Primary hyperparathyroidism is the third most common endocrine disease. The aim of our study was to determine long-term outcomes and risk factors for persistence in patients undergoing parathyroidectomy for primary hyperparathyroidism.
MethodsRetrospective study including patients undergoing parathyroidectomy between 2009−2019. Cure was defined as reestablishment of normal calcium homeostasis lasting a minimum of 6 months. Persistence was defined by ongoing hypercalcemia more than 6 months after surgery. Recurrent PHTP was defined by recurrence of hypercalcemia after a normocalcemic interval at more than 6 months after surgery. A more detailed analysis was performed on patients with normocalcemia and persistently elevated PTH levels after surgery. Variables independently related to persistence were analyzed by multivariate analysis.
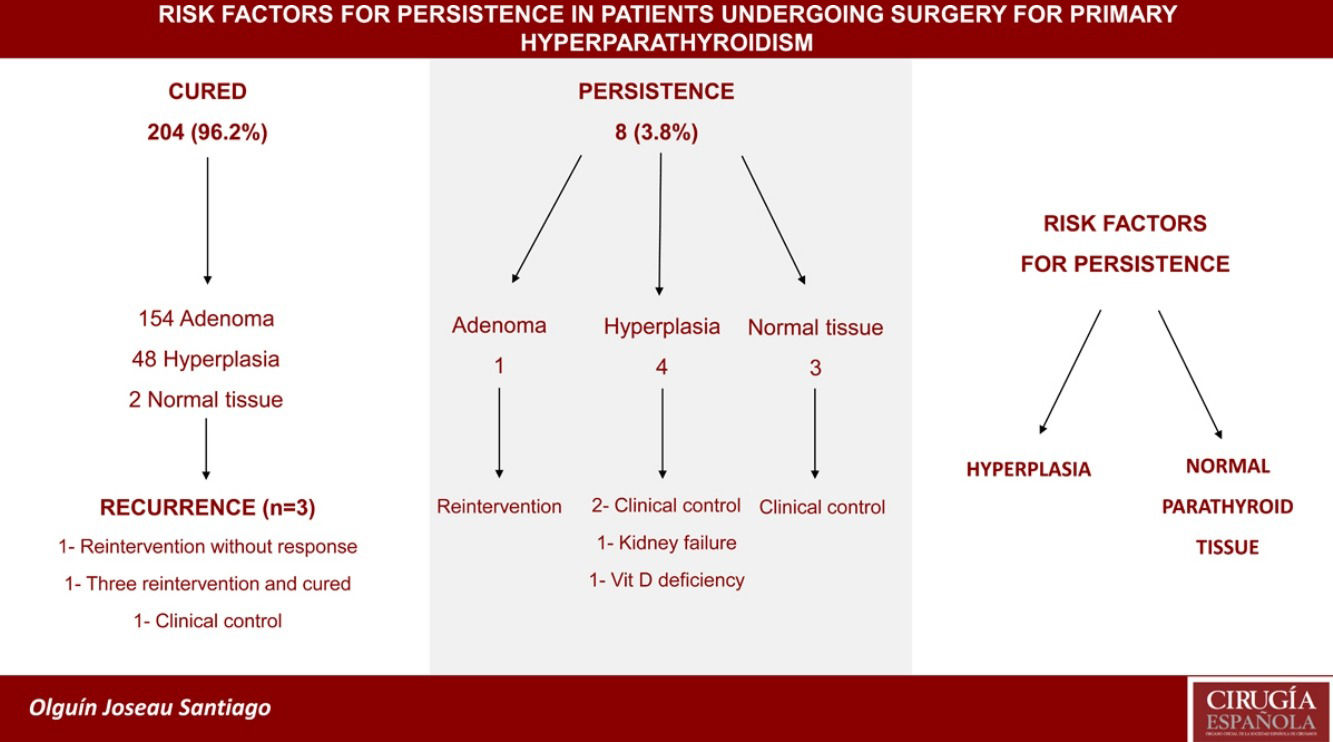
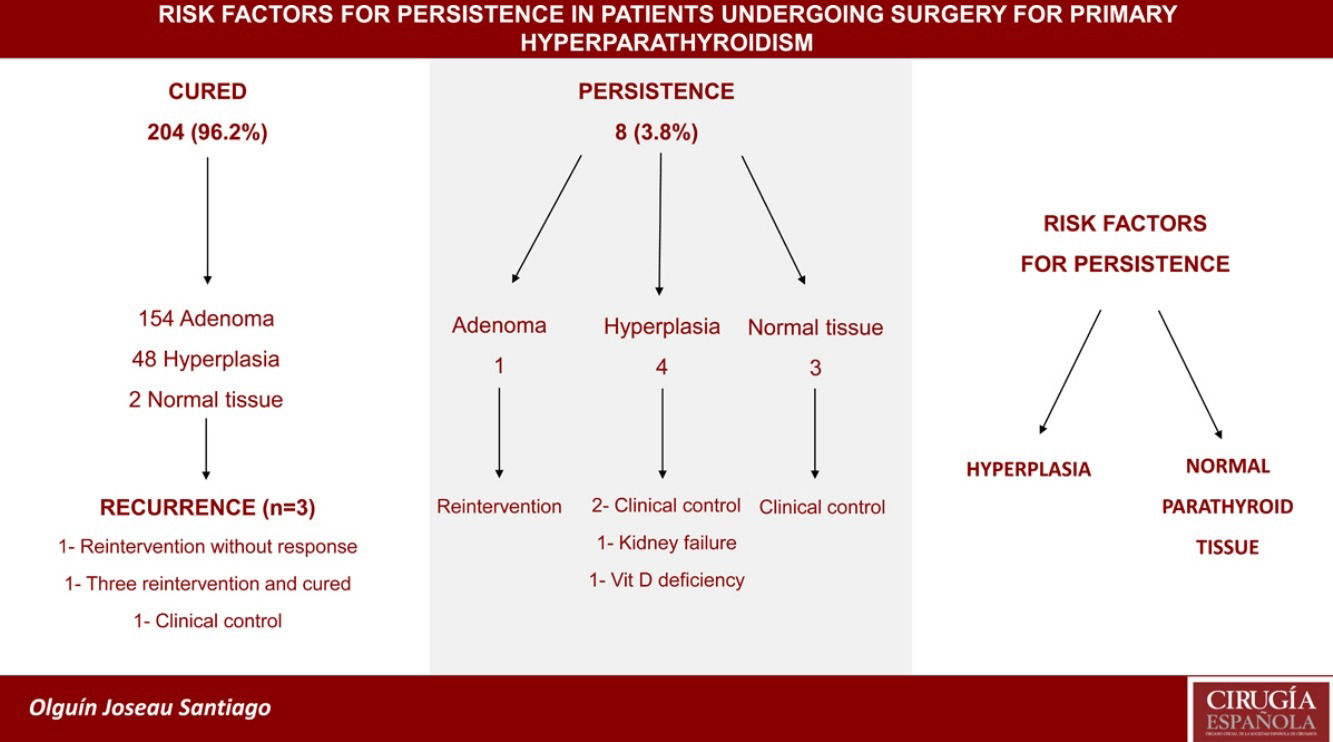
ResultsWe included 212 patients. Mean age was 59 years and 83% were women. Cure was observed in 204 patients (96.2%), persistence in 8 (3.8%) and recurrence in 3 (1.4%). Four patients (1.9%) presented normocalcemia and persistently elevated PTH after surgery. All presented parathyroid pathology (2 adenomas and 2 hyperplasia). In follow-up we observed that adenoma subgroup presented one patient with CKD and one with vitamin D deficiency while in the hyperplasia subgroup two patients presented CKD. Persistence was independently associated with hyperplasia (Odds ratio = 12.6, IC95% = 1.28−124, p = 0.030) and normal parathyroid tissue (Odds ratio = 188, IC95% = 9.33−379, p = 0.001) on histopathological report.
ConclusionPrimary hyperparathyroidism is a safe procedure in terms of morbidity and long-term outcomes. Hyperplasia and normal parathyroid tissue on histopathological report are risk factors for persistence. An interdisciplinary diagnostic and therapeutic approach is required to prevent persistence.
El hiperparatiroidismo primario es la tercera enfermedad endócrina más frecuente. El objetivo de este estudio fue determinar los resultados a largo plazo y los factores de riesgo de persistencia en pacientes operados por hiperparatiroidismo primario.
MétodosEstudio retrospectivo de pacientes operados de paratiroidectomía entre 2009−2019. Se definió cura como el restablecimiento de la homeostasis normal del calcio durante un mínimo de seis meses, persistencia como la continuidad de hipercalcemia por más de seis meses postoperatorios, y recurrencia como la reaparición de hipercalcemia luego de un intervalo normocalcémico mayor a seis meses postoperatorios. Se realizó un análisis más detallado en pacientes con normocalcemia y hormona paratiroidea (HPT) elevada postoperatoria. Las variables independientemente relacionadas a persistencia fueron analizadas mediante análisis multivariante.
ResultadosSe incluyeron 212 pacientes. La edad media fue 59 años y 83% fueron mujeres. Se observó cura en 204 pacientes (96,2%), persistencia en ocho (3,8%) y recurrencia en tres (1,4%). Cuatro pacientes (1,9%) presentaron normocalcemia y HPT persistentemente elevada luego de la cirugía. Todos presentaron patología paratiroidea (dos adenoma y dos hiperplasia). En el seguimiento se observaron tres pacientes con fallo renal crónico (FRC) y uno con déficit de vitamina D. La persistencia se asoció independientemente con hiperplasia (Odds ratio = 12,6; IC 95%: 1,28–124; p = 0,030) y tejido paratiroideo normal (Odds ratio = 188; IC 95%: 9,33–379; p = 0,001) en el estudio histopatológico.
ConclusiónLa paratiroidectomía es un procedimiento seguro en términos de morbilidad y resultados a largo plazo. La hiperplasia y el tejido paratiroideo normal en el estudio histopatológico son factores de riesgo de persistencia.
Primary hyperparathyroidism (PHPT) is characterized by the persistent elevation of total serum calcium levels with corresponding elevated or inappropriately normal parathyroid hormone (PTH) levels. The only definitive treatment for PHPT is surgical resection of adenomatous or hyperplastic parathyroid glands1–3.
Surgical cure is defined as the reestablishment of normal calcium homeostasis lasting a minimum of 6 months. Persistent disease is defined by ongoing hypercalcemia more than 6 months or later after surgery. Recurrent PHTP is defined by recurrence of hypercalcemia after a normocalcemic interval at more than 6 months after surgery4.
We present a retrospective cohort of 212 patients who underwent parathyroidectomy for PHPT between 2009−2019. Mean age was 59 years and 176 (83%) were women. Cervical ultrasonography and sestamibi scintigraphy were performed in 155 patients (73.1%), ultrasonography alone in 29 (13.7%) and sestamibi scintigraphy in 28 (13.2%). Both studies coincided in 86 patients (55.4%).
Considering that 47 patients (22.2%) required total thyroidectomy and excluding them, we carried out a focused dissection in 127 (59.9%) and a bilateral exploration in 38 (17.9%). Multiglandular disease was observed in 13 patients (6.1%) and all were cured (Table 1).
Surgical variables.
| Cure | Persistence | p | |
|---|---|---|---|
| Focused dissection | 124 (97.6%) | 3 (2.4%) | 0.272 |
| Bilateral exploration | 36 (94.7%) | 2 (5.3%) | 0.636 |
| Surgery location | 0.642 | ||
| Upper right | 21 (100%) | 0 | |
| Upper left | 29 (93.5%) | 2 (6.5%) | |
| Lower right | 84 (95.5%) | 4 (4.5%) | |
| Lower left | 68 (97.1%) | 2 (2.9%) | |
| Ectopic | 1 (100%) | 0 | |
| Biopsy | 0.001 | ||
| Adenoma | 154 (99.4%) | 1 (0.6%) | |
| Hyperplasia | 48 (92.3%) | 4 (7.7%) | |
| Normal tissue | 2 (40%) | 3 (60%) |
Median surgical time was 60 min. Median hospital length of stay was 1 day. Seven patients (3.8%) presented complications. We observed 2 transitory and 1 permanent recurrent nerve palsy, 3 symptomatic hypocalcemia with need of readmission and 1 reintervention for surgical site hematoma.
Mean follow-up time was 29 months (SD = 21.6). Cure was achieved in 204 patients (96.2%). Persistence was observed in 8 patients (3.8%) and recurrence in 3 (1.4%).
Four patients (1.9%) presented normocalcemia and persistently elevated PTH levels after surgery. All presented parathyroid pathology (2 adenomas and 2 hyperplasia). In postoperative follow-up we observed that adenoma subgroup presented one patient with chronic kidney disease (CKD) and one with vitamin D deficiency while in the hyperplasia subgroup two patients presented CKD.
Multivariate analysis showed that persistence was independently associated with hyperplasia (Odds ratio = 12.6, IC95% = 1.28−124, p = 0.030) and normal parathyroid tissue (Odds ratio = 188, IC95% = 9.33−379, p = 0.001) on histopathological report (Table 2).
Multivariate analysis.
| OR | IC 95% | p | |
|---|---|---|---|
| Hyperplasia | 12.6 | 1.28–124 | 0.030 |
| Normal parathyroid tissue | 188 | 9.33–379 | 0.001 |
| Previous surgery | 1.17 | 0.09–14.3 | 0.898 |
| Bilateral exploration | 1.80 | 0.20–15.8 | 0.594 |
| PTH >200 | 0.69 | 0.12–4.1 | 0.683 |
| Age over 60 years | 0.16 | 0.01–1.86 | 0.144 |
| Hypertension | 0.16 | 0.01–1.60 | 0.121 |
PTH (parathyroid hormone).
Parathyroidectomy is the only definitive cure for PHTP. Our cure rate of 96.2% was in accordance with the American Association of Endocrine Surgeons guidelines which states that it should approach 95%–99%4.
In patients with persistence, histopathological report informed one adenoma, four hyperplasia and three normal parathyroid tissue. The patient with adenoma underwent reintervention with the subsequent cure while the other seven patients clinical control was performed. The group of hyperplasia presented one patient with CKD, one with vitamin D deficiency. On the other two hyperplasia patients and on the normal parathyroid group no pathology was identified.
Although patients with normocalcemia and increased PTH are considered cured, causes of secondary hyperparathyroidism disease should be evaluated and a long-term surveillance for recurrence should be performed. We evaluated this group of patients and found that all presented parathyroid pathology in histopathological report and other causes of elevated PTH were identified (CKD and vitamin D deficiency). There are several authors who report causes of normocalcemia and elevated PTH (CKD, vitamin D deficiency, advanced age, high preoperative PTH, inadequate calcium absorption and decrease in PTH sensitivity due to PHPT)4–7. Despite this, it is expected that this group of patients will achieve a long-term eucalcemia8.
Our recurrence rate of 1.4% was similar to rates reported by other studies in surgically treated PHPT8,9. In this concept they agree that patients who raise any of both biochemical parameters after a normocalcemic interval of 6 months should be considered as recurrence. In the three patients with recurrence in our series the histopathological report informed adenoma. Imaging studies were performed and in all the site of recurrence coincided with previous location. In the first patient clinical control was carried out. In the second patient, one reintervention was performed and histopathological report informed parathyroid adenoma. After surgery continued with persistence and was lost in follow-up. In the third patient three reinterventions were performed for three recurrences and in the three opportunities presented histopathological confirmation of adenoma and until the last control presented as cured.
Hyperplasia and normal parathyroid tissue on histopathological report were risk factors for persistence in our series. Hyperplasia has been previously described as a risk factor for surgical failure and the authors concluded that performing a focused dissection may lead to an increased risk of persistence due to not observed parathyroid disease10. Nevertheless, histopathological report is only available only after surgery so we have to underline the importance of a meticulous preoperative localization study of the affected parathyroid gland. Moreover, the high persistence rate in patients with normal parathyroid tissue on histological report reinforce this concept since the cause of the PHPT remains without treatment in this group.
Biochemical criteria used for diagnosis should be the same used to define persistence or recurrence. Other causes of normocalcemia and elevated PTH should be evaluated after six months of surgery. Long-term surveillance for recurrence should be performed. It is important to take these concepts into account because if the cause of persistence or recurrence is identified it can be treated and the patient can be given a better prognosis.
FundingThere was no source of funding.
Conflict of interestThe authors declare that they have no conflict of interests.
Please cite this article as: Olguín Joseau S, Arias A, Garzón A, Peretti E, Guzmán L, Ruggieri M. Factores de riesgo de persistencia en pacientes con tratamiento quirúrgico de hiperparatiroidismo primario. Cir Esp. 2022;100:569–572.