We aim to determine the utility of intraoperative parathyroid hormone (IOPTH) monitoring in patients with matching preoperative ultrasound and mibi SPECT for primary hyperparathyroidism for a single adenoma.
MethodsAll patients who underwent minimally invasive parathyroidectomy (MIP) for pseudohypoparathyroidism (PHP) for a single parathyroid adenoma, were included. An Ultrasound and mibi SPECT were performed in all patients. We defined matching studies when both coincided in the localization of the adenoma. IOPTH was performed in all patients and analyzed in three occasions: a baseline measurement at the anesthetic induction, immediately before, and 15 min after gland excision. Success was defined during the third measurement as a drop of IOPTH of at least 50% compared to the previous maximum value after gland excision. Demographics, intraoperative, postoperative variables and the utility of IOPTH monitoring were analyzed.
ResultsA total of 218 MIP were performed. The average age was 60.1 years and 85% were female. Preoperative ultrasound and mibi SPECT coincided 100%. When the adenoma was localized, 15 min after its excision, IOPTH did not decrease in 9 patients (4.2%. OR 1.9%–7.69%); all of them underwent a bilateral neck exploration. The added-value of IOPTH accuracy for disease cure was 3.6%. There was a 99% of cure rate. The mean surgical time was 66.4 min and the waiting time for the third IOPTH result was 31 min. Performing IOPTH monitoring made the surgery about twice more expensive.
ConclusionsPreoperative matching ultrasound and mibi SPECT for parathyroid adenoma localization in PHP, could avoid IOPTH monitoring in minimally invasive parathyroidectomies.
La causa más frecuente de hiperparatiroidimso primario (HPP) es el adenoma paratiroideo (único en el 80–85% de los casos y doble en un 4%, aproximadamente). El resto de los casos obedece a una hiperplasia de las glándulas paratiroides, o de forma más infrecuente, a un carcinoma paratiroideo. Nuestro objetivo es determinar la utilidad de la PTH intraoperatoria (PTHio) en pacientes con ecografía cervical y centellograma coincidentes preoperatorios, en el HPP por un adenoma simple.
MétodosSe realizó un estudio retrospectivo, unicéntrico, incluyendo todos los pacientes sometidos a paratiroidectomía mini-invasiva (PMI) por HPP, por adenoma simple fueron incluidos. Definimos estudios coincidentes cuando ambos localizaron el adenoma. La PTHio fue medida en tres ocasiones: en la inducción anestésica, inmediatamente antes y a los 15 minutos de la escisión de la glándula. El éxito se definió como la caída de al menos el 50% del valor máximo de la PTH luego de remover de la glándula. Se analizaron variables demográficas, intraoperatorias, postoperatorias y la utilidad de la PTHio.
ResultadosSe realizaron un total de 499 paratiroidectomías, de éstas, 218 presentaron un adenoma localizado en la ecografía y gammagrafía. La edad fue de 60.1 años y 85% eran mujeres. Luego de 15 minutos de la escisión del adenoma, la PTHio no descendió en 9 pacientes (4.2%. OR 1.9%–7.69%); todos ellos fueron a una exploración cervical bilateral. El valor agregado de la PTHio para la cura de la enfermedad fue de 3.6%. Hubo un 99% de curación de enfermedad. El tiempo operatorio fue de 66.4 minutos, y el de espera de la PTHio de 31 minutos. La PTHio encareció el procedimiento al doble.
ConclusiónesLa ecografía y el centellograma preoperatorios coincidentes para la localización de un adenoma en HPP, podrían evitar la medición de la PTHio durante las PMI.
Historically, bilateral cervical exploration has been the approach of choice in primary hyperparathyroidism (PHP) surgery1. Because between 80% and 90% of patients with PHP have single-gland disease, focused minimally invasive parathyroidectomy (MIP) with intraoperative parathyroid hormone (IOPTH) monitoring has been widely accepted2,3. This approach has been made possible by improvements in the accuracy of imaging studies to detect the pathological gland.
Many authors have shown that the combination of ultrasound and scintigraphy with technetium-99 sestamibi SPECT for the preoperative localization of a parathyroid adenoma has a diagnostic accuracy higher than 90%4. Precise localization would make it possible to avoid monitoring with IOPTH during parathyroidectomy, with results comparable to those reported in patients with IOPTH1 (Fig. 1).
The objective of this study was to determine the usefulness of IOPTH monitoring in patients with coinciding preoperative ultrasound and scintigraphy with technetium-99 sestamibi SPECT in patients with primary hyperparathyroidism caused by a single parathyroid adenoma.
MethodsAfter the approval of the Review Committee of our institution (Hospital Alemán, Buenos Aires, Argentina), a retrospective, single-center study was carried out that included all patients who underwent MIP for PHP caused by a single parathyroid adenoma from January 2008 to December 2018. We included all patients with a diagnosis of PHP and suspected parathyroid adenoma who had two coinciding preoperative imaging studies (ultrasound and scintigraphy) in which MIP was performed with IOPTH monitoring. All patients with less than six months of postoperative follow-up were excluded to rule out persistent hyperparathyroidism. Patients with secondary hyperparathyroidism or any hyperparathyroid syndrome were also excluded.
The diagnosis of PHP was made by the Endocrinology Department in all cases and was based on two factors: clinical presentation and/or laboratory parameters (normocalcemic PHP, with persistently elevated parathyroid hormone [>55 pg/mL]) and/or symptoms of hyperparathyroidism (pathological fractures, renal colic, polyuria, pain and generalized muscle weakness); or hypercalcemic PHP (serum calcium >10.5 mg/dL) with or without symptoms. All patients underwent ultrasound and technetium-99 sestamibi scintigraphy with SPECT to locate the pathological glands. Coinciding preoperative imaging studies were defined as concurring ultrasound and MIBI-SPECT results regarding the location of the pathological gland. The indication for parathyroidectomy was based on the guidelines for the definitive treatment of primary hyperparathyroidism of the American Association of Endocrine Surgery5. All surgical procedures were performed by two specialists in head and neck surgery or by general surgery residents under supervision. The surgical technique used in all patients was minimally invasive and focused, following the location identified in the preoperative imaging studies6. Bilateral cervical exploration was carried out in patients with persistently elevated IOPTH after excision of what was assumed to be the pathological gland. Patients were considered to have multiglandular disease when more than one pathological gland was found during surgery (abnormal size and/or persistently elevated IOPTH), as confirmed by histology (frozen biopsy).
IOPTH was analyzed on three occasions: a baseline measurement at induction of anesthesia, immediately before excision of the pathological gland, and 15 min afterwards. Success was defined as a decrease in IOPTH ≥50% during the third measurement compared to the maximum previous value after removal of the pathological gland7. PTH concentrations were measured with Roche Cobas E 601 electrochemiluminescence immunoassay (Roche Diagnostics, Mannheim, Germany). The lack of decline in IOPTH was analyzed in cases of persistently high levels in the third measurement after excision of the presumed pathological gland, calculating the prevalence of the event with a 95% confidence interval, considering the distribution binomial. We also analyzed the added value of the precision of IOPTH for curing hyperparathyroidism. The patients were treated under a short-hospitalization surgical regimen.
Patients were discharged from hospital when they could tolerate oral intake and had a stable clinical condition. Follow-up visits were scheduled for 7 days, 30 days and 6 months after hospital discharge.
The disease was considered cured when patients presented no symptoms of hyperparathyroidism, in addition to normal calcium and parathyroid hormone levels (serum calcium: 8.5–10.5 mg/dL; PTH: 10–55 pg/mL) at the six-month follow-up. After that period, they continued to be followed by the Endocrinology Department.
Variables analyzedData analyzed included age, sex, American Society of Anesthesiologists (ASA) classification, diagnosis from imaging studies, and comorbidities and clinical findings associated with primary hyperparathyroidism. We analyzed the diagnostic utility of ultrasound and scintigraphy together. Perioperative variables were registered, such as operative time, costs, usefulness of IOPTH measurement, and conversion of surgery to bilateral cervical exploration. We also analyzed the different variables and their relationship with the persistence of disease after surgical treatment (age >60 years, calciuria >400 mg/dL/day, calcium >11.5 mg/dL, PTH >100 pg/mL, weight of diseased gland >1 g, lack of decrease in IOPTH, gland size >1.5 cm). Morbidity and mortality rates were also considered in the hospital stay analysis.
Statistical analysisFor the statistical analysis, the IBM SPSS (version 20.0) program was used. A P value <.05 was considered statistically significant.
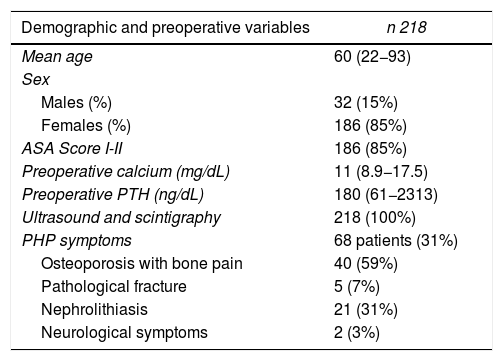
ResultsDuring the study period, a total of 499 parathyroidectomies were performed for primary hyperparathyroidism. There were 218 patients who met the inclusion criteria, with a mean age of 60.1 years (22–93 years) and a predominance of females (85%). Mean preoperative serum calcium was 11 mg/dL (8.9–17.5 mg/dL) and PTH was 180 pg/mL (61–2313 pg/mL). The vast majority of patients were in good clinical condition at the time of surgery. Out of the 218 patients, 68 (31%) presented symptoms associated with primary hyperparathyroidism (40 presented osteoporosis with associated bone pain, five had pathological fractures, 21 nephrolithiasis, and two patients with neurological symptoms) (Table 1).
Demographic and preoperative variables.
| Demographic and preoperative variables | n 218 |
|---|---|
| Mean age | 60 (22−93) |
| Sex | |
| Males (%) | 32 (15%) |
| Females (%) | 186 (85%) |
| ASA Score I-II | 186 (85%) |
| Preoperative calcium (mg/dL) | 11 (8.9−17.5) |
| Preoperative PTH (ng/dL) | 180 (61−2313) |
| Ultrasound and scintigraphy | 218 (100%) |
| PHP symptoms | 68 patients (31%) |
| Osteoporosis with bone pain | 40 (59%) |
| Pathological fracture | 5 (7%) |
| Nephrolithiasis | 21 (31%) |
| Neurological symptoms | 2 (3%) |
ASA: American Society of Anesthesiologists; PHP: primary hyperparathyroidism.
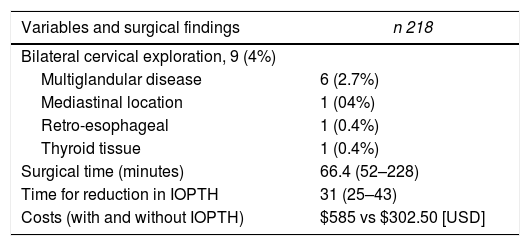
All patients underwent IOPTH monitoring (100%). Fifteen minutes after removal of the adenoma, IOPTH did not decrease in nine patients (4.2%; OR 1.9%–7.69%). In all these patients, surgery was converted to bilateral cervical exploration: 6 presented multiglandular disease (4 parathyroid hyperplasia and 2 double adenomas, confirmed by histological examination), one mediastinal, one retro-esophageal (previously, in both cases the suspicious gland in the imaging studies had been removed) and one due to thyroid tissue that pressed on the pathological left upper parathyroid gland (false positive on ultrasound and scintigraphy), while the other three glands were normal, as confirmed on histological examination. Therefore, the added value of IOPTH for the cure of hyperparathyroidism was 3.6% in our cohort (Table 2).
Variables and surgical findings.
| Variables and surgical findings | n 218 |
|---|---|
| Bilateral cervical exploration, 9 (4%) | |
| Multiglandular disease | 6 (2.7%) |
| Mediastinal location | 1 (04%) |
| Retro-esophageal | 1 (0.4%) |
| Thyroid tissue | 1 (0.4%) |
| Surgical time (minutes) | 66.4 (52–228) |
| Time for reduction in IOPTH | 31 (25–43) |
| Costs (with and without IOPTH) | $585 vs $302.50 [USD] |
IOPTH: intraoperative parathyroid hormone.
The surgical time was approximately 66.4 min (52–228 min), and, after wound closure, the average waiting time for the IOPTH result after excision of the parathyroid adenoma was 31 min (25–43 min). The length of hospital stay was 11.7 h (5–192 h). The approximate cost of IOPTH measurement plus additional operating room time was double ($585 vs $302.50 [USD] with and without IOPTH monitoring, respectively) (Table 2).
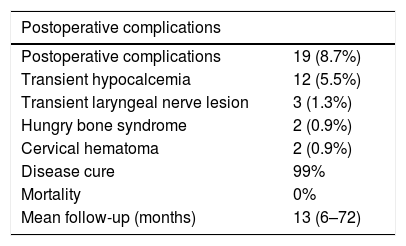
There were 19 (8.7%) postoperative complications: 12 transient hypocalcemia (5.5%), 2 hungry bone syndrome (1%), 2 cervical hematomas (1%), and 3 transient unilateral lower laryngeal nerve palsy (1.3%). There was no mortality in our series. After six months of follow-up, the disease cure rate (normal serum calcium values, no symptoms of hyperparathyroidism) was 99% (216/218 patients). The two patients with persisting hyperparathyroidism after six months of postoperative follow-up were not from the group of patients in which IOPTH did not decrease. All patients continued their follow-up with the Endocrinology Department for an average time of 13 months (6–72 months) (Table 3).
Postoperative variables and complications.
| Postoperative complications | |
|---|---|
| Postoperative complications | 19 (8.7%) |
| Transient hypocalcemia | 12 (5.5%) |
| Transient laryngeal nerve lesion | 3 (1.3%) |
| Hungry bone syndrome | 2 (0.9%) |
| Cervical hematoma | 2 (0.9%) |
| Disease cure | 99% |
| Mortality | 0% |
| Mean follow-up (months) | 13 (6–72) |
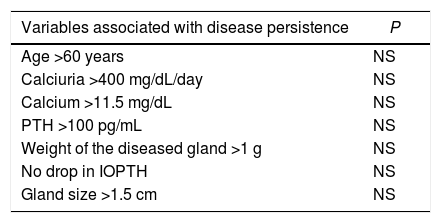
No statistical significance was found between the different risk factors evaluated and the persistence of the disease in the postoperative period (Table 4).
Analysis of variables associated with disease persistence.
| Variables associated with disease persistence | P |
|---|---|
| Age >60 years | NS |
| Calciuria >400 mg/dL/day | NS |
| Calcium >11.5 mg/dL | NS |
| PTH >100 pg/mL | NS |
| Weight of the diseased gland >1 g | NS |
| No drop in IOPTH | NS |
| Gland size >1.5 cm | NS |
NS: not significant; IOPTH: intraoperative parathyroid hormone.
The objective of this study was to analyze the usefulness of monitoring IOPTH during minimally invasive parathyroidectomy for parathyroid adenoma in patients with two coinciding preoperative localization studies. We found that: (a) in only 4.2% of patients did the IOPTH value not decrease after excision of the affected gland according to preoperative localization studies; (b) surgical time increased by 31 min when waiting for the result from the third IOPTH measurement, and costs increased approximately two-fold when tested.
Approximately 50%–60% of patients with primary hyperparathyroidism have matching preoperative localization studies8. There is no doubt about the usefulness of IOPTH in the remaining 40% of patients with differing preoperative studies8,9 and in patients with a single positive preoperative localization study10,11. However, the usefulness of IOPTH in patients with coinciding preoperative localization studies remains controversial. Those who support its usefulness argue that, among patients with primary hyperparathyroidism, approximately 10% have multiglandular disease that can only be identified and cured by observing the four parathyroid glands12–14. Accordingly, a prospective study was conducted that included 350 patients who underwent bilateral cervical exploration for sporadic primary hyperparathyroidism, all of them with coinciding preoperative studies. Single-gland disease was identified in 79% of all patients. However, up to 15% of patients with concordant studies and an adequate drop in IOPTH had an additional abnormal parathyroid gland on bilateral neck examination. Interestingly, IOPTH monitoring did not detect multiglandular disease in all cases14. Clerici et al.15 published a study in which a cervical exploration was performed by different approaches with IOPTH monitoring for primary hyperparathyroidism in 69 patients, reporting a 75% failure rate in the intraoperative detection of multiglandular disease. However, two years later, Carneiro and Irvin16 compared the results of parathyroidectomy between bilateral cervical exploration and the IOPTH-guided technique and showed that there was no significant difference between the two groups. The importance of this finding lies in the fact that, when faced with an enlarged gland, gland function may be normal. However, several studies have shown excellent results performing a minimally invasive parathyroidectomy without using IOPTH monitoring, in patients with coinciding preoperative localization studies1,17–19.
The combination of scintigraphy and ultrasound for the localization of a single adenoma has an accuracy of approximately 94%–99% and a surgical success rate of approximately 99%9,20–22. Gawande et al.9 demonstrated that the use of IOPTH monitoring could only add a marginal benefit in patients with concordant preoperative localization studies, increasing the risk of negative bilateral cervical examinations. In addition, Stalberg et al. conducted a retrospective study that included 100 patients who had undergone MIP with IOPTH monitoring for sporadic hyperparathyroidism. The precision of the added value of the PTH measurement was 1%, leading to the conclusion that it was not relevant intraoperatively and that patient selection based on preoperative surgical studies can contribute significantly to the cure of the disease23.
Another reason for controversy is the criteria chosen to define surgical success, since it is not equivalent for the detection of multiglandular diseases and for predicting the cure of the disease. Barczynski et al.24 showed that the Miami criteria followed by the Vienna criteria are the most precise for predicting intraoperative cure. However, the Rome criteria followed by the Halle criteria were the most useful in the intraoperative detection of multiglandular disease. According to these results, based on the Miami criteria, we had a positive predictive value of 99% for intraoperative cure of the disease and, following the Halle criteria, we were able to detect six out of nine patients with multiglandular disease.
The American Association for Endocrine Surgery strongly suggests the use of IOPTH monitoring for minimally invasive parathyroidectomies and, when IOPTH is not available, bilateral neck exploration should be the surgery of choice5. On the other hand, and according to our study, the European Society of Endocrine Surgeons recommends the use of IOPTH only when preoperative studies do not coincide or in patients who had undergone previous parathyroidectomy25.
The limitations of this study include its retrospective nature, which is the main limiting factor. In addition, a head-and-neck surgeon participated in all surgical procedures, so conclusions must be drawn with caution when extrapolating the results to hospitals where surgeries are performed by general surgeons. Furthermore, a control group was not included to compare the results obtained.
ConclusionIOPTH monitoring could be omitted in patients with matching ultrasound and scintigraphy results for the localization of parathyroid adenomas in PHP and could achieve a high cure rate, avoiding increased surgical time and costs.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Laxague F, Angeramo CA, Armella ED, Valinoti AC, Mezzadri NA, Fernández Vila JM. Estudios preoperatorios coincidentes para el diagnóstico de hiperparatiroidismo primario por adenoma simple: ¿podemos evitar la PTH intraoperatoria? Cir Esp. 2021;99:572–577.