Expansion of the pandemic produced by new coronavirus SATS-CoV-2 has made healthcare focused on patients with COVID-19 disease, leading to discontinue most of elective surgical procedures. Being thoracic surgery eminently oncological, an optimal triage of patients amenable to be safely operated on is mandatory. Moreover, severe pulmonary involvement by COVID-19 causes complications frequently needing urgent thoracic surgical procedures under a new context. The Spanish Society of Thoracic Surgery (SECT) has developed this document to establish basic recommendations to keep up essential elective surgical activity and to guide surgeons facing thoracic urgencies in this new and unknown environment.
La expansión de la pandemia producida por el nuevo coronavirus SARS-CoV-2 ha obligado a focalizar casi toda la asistencia sanitaria en pacientes con enfermedad COVID-19, obligando a suspender la mayoría de intervenciones quirúrgicas electivas programadas. La cirugía torácica es eminentemente oncológica, por lo que resulta obligada una adecuada priorización de los pacientes para ser intervenidos lo antes posible y en condiciones de máxima seguridad. Por otra parte, la afectación pulmonar grave COVID-19 presenta complicaciones que con frecuencia requieren procedimientos quirúrgicos torácicos urgentes en un contexto nuevo. La Sociedad Española de Cirugía Torácica (SECT) ha desarrollado este documento para establecer unas recomendaciones básicas para mantener la actividad quirúrgica electiva imprescindible y para orientar a los cirujanos que deban afrontar urgencias torácicas en este nuevo y desconocido entorno.
During the expansion of the SARS-CoV-2 coronavirus, the healthcare system has been overwhelmed, and much of the usual activity has been suspended, especially scheduled surgeries.1 The Spanish Society of Thoracic Surgery (SECT), through its Scientific Committee, has developed this document for the reorganization of surgical activity with the aim to: minimize the inherent risks of healthcare activities for patients and healthcare professionals; minimize collateral effects due to not being able to provide the healthcare required by patients with pathologies other than SARS-CoV-2 infection; optimize healthcare resources for the greatest possible efficiency; and investigate and offer solutions to the processes of the specialty that appear in a novel manner in these patients.
The evolution of the spread and impact of the SARS-CoV-2 coronavirus is dynamic. The disease scenarios are changing over very short periods of time and in different geographical areas. For this reason, management recommendations, which until now have been supported by a weak level of evidence, are subject to continuous modifications and should be flexible.
At the time of writing this document, the expansion of the SARS-CoV-2 coronavirus is generalized, so contact tracing is not possible. Therefore, it is a document of general ideas that we feel are applicable to similar potential threats that may occur. In the case of limited small outbreaks, many of the recommendations established in this document may not be necessary, even though specific measures may be needed to temporarily modify healthcare activity. This manuscript has therefore been developed for a time when all persons should be considered potential carriers and transmitters of the virus. It also focuses on circumstances in which there are no accurate tools that allow us to rule out asymptomatic virus carriers. Furthermore, not enough time has elapsed to be able to know how immunity develops in SARS-CoV-2 patients, whether it is complete, and what its duration will be.2
Healthcare centers are potential sources for spread of the SARS-CoV-2 coronavirus. Determining the infection situation or the immunological status of patients as well as healthcare workers in each medical activity is a priority to establish COVID-free healthcare circuits that provide optimized care for other pathologies.
MethodsTo prepare this document, a bibliographic search was conducted in PubMed (with the keywords COVID-19, SARS-CoV-2 and thoracic surgery). Likewise, we consulted the websites of the Spanish Ministry of Health, the Center for Disease Control (CDC), the World Health Organization (WHO), the American College of Surgeons (ACS) and those of various national and international scientific societies. This search was carried out by the scientific committee of the SECT and, after concurring during online meetings, the recommendations were extracted and included in this document. No formal consensus technique was used.
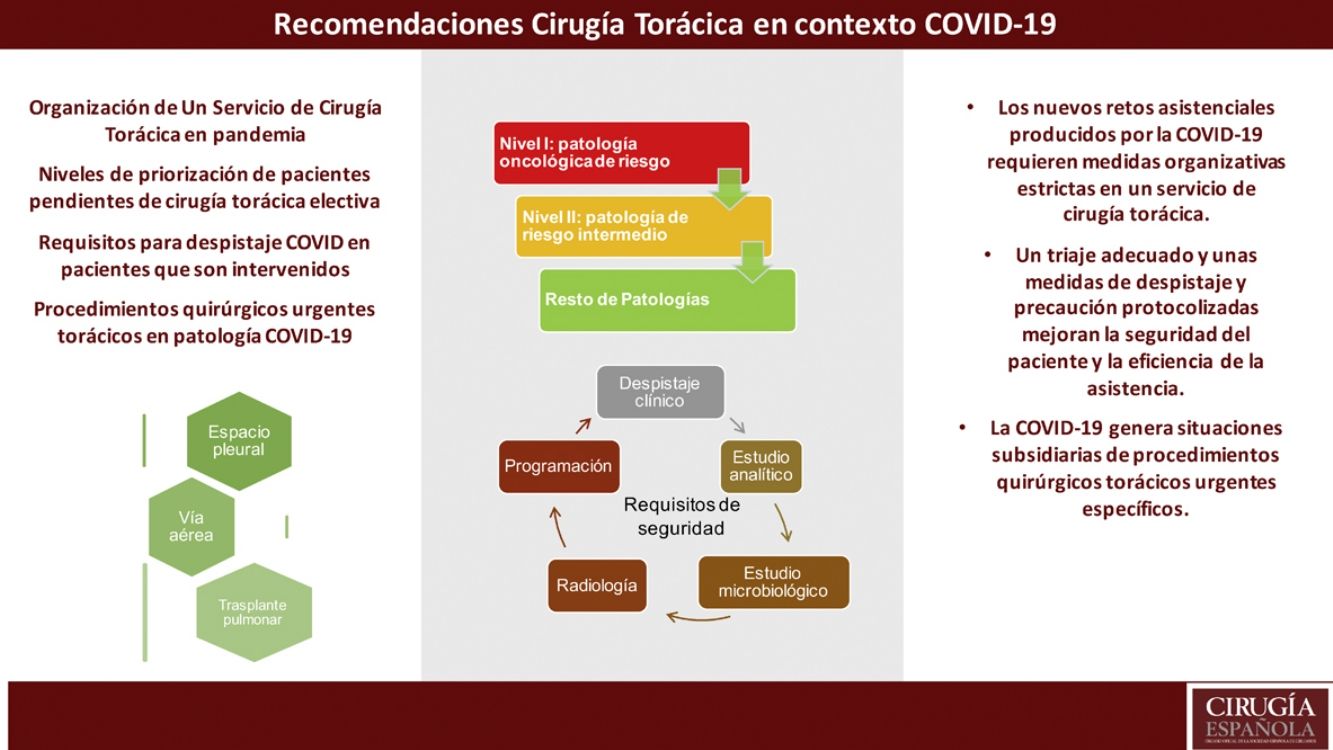
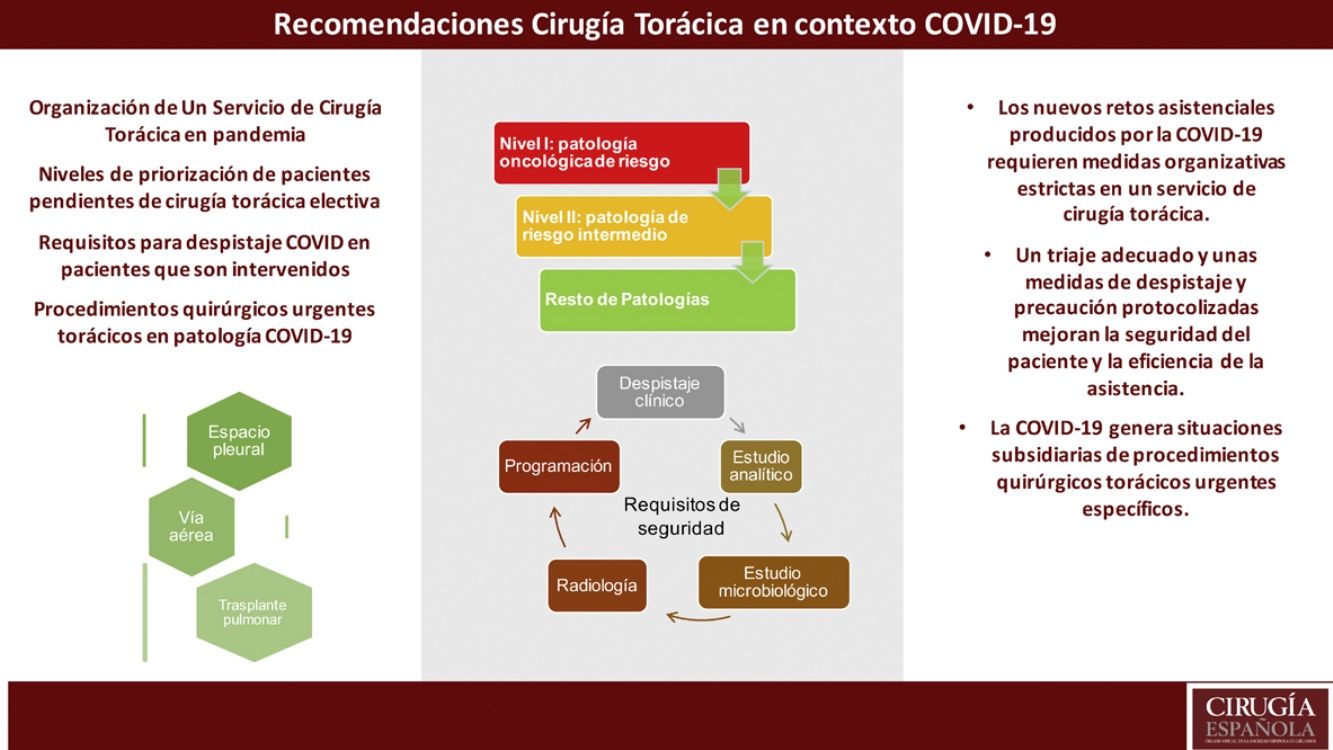
The final text was reviewed by each member of the SECT scientific committee, as well as by members of the Thoracic Surgery division of the Spanish Association of Surgeons (AEC) and its Scientific Committee. The first version of the document was published on the SECT and AEC websites on April 29, 2020. An attempt has been made to establish recommendations for scheduled and urgent surgery: internal organization of a Thoracic Surgery Service (TSS), measures for the different healthcare areas, organization of the scheduled surgical activity based on the epidemiological scenario, and the minimum requirements required to carry out scheduled procedures safely for both patients and surgeons. Within the urgent surgical activity, we analyzed the management of the pleural space (thoracic drainage) and the airway (tracheostomies), lastly making a brief reference to lung transplantation.
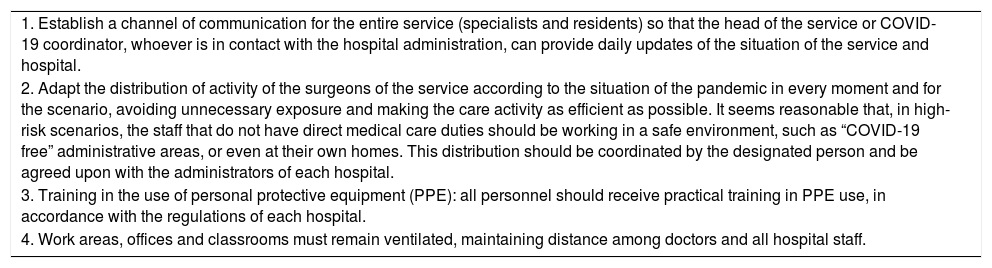
ResultsInternal organization of a TSSThe objective must be to optimize human and material resources in order to guarantee the continuity of medical care activities in the short, medium and long terms. In this context, the AEC establishes general recommendations that can be extrapolated to any surgical service (Table 1).3
Recommendations of the Spanish Association of Surgeons (AEC) for the organization of a surgical service.
| 1. Establish a channel of communication for the entire service (specialists and residents) so that the head of the service or COVID-19 coordinator, whoever is in contact with the hospital administration, can provide daily updates of the situation of the service and hospital. |
| 2. Adapt the distribution of activity of the surgeons of the service according to the situation of the pandemic in every moment and for the scenario, avoiding unnecessary exposure and making the care activity as efficient as possible. It seems reasonable that, in high-risk scenarios, the staff that do not have direct medical care duties should be working in a safe environment, such as “COVID-19 free” administrative areas, or even at their own homes. This distribution should be coordinated by the designated person and be agreed upon with the administrators of each hospital. |
| 3. Training in the use of personal protective equipment (PPE): all personnel should receive practical training in PPE use, in accordance with the regulations of each hospital. |
| 4. Work areas, offices and classrooms must remain ventilated, maintaining distance among doctors and all hospital staff. |
Each healthcare center establishes measures and recommendations aimed at reducing the risk of spreading the virus in the different areas of care. An activity protocol and basic hygiene measures are essential for this objective (supplementary material).
Surgical activity scheduled in an TSSIt is important to define possible scenarios for action in order to establish recommendations. Current evidence about the pathologies and collateral effects (both at the individual level and in terms of public health) derived from SARS-CoV-2 infection is very limited. It seems that performing surgery on patients who are in the incubation period of unknown COVID-19 disease carries a high risk of postoperative complications, with almost a 45% need for admission to the ICU and up to 20% mortality according to small preliminary studies.4 Even so, current recommendations are based on consensus opinions of professionals, published information and the collective experience, in this case, of thoracic surgeons.
In order to gather accumulated experience related to SARS-CoV-2 and thoracic surgery,5 the SECT has established real-time communication channels with partners through emails, social networks, and by designing surveys. Likewise, through the TSS of the AEC and other scientific societies, an attempt is made to obtain all the complementary information that allows conclusions to be drawn and transmitted to the scientific community.
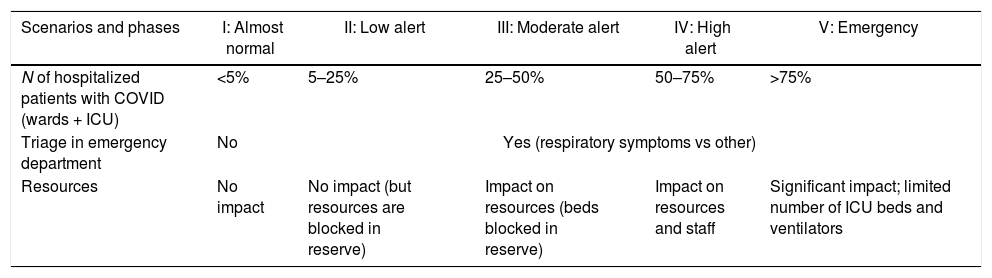
Scenarios for action based on the incidence and prevalence of SARS-CoV-2 pathology in hospitalsThe AEC has established a classification of five possible hospital scenarios of the SARS-CoV-2 pandemic (Table 2). A survey carried out by the SECT that is currently pending publication estimates that some 75% of hospitals with TSS in Spain reached peak scenarios IV and V during the first few weeks of the pandemic. Thoracic cancer surgery is, by definition, priority surgery, and we feel that certain non-urgent priority surgeries cannot be postponed despite a scenario that is considered ‘high alert’ or even ‘emergency’. Given the risk of outbreaks, action protocols must be updated in order to contemplate all possible scenarios.
Alert scenarios according to the expansion of the SARS-CoV-2 pandemic.
| Scenarios and phases | I: Almost normal | II: Low alert | III: Moderate alert | IV: High alert | V: Emergency |
|---|---|---|---|---|---|
| N of hospitalized patients with COVID (wards + ICU) | <5% | 5–25% | 25–50% | 50–75% | >75% |
| Triage in emergency department | No | Yes (respiratory symptoms vs other) | |||
| Resources | No impact | No impact (but resources are blocked in reserve) | Impact on resources (beds blocked in reserve) | Impact on resources and staff | Significant impact; limited number of ICU beds and ventilators |
The vast majority of patients undergoing thoracic cancer surgery do not require postoperative stays in the ICU, and the use of this type of human and material resources is relatively low. For this reason, in de-escalation phases, these patients should be considered a priority in the management of hospital surgical processes. We present a possible order of prioritization for thoracic cancer disease and the requirements that must be met before performing surgery.6
Prioritization of scheduled surgical procedures in patients with thoracic diseaseWe base our recommendations on those established by the American College of Surgeons (ACS),7 the American Association of Thoracic Surgery (AATS) and the Society of Thoracic Surgeons (STS),8 adapting them to current realities throughout the evolution of the pandemic in Spain.
- •
Level I. Patients who should be operated on preferentially.
- (1)
Bronchogenic carcinoma (BC), whether confirmed by histology or not, solid or predominantly solid (component greater than 50%) >2cm with no lymph node involvement (cN0).
- (2)
BC, whether confirmed by histology or not, with lymph node involvement and no indication for neoadjuvant therapy.
- (3)
Neuroendocrine tumors with mediastinal lymph node involvement with no indication for neoadjuvant therapy.
- (4)
Patients with BC who have completed neoadjuvant therapy: In these cases, assess the risk–benefit ratio of prolonging the neoadjuvant treatment in individual cases and in the context of a decision by a multidisciplinary committee.
- (5)
High-grade chest wall tumors: Assess the risk–benefit ratio of neoadjuvant treatment in individual cases and in the context of a decision by a multidisciplinary committee.
- (6)
Surgical procedures for diagnosis or staging in neoplasms or possible neoplasms that require starting preferential treatment.
- (7)
Mediastinal tumors that cause symptoms: Consider a histological study by transthoracic or endoscopic needle aspiration and neoadjuvant treatment in resectable tumors in the context of a decision made by a multidisciplinary committee.
- (8)
Selected cases of patients with resectable pleural mesothelioma after neoadjuvant treatment: It is recommended to individualize the cases and assess the potential benefit of surgical resection compared to a radical systemic treatment with chemoradiotherapy. Also, evaluate based on the type of surgery proposed, considering extrapleural pleuropneumonectomy high risk.
- (9)
Infectious complications of oncological processes, such as a lung abscess, in which medical treatment has failed or is not viable and which require surgical resection for resolution.
- (1)
- •
Level II. Patients in whom surgery may be delayed, although not more than three months after the indication for surgery.
- (10)
BC, whether confirmed by histology or not, predominantly ground glass or with a solid component less than 50%.
- (11)
BC, whether confirmed by histology or not, predominantly solid up to 2cm.
- (12)
Slow-growing, suspicious pulmonary nodule, documented by a retrospective series of radiological studies.
- (13)
Pulmonary neoplasms with histology other than BC, either identified or reasonably suspicious for pulmonary metastases in an oligometastatic context or carcinoid tumors without mediastinal lymph node involvement.
- (14)
Mildly aggressive thymic tumors confirmed by transthoracic needle aspiration with no associated symptoms: upon confirmation of thymic carcinoma or stage B3, induction treatment may be considered with later rescue surgery.
- (15)
Patients who, due to their clinical situation or characteristics of their pathology, present a high risk of postoperative complications: The risk–benefit ratio of the surgical procedure will be continually reassessed.
- (16)
Airway procedures, such as non-urgent tracheostomies, bronchoscopies, tracheal surgeries except malignant neoplasms with no alternative to surgery.
- (10)
- •
Level III. Patients in whom the surgery can be delayed with a low risk of complications derived from it: the remaining pathologies.
In the case of pure ground-glass lesions, the National Lung Screening Trial showed that the risk of malignancy after re-evaluation with CT scan after 6 months is only 1.1%. However, for lesions greater than 2cm, the risk of malignancy on re-evaluation CT scan after 3 months is 10.9%.9,10 In these cases, the interpretation of the evolution of ground-glass images may be hampered by the radiological lesions typical of SARS-CoV-2 pneumonia, with a more diffuse distribution but with a ground-glass appearance. Such images have been described in asymptomatic patients with no known history of COVID-19.11 It seems reasonable to wait in these cases at least 3 months for radiological reassessment in lesions with a diameter of less than 2cm.12
Therapeutic alternatives to consider based on availability and experience, after evaluation by a multidisciplinary committeeInternational guidelines have proposed that, in certain situations, alternative treatments can be contemplated after assessing the risk–benefit ratio:
- (1)
Evaluation of neoadjuvant therapy in tumors that are candidates for adjuvant treatment (such as neoplasms larger than 4cm, N1 lymph node involvement or chest wall involvement)
- (2)
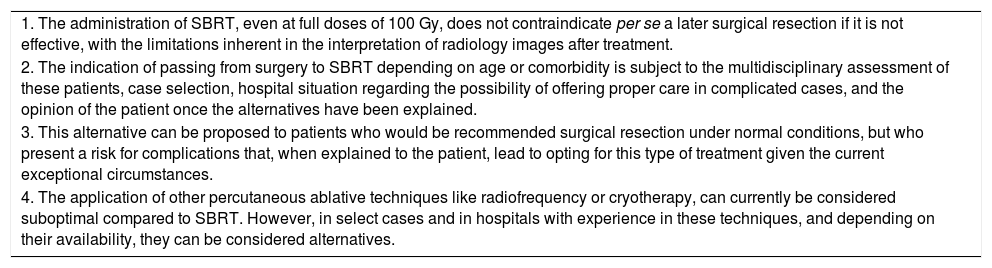
Consider performing extracranial stereotactic body radiation therapy (SBRT) in lesions within the indication, which can be considered in lung tumors in stage I of up to 3cm in size in patients with moderate surgical risk or over 80 years in whom resection had been proposed.13Table 3 presents some considerations in this regard.
Table 3.Considerations regarding the use of local therapies as an alternative to surgical resection in select cases of early-stage BC.
1. The administration of SBRT, even at full doses of 100 Gy, does not contraindicate per se a later surgical resection if it is not effective, with the limitations inherent in the interpretation of radiology images after treatment. 2. The indication of passing from surgery to SBRT depending on age or comorbidity is subject to the multidisciplinary assessment of these patients, case selection, hospital situation regarding the possibility of offering proper care in complicated cases, and the opinion of the patient once the alternatives have been explained. 3. This alternative can be proposed to patients who would be recommended surgical resection under normal conditions, but who present a risk for complications that, when explained to the patient, lead to opting for this type of treatment given the current exceptional circumstances. 4. The application of other percutaneous ablative techniques like radiofrequency or cryotherapy, can currently be considered suboptimal compared to SBRT. However, in select cases and in hospitals with experience in these techniques, and depending on their availability, they can be considered alternatives. BC: bronchogenic carcinoma; Gy: grays; SBRT: radioterapia estereotáxica extracraneal.
The application of these suggestions must be done cautiously and be endorsed by a multidisciplinary committee. We understand that they should be reserved for extreme situations and be preceded by thorough information for the patient, since they may represent a suboptimal cancer treatment. There is no evidence to recommend them from a scientific society.
Each case should be individualized by the entire TSS, reevaluating the surgical waiting list weekly in cases of level I and II pathologies, and every 15 days in level III pathologies. It is recommended to contact the patients on the waiting list by phone to update their clinical situation and their possible evolution with a frequency of one to 4 weeks, depending on the level of their pathology. It is recommended to repeat an imaging test in order to assess the changes in the lesions subject to surgery so that no more than 3 months elapse between the last study and surgery.
Requirements to be able to perform a scheduled surgical procedure, minimizing the added risk of complications in the context of a COVID-19 pandemic- 1.
A “COVID-19 free” circuit for preoperative care, transfers, operating room, postoperative stay unit and hospitalization area in the ward.
- 2.
Healthcare personnel who will treat the patient throughout the “COVID-19 free” process, according to the criteria and possibilities established by each hospital.
- 3.
Preoperative evaluation of the patient in the days prior to the intervention. At the moments of greatest extension of the pandemic, a clinical and epidemiological checklist was proposed, including complete physical examination and various tests, such as lab work, chest X-ray, PCR for the virus in nasopharyngeal exudate, and a complete serological study. Such a thorough study before a scheduled procedure, which would then have to be extrapolated to any interventional procedure at the hospital, is not feasible in practice. Furthermore, a fairly significant rate of serological false positives has been reported.14 Currently, a correct clinical and epidemiological check-list applied by telephone, together with the PCR screening study for SARS-CoV-2, is considered sufficient to carry out scheduled surgical procedures with a certain level of safety. This is especially the case when the sensitivity and specificity of serological studies are not well defined.15,16 We include an example of a checklist for clinical and epidemiological screening (supplementary material). In cases of positive PCR or clinical and/or epidemiological suspicion, surgery should be postponed for 14 days, and the patient should then be fully reassessed, following the same steps. To proceed with surgery, a negative PCR test and a normal clinical–epidemiological study from the preceding 2 weeks must be available.
- 4.
The patient must sign a specific informed consent form with the information and the specific risks of surgical intervention in the context of the COVID pandemic.
Depending on the healthcare setting and the medical center, surgeons who treat urgent thoracic surgical patients are usually not thoracic surgeons.
Recommendations for the placement and management of chest drains in the context of the COVID-19 pandemic- 1.
In pleural effusions, with the exception of empyema and hemothorax, the placement of closed pleural catheter systems connected to a bag is recommended instead of connection to an underwater-sealed system. In the event of an air leak that fills the collection bag with air, it will be replaced by a conventional water-seal system.
- 2.
In pneumothorax with indication for thoracic drainage, connection to a conventional water-seal system is recommended. Some authors propose adding bleach to the water seal at a 1:50 dilution ratio. Likewise, filters with the capacity to filter viruses can be used at the outlet of the water-seal system, towards the intake or outside the system.17 There are no studies that show whether the connection of the system to suction can reduce the presence of viruses in the environment by aerosolization.
- 3.
There is no evidence of the greater benefit of the use of digital systems in these patients.18
- 4.
Elimination of air by the water-seal system in air leaks constitutes a source of aerosolization with a high risk of transmission of SARS-CoV-2.
- 5.
In general, and especially in patients subjected to positive airway pressure, it is recommended to avoid early removal of chest drains placed for pneumothorax in patients with COVID-19 pneumonia. It is recommended to clamp or close the drain for at least 24h before confirming the absence of pneumothorax radiologically.19
- 6.
In the case of secondary spontaneous pneumothorax in a patient with COVID-19 lung involvement or iatrogenic barotrauma pneumothorax, aspiration must be handled with caution to achieve maximum lung re-expansion by collecting all air leakage. This can be begun by keeping the drain in free fall and, if necessary, connecting intermittently or with suction pressures below 15cmH2O.
- 7.
The technique of placing a chest drain does not differ from the standard technique. In mechanical ventilation, it is recommended to temporarily interrupt ventilation when inserting the drain until it is quickly connected to the water-seal system, in order to minimize the leakage of contaminated air to the outside. If immediate connection to the water-seal system is not possible, the drain may be momentarily clamped.17
This is frequently indicated to favor weaning in patients with prolonged intubation due to severe SARS-CoV-2 pulmonary involvement. There is little evidence as to whether a percutaneous or open tracheostomy is safer in these patients. In any case, a quick procedure by trained personnel is recommended.20 Although there is no evidence to recommend surgical over percutaneous tracheostomy, the latter may imply a longer time to open the airway and in a less controlled manner. General recommendations in this regard have already been published.21
Emergency thoracic surgery proceduresIn situations in which the patient presents a vital risk in a very short space of time, the general approach is the same as usual, using the greatest possible safety measures for the patient and for healthcare workers.
Situations that require early, non-urgent surgical treatmentThis would be the case of pneumothorax with persistent air leak without respiratory complications, or the presence of empyema that can be managed conservatively. The evolution of these patients should be monitored by a TSS. If conservative management is feasible under safe conditions, opt for it.
Recommendations regarding lung transplantationDonation and transplantation activity has been reduced from a daily average of 7 donors and 15 transplantations performed to 1.1 notified donors and 2 transplantations performed per day in Spain. The National Transplant Organization (NTO) has issued successive reports establishing recommendations at each moment of the pandemic depending on the varying epidemiological situation22:
- 1.
Adapt the transplant activity of each hospital to its reality at all times.
- 2.
Restrict the activity to patients in emergency situations or with greater difficulties to be transplanted. When the general situation allows, gradually incorporate patients with a low probability of post-transplantation complications and with expectations of a short hospital stay.
- 3.
Prioritize donation to suitable donors in brain death and controlled asystole, at the most critical moments, to later consider donors with expanded criteria, reactivating donation-oriented intensive care programs. Uncontrolled asystole programs have been the last to be reactivated.
- 4.
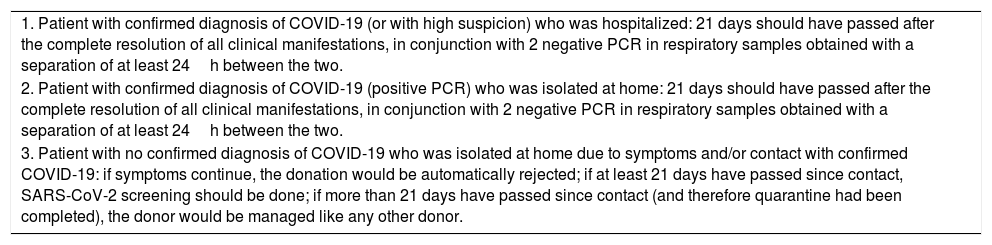
All potential lung donors are screened. In these cases, PCR for SARS-CoV-2 will be performed on a bronchoalveolar lavage sample at least 24h prior to donation. Table 4 indicates the criteria that the NTO considers a cured case in a potential donor. Patients on the waiting list with COVID-19 disease should be excluded from it until these criteria for cure are met.23
Table 4.Criteria for a cure in potential organ donors with COVID-19 disease.
1. Patient with confirmed diagnosis of COVID-19 (or with high suspicion) who was hospitalized: 21 days should have passed after the complete resolution of all clinical manifestations, in conjunction with 2 negative PCR in respiratory samples obtained with a separation of at least 24h between the two. 2. Patient with confirmed diagnosis of COVID-19 (positive PCR) who was isolated at home: 21 days should have passed after the complete resolution of all clinical manifestations, in conjunction with 2 negative PCR in respiratory samples obtained with a separation of at least 24h between the two. 3. Patient with no confirmed diagnosis of COVID-19 who was isolated at home due to symptoms and/or contact with confirmed COVID-19: if symptoms continue, the donation would be automatically rejected; if at least 21 days have passed since contact, SARS-CoV-2 screening should be done; if more than 21 days have passed since contact (and therefore quarantine had been completed), the donor would be managed like any other donor.
The personal protective equipment for surgical staff should be that of a moderate–high risk procedure.24
Protection protocol for medical professionals in the operating roomThe AEC has developed a protocol that can be extrapolated to all surgical activities.3 Surgery that involves opening the airway or lung parenchyma is considered to have a special risk for viral transmission.25,26 Minimally invasive surgery could carry a lower risk of intraoperative transmission of the virus. Currently, there is no evidence about the role of intraoperative CO2 and the transmission of the virus.27
Updates to this documentThe SECT scientific committee will publish updates for this document on the websites of both the SECT and AEC.
ConclusionsThe limited evidence for analyzing the available data on the topics discussed and the rapid evolution of an epidemiological situation of this type make it difficult to establish solid recommendations from a scientific society. However, we have created this document by pooling available data, which has then been interpreted by thoracic surgery professionals in a scientific committee. The recommendations can be adapted to the particular clinical–epidemiological situation of each service and medical professional, depending on the geographical and temporal reality of the SARS-CoV-2 pandemic. It also serves as an axis from which the hypotheses presented herein can be validated prospectively.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Jarabo JR, Martínez N, Cabañero A, Call S, Campo-Cañaveral JL, Cilleruelo Á, et al. Recomendaciones de actuación en cirugía torácica electiva y urgente en contexto de pandemia por SARS-CoV-2 de la Sociedad Española de Cirugía Torácica (SECT). Cir Esp. 2020;98:574–581.