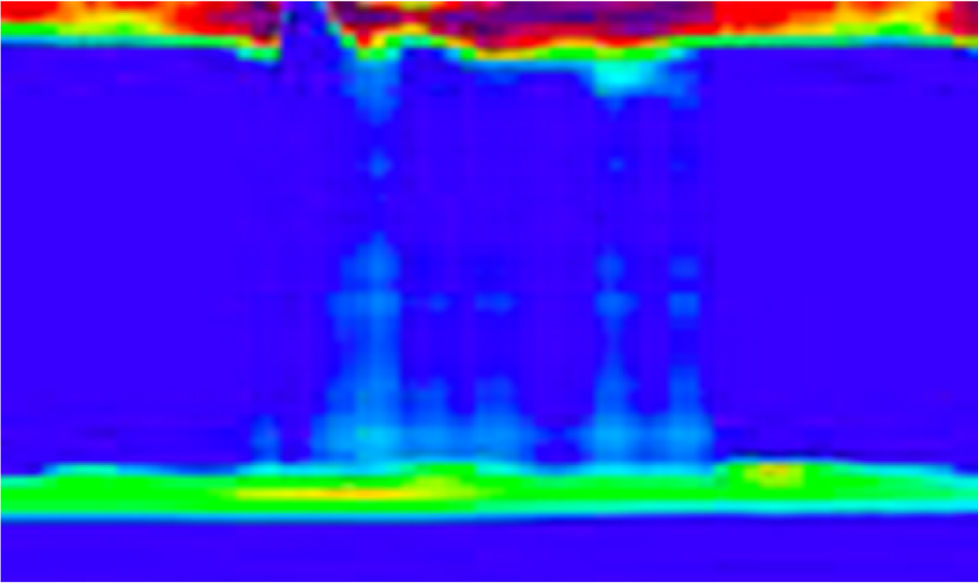
Reflux pH: all of the above parameters are classified as acid and non-acid based on the changes recorded at the time when the reflux occurred and are also determined by the patient's position, either standing or supine. An acid reflux episode is an event with pH falling below 4; a non-acid reflux is defined as the reflux episode in which the pH is above 4; a weakly acid episode defines the episode within a pH 4–7, and alkaline reflux when the pH is >7. Fig. 2 shows dual-channel pH monitoring, with short refluxes, and preserved oesophageal clearance.
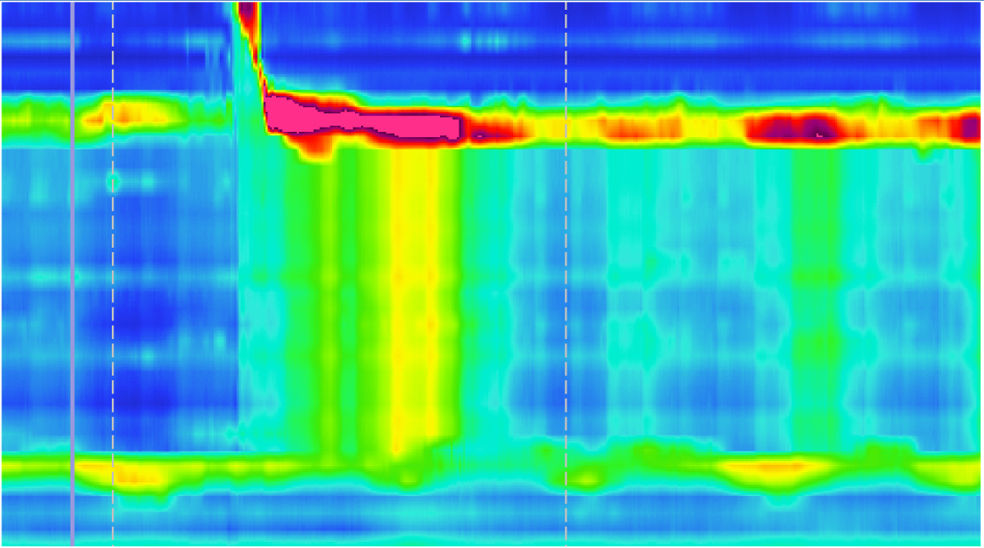
Fig. 3 shows the graph of a patient with reflux in both the supine and standing position.
Interpretation of resultsOnce these characteristics have been determined, we have to evaluate the following parameters in the pHz recording13,34:
- 1
Duration of pHz monitoring: the minimum duration to interpret a study and for it to be valid is 18 h.
- 2
Acid exposure time (AET) determination: this refers to the time the oesophagus is exposed to a pH < 4 and correlates with the presence of reflux. AET < 4%: physiological reflux; AET >4%–<6%: grey area; AET > 6%: pathological reflux.
- 3
Assessment of the number of reflux episodes: acid reflux is considered physiological when there are <40 acid reflux episodes; pathological reflux is when there are >80 episodes of acid reflux.
- 4
Establishment of the association of symptoms with reflux episodes: the symptomatic index is the ratio of the number of symptoms associated with reflux episodes to the total number of symptomatic episodes×100. The clinical symptom is present at least 3 times in 24 h monitoring, and is considered pathological when it happens 2 min. before or after the reflux episode; it is pathological if it is >50%, and the symptom association probability (SAP) is the probability that a patient's symptoms are related to reflux, it is significant if it is >95%.
- 5
DeMeester score assessment: this is the best-known measure for assessing pathological reflux; it is considered impaired when the total DeMeester score is >14.72; this measure considers the percentage of total time at pH < 4, the number of reflux episodes, and the position in which reflux episodes occur.
- 6
Nocturnal baseline impedance: this expresses mucosal integrity and provides evidence of macroscopic and microscopic oesophageal damage after exposure to reflux. It consists of measuring baseline impedance from 3 to 5 cm above the LOS during sleep in 3 periods of 10 min. Values <2292 Ω suggest the presence of GORD.
- 7
Post-reflux swallow-induced peristaltic wave: reflects the integrity of oesophageal peristalsis stimulated by reflux episodes and chemical clearance. It is abnormal when present with a 50% anterograde drop in impedance within 30 s after the reflux event.
- 8
Assessment of nocturnal acid leakage: physiologically, during sleep the frequency of reflux episodes decreases; however, there may be a nocturnal leakage phenomenon, with reflux episodes >1 h in duration during sleep.34
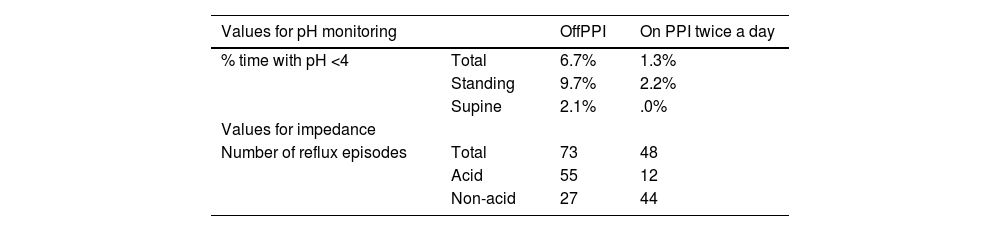
There are no established normality values for pHz assessment in patients with obesity. In 2016 Doulami et al.35 were the first group to assess normal values for 24 h pHz in volunteers with obesity without reflux and reported a higher number of reflux episodes and an equal or, in some cases, slightly increased median acid bolus clearance exposure, hypothesising that specific cohort values should be used in the assessment of pHz for patients with obesity36; however, to date we still use the same parameters as those established for healthy non-obese volunteers.37 The values are shown in Table 7.
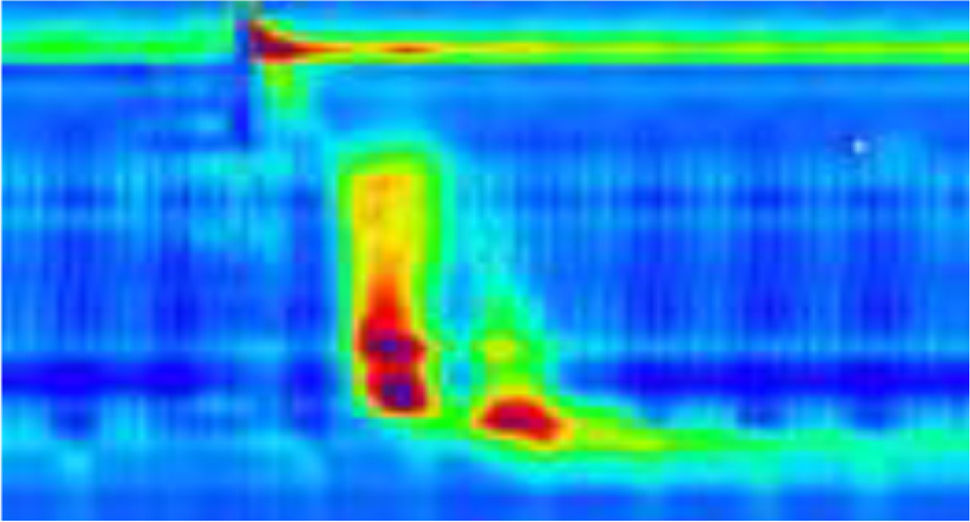
Fig. 4 shows a pH impedance monitoring plot.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Barba Orozco E, Ezquerra Duran A, Estudio del reflujo gastroesofágico. Interpretación de las pruebas funcionales en el paciente obeso. Cir Esp. 2023. https://doi.org/10.1016/j.ciresp.2023.01.001