The field of laparoscopic surgery has experienced an exponential growth in recent years. Despite great progress in this field, standard laparoscopic tools have not been optimally developed and still have some deficiencies when it comes to mobility and ergonomics.
Robotic surgery has attempted to solve these problems by improving the articulation of surgical instruments. However, it presents a series of disadvantages, among which are its high cost, low availability and the need for specific training, which conditions its profitability and hinders widespread use.
We present the results of a prospective clinical series of 20 cases in which the safety, efficacy and ergonomics of FlexDex® have been tested for performing laparoscopic intracorporeal sutures. The result is a safe and functional tool that offers both control and precision in its handling, while improving the ergonomics of the surgeon. This device represents an alternative that combines the precision and range of movements of robotic surgery with the greater availability of conventional laparoscopy.
El campo de la cirugía laparoscópica ha experimentado un crecimiento exponencial en los últimos años. A pesar de los grandes avances en este campo, las herramientas laparoscópicas estándar no han logrado su desarrollo óptimo, presentando ciertas deficiencias en lo que a movilidad y ergonomía se refiere.
La cirugía robótica ha intentado aportar soluciones a estos problemas, sin embargo, existen inconvenientes, entre los que se encuentran su elevado coste, escasa disponibilidad y la necesidad de capacitación específica, lo que condiciona su rentabilidad y generalización de uso.
Presentamos los resultados de una serie clínica prospectiva de 20 casos, en los que se ha testado la seguridad, eficacia y ergonomía de FlexDex® para la realización de suturas intracorpóreas laparoscópicas. El resultado muestra una herramienta segura y funcional que ofrece control y precisión en su manejo, además de mejorar la ergonomía del cirujano. Este dispositivo supone una alternativa que combina la precisión y el rango de movimientos de la cirugía robótica, con la mayor disponibilidad de la laparoscopia convencional.
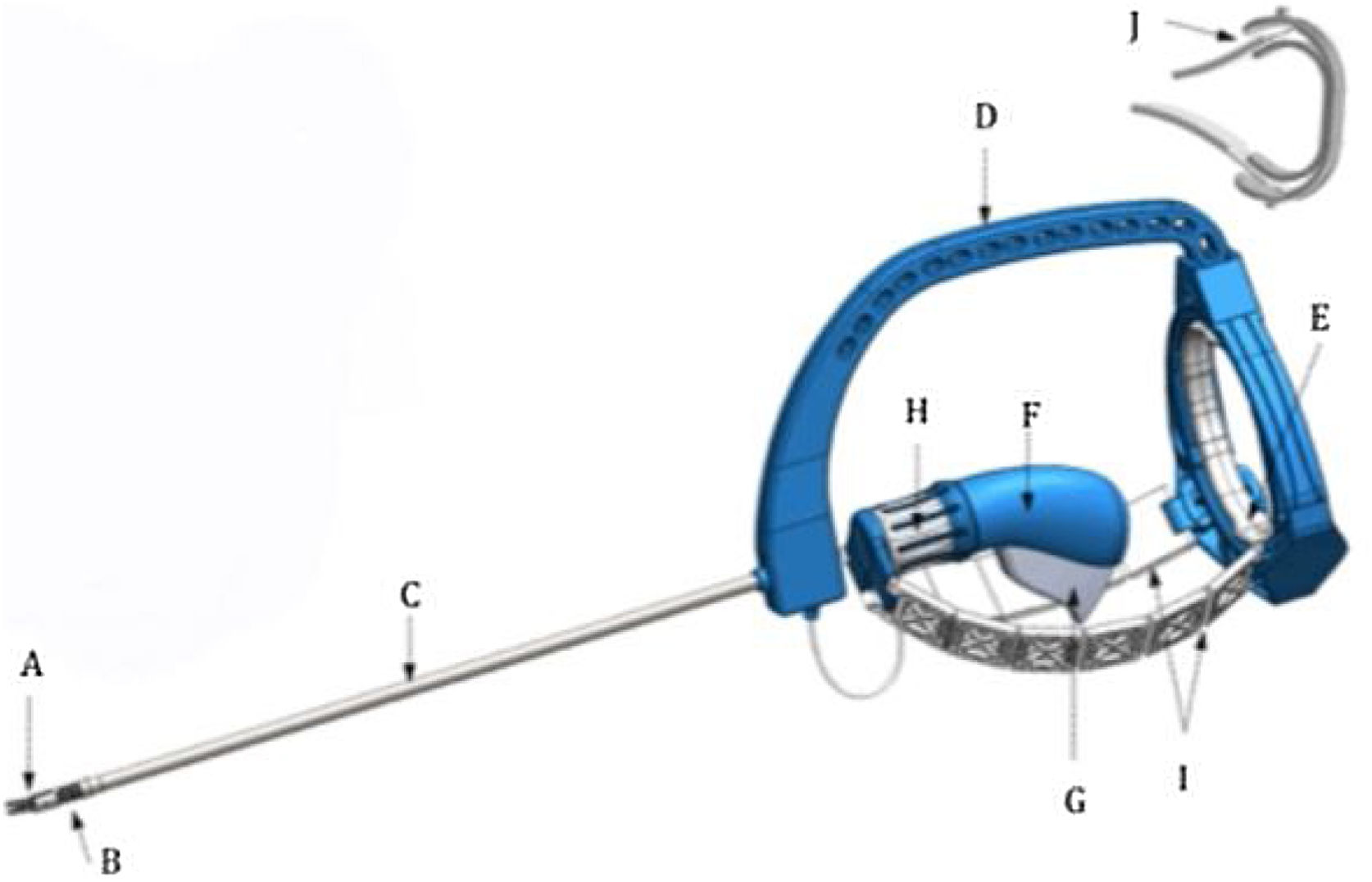
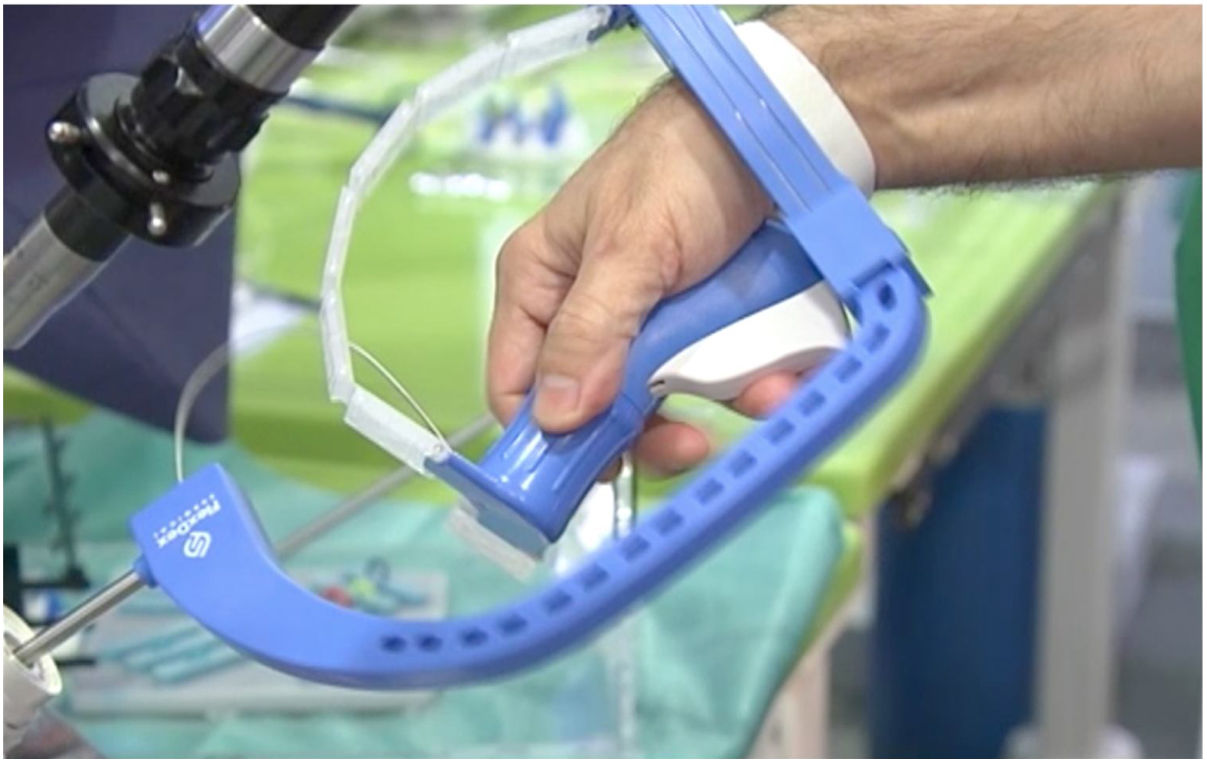
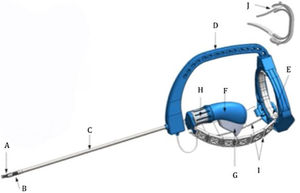
In recent years, due to the advances in laparoscopic surgery techniques and instrumentation, different fields of innovation have emerged, including robotic surgery. While improved functionality is a common goal, achieving it without a significant increase in cost remains a challenge. In this context, a new tool has emerged, the FlexDex® mechanized arm (FlexDex Surgical®, Brighton, Michigan, USA) (Fig. 1), which combines the precision and range of motion of robotic surgery with greater accessibility.
The primary objective of this study was to evaluate the safety of the FlexDex® device, and the secondary objectives were to verify its effectiveness and ergonomics. To this end, we conducted a series of surgical procedures with progressively more complex laparoscopic sutures.
Surgical techniqueWe present a prospective series of 20 laparoscopic procedures that demonstrate the initial experience in our environment with the FlexDex® mechanical arm, used in different surgical techniques requiring manual suture. The study was carried out in two clinical phases of increasing technical difficulty after prior training in an experimental operating room. Initially, 10 Nissen fundoplications were performed, and later the device was used in more complex procedures: four TAPP hernia repairs, four rectal sacropexies, and two reinforcements of colorectal anastomoses.
In all procedures, we used three-dimensional vision (Karl Storz 3D) and 30° optics, which we consider essential for proper execution of the procedures with FlexDex®. All interventions were performed by two surgeons who are experts in minimally invasive surgery. Depending on the type of procedure performed, the robotic arm was utilized for a different purpose and location. For the Nissen fundoplication, it was used to suture the crura and to create the fundoplication; during the TAPP, to anchor the prosthesis and peritoneal closure; in the rectal sacropexy, to attach the prosthesis to the rectum and promontory; and in colorectal anastomoses at risk, for anastomotic reinforcing suture.
To present the surgical technique and particularities of the FlexDex®, we will refer to the Nissen fundoplication, as it is the largest series and included the first 10 cases we performed.
After anesthesia induction and positioning of the patient with the legs lowered, a 12 mm optical trocar was placed in the navel, an 11 mm trocar in the left pararectal position for FlexDex® and the insertion/withdrawal of needles, and three 5-mm trocars (right pararectal, subxiphoid, left anterior axillary line). It was necessary to separate the trocar through which the FlexDex® was inserted at least 8 cm from the optical trocar and the assistant, thus avoiding forced positions and optimizing the ergonomics for the operator. This spacing between trocars is necessary to prevent space conflicts when rotating the arc of the device. It is important to note that when the suture is introduced into the abdomen, the tip of the device must be accompanied with the left hand during its insertion into the trocar.
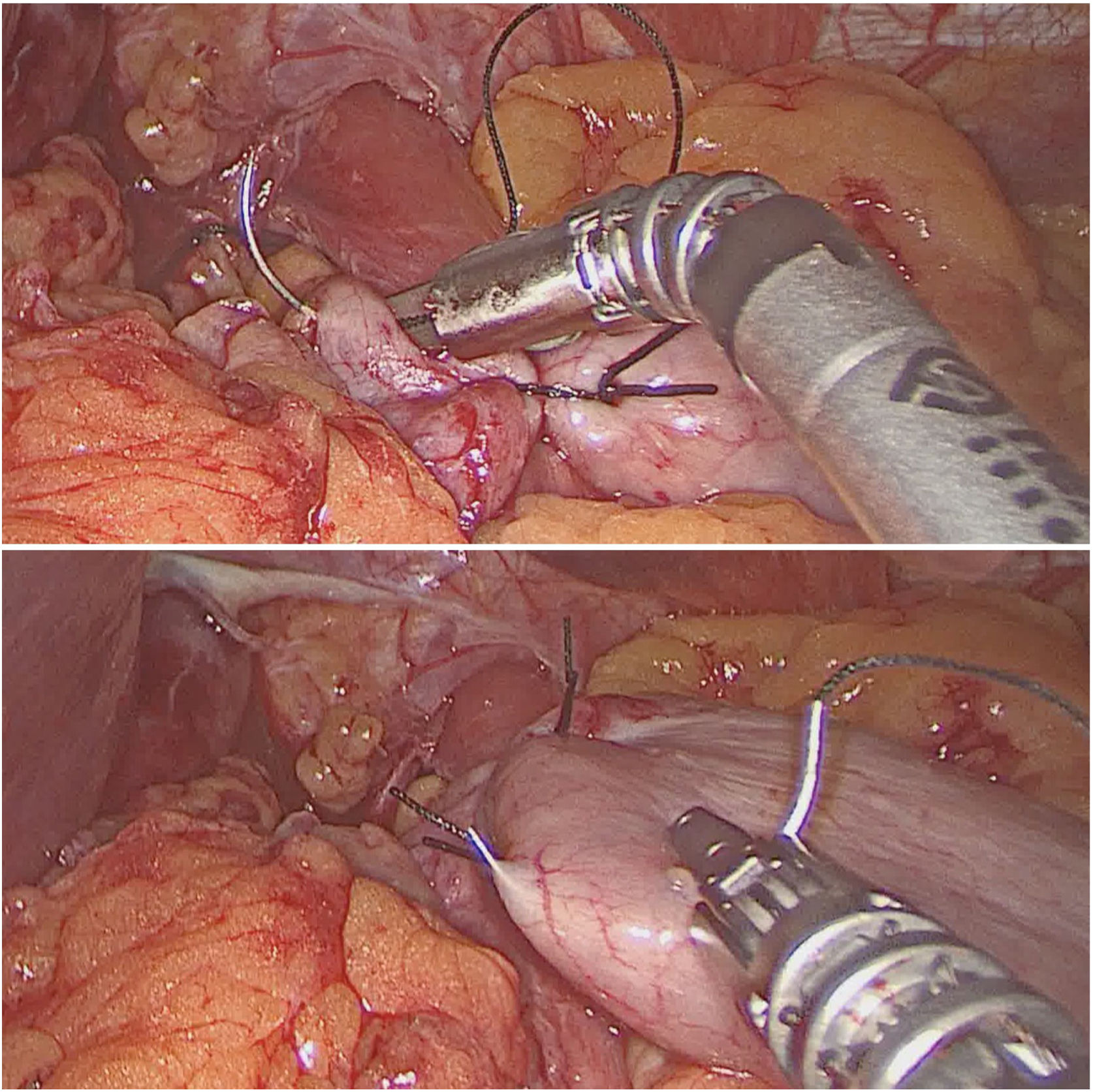
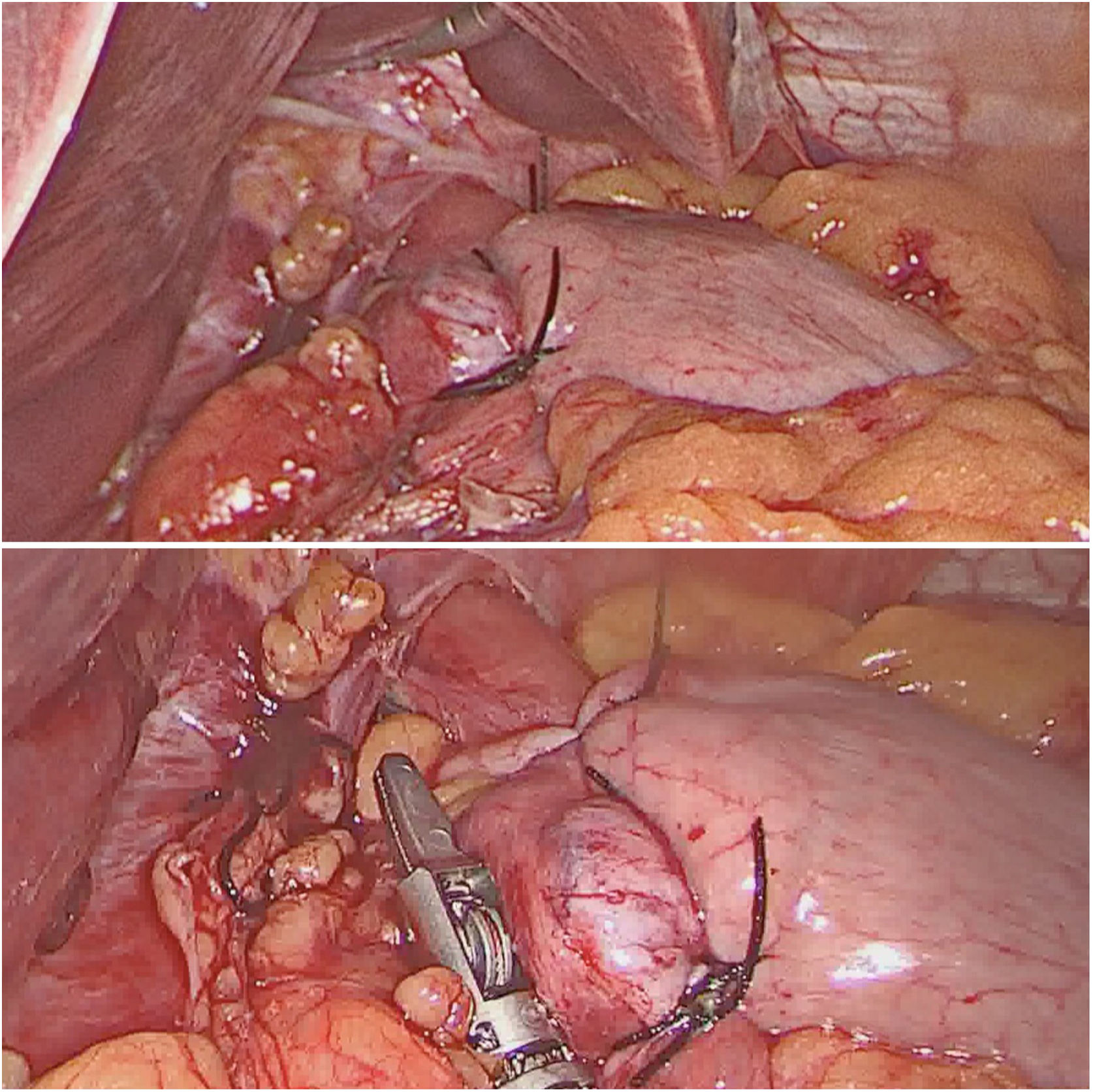
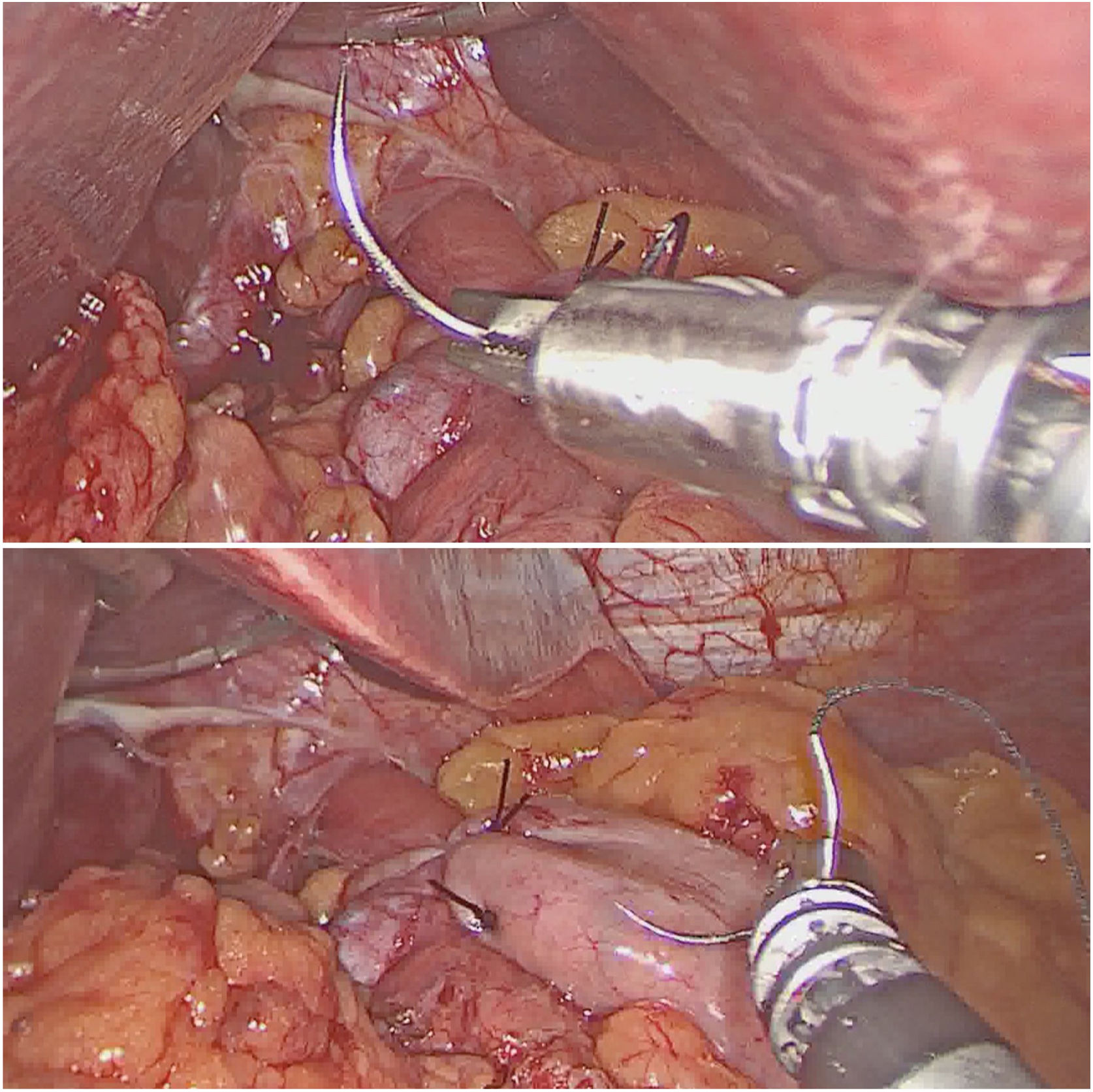
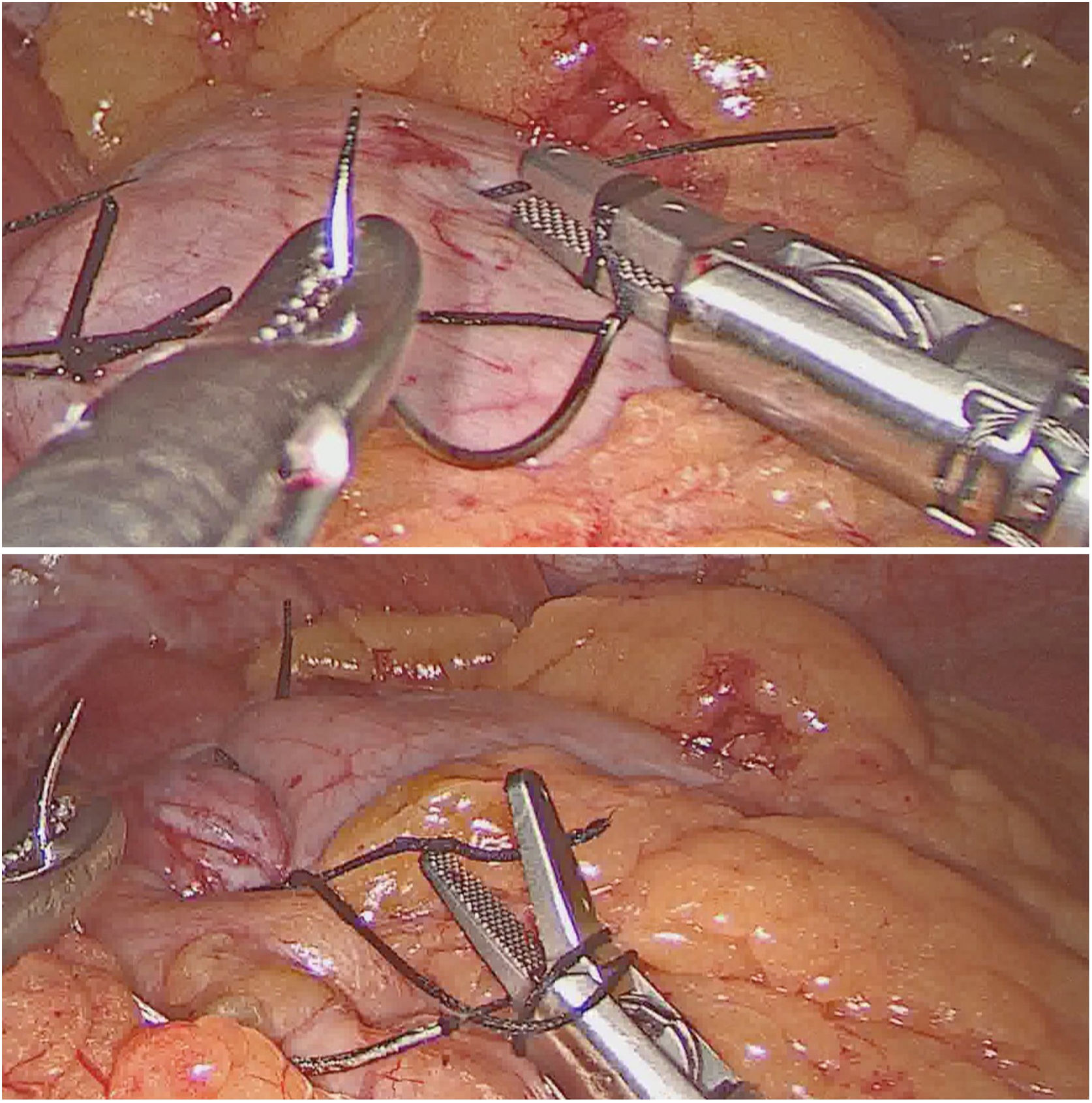
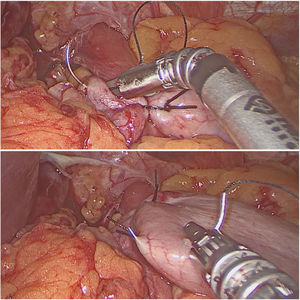
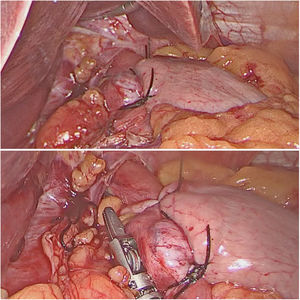
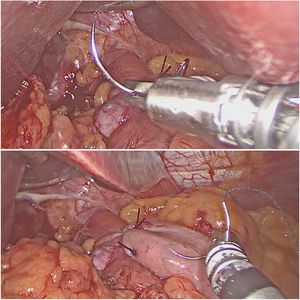
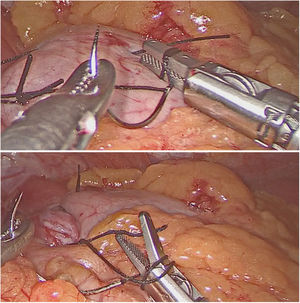
The antireflux surgery was performed following the Nissen technique, performing hiatal repair after a wide esophageal dissection, into which the FlexDex® instrument was inserted to perform the 2−0 silk suture in the lower part of the hiatus, one supraesophageal suture and three interrupted sutures (Fig. 2) to create the fundoplication, respecting a distance of approximately 1 cm between them (Fig. 3). The surgical suture was performed, achieving correct positioning of both the needle holder and the needle (Fig. 4). Likewise, intracorporeal knotting was facilitated thanks to the articulation of the distal part of the needle holder, largely avoiding tissue traction (Fig. 5).
To evaluate this technology, a visual analog scale (VAS) was used for participating surgeons to subjectively evaluate the device immediately after its use, evaluating the safety, efficacy and ergonomics of the tool from one to 10. The range of values had a mean of 6–7 during the training period, which rose to 9–10 after clinical use of the instrument. In their evaluations, the surgeons highlighted that FlexDex® allowed for sutures and knots to be executed with considerably less effort than with the conventional laparoscopic technique, improving the ergonomics and efficiency for the operator.
DiscussionMinimally invasive surgery has flourished in recent years, as it provides several advantages:1 smaller incisions, shorter hospital stays, less postoperative pain, and faster patient recovery.2 However, laparoscopic techniques are associated with several technical challenges, such as restricted movement of straight laparoscopic instruments, two-dimensional vision, and poor ergonomics for surgeons.2
One of the most effective improvements in the field of minimally invasive surgery was the implementation of robotic systems. The DaVinci® system (Intuitive Surgical, Sunnyvale, California, USA) enables surgeons to operate with greater precision, range of motion, ergonomics, and comfort.3 However, it also presents a series of drawbacks, such as the lack of haptic perception for the surgeon on the tissues4 or the limited accessibility and maneuverability in the abdominal cavity due to the size of the robotic arms.5 Currently, the Da Vinci® system is the only robotic surgical platform available on the market that enables remote manipulation in minimally invasive surgery. This technology has a significant cost,6 which would explain why its use has not yet become widespread.7
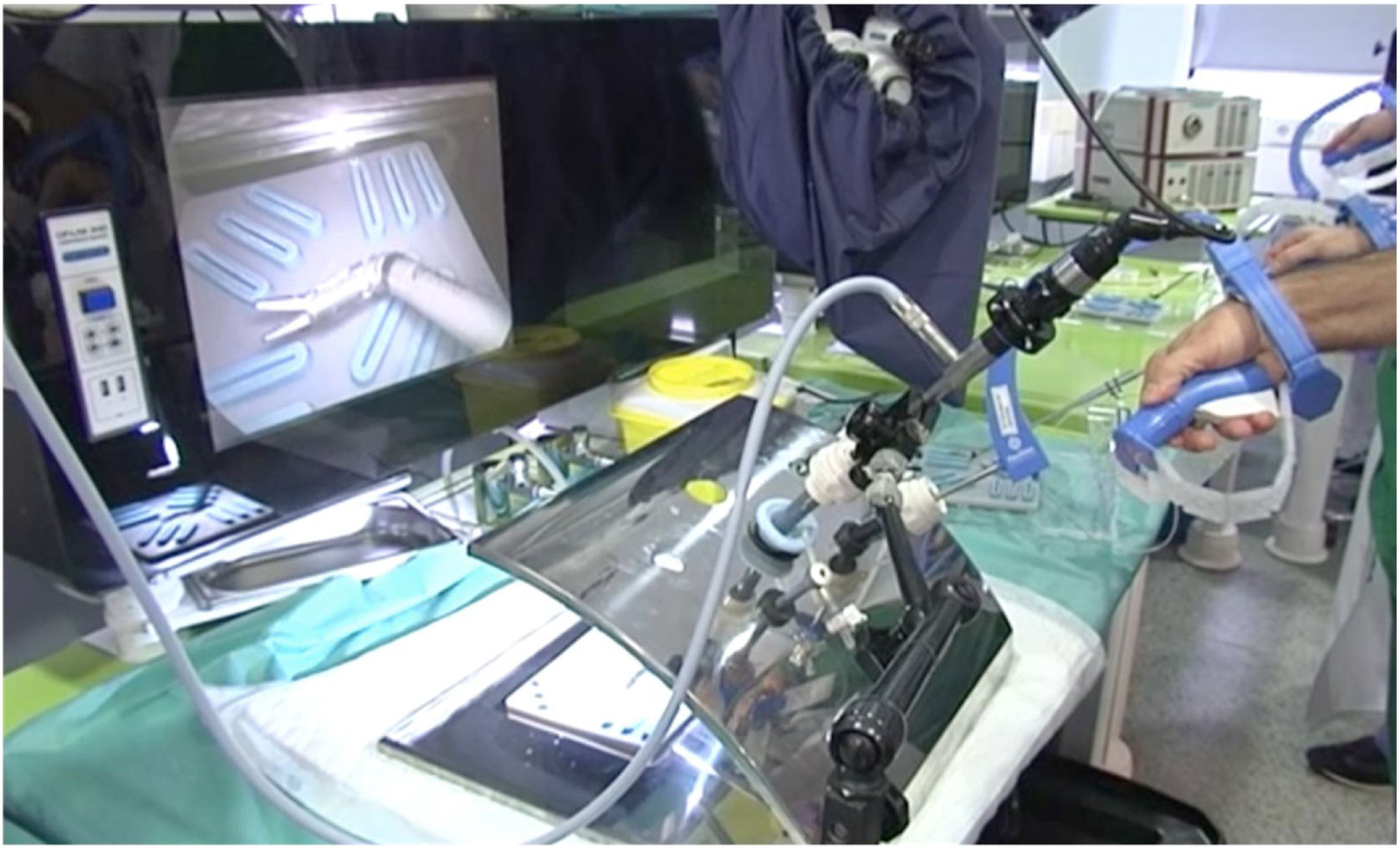
Since the first laparoscopic cholecystectomy in 1985, there has been little progress in laparoscopic instruments. Standard-use tools fail to optimize mobility in limited spaces.3 The FlexDex® system is a technology developed on the three axes and integrated into a conventional laparoscopic instrument, which transmits the movements of the surgeon’s hand, wrist and arm from outside the patient to an end-effector inside the patient’s body (Fig. 6). Its greater accessibility enables suturing in areas with difficult access where mobility with conventional laparoscopic instruments is not optimal, such as in the case of the pelvis and hiatus. It also allows surgeons to avoid forced hand movements thanks to the transmission of a wide freedom of movement at the tip of the device (Fig. 7).
As during the early days of conventional laparoscopy, the effort of the operator will be essential to optimize the potential of FlexDex® and facilitate its implementation.3 In this case, the main difficulty is the need to coordinate the movements of the left hand (which will handle a standard laparoscopic instrument), with those of the right hand, whose movements are transmitted inverse to conventional laparoscopy when using FlexDex®.
In 2017, Criss et al3 published the first experience with the use of FlexDex®, performing reoperation of a laparoscopic Nissen fundoplication. They concluded that the use of FlexDex® had improved the surgeon’s operative control within a reduced space, and intracorporeal knotting could be done with considerably less effort. Subsequently, there have been few studies about the technology and use of FlexDex®. One that we should highlight is the prospective simulation study carried out by Criss et al. in 2019,8 where the ergonomics, difficulty of use and performance of FlexDex® were evaluated in different groups using this instrument for the first time. The surgeons who operated with FlexDex® described improved ergonomics and more effective intracorporeal sutures in difficult-to-access locations.
In our case, the instrument was evaluated by two surgeons who are experts in laparoscopic surgery and who had undergone training in pelvi-trainer and a porcine animal model for a total of 10 h. In our opinion, prior to handling FlexDex®, the surgeon must be trained in laparoscopic surgery and have complete mastery of intracorporeal sutures.
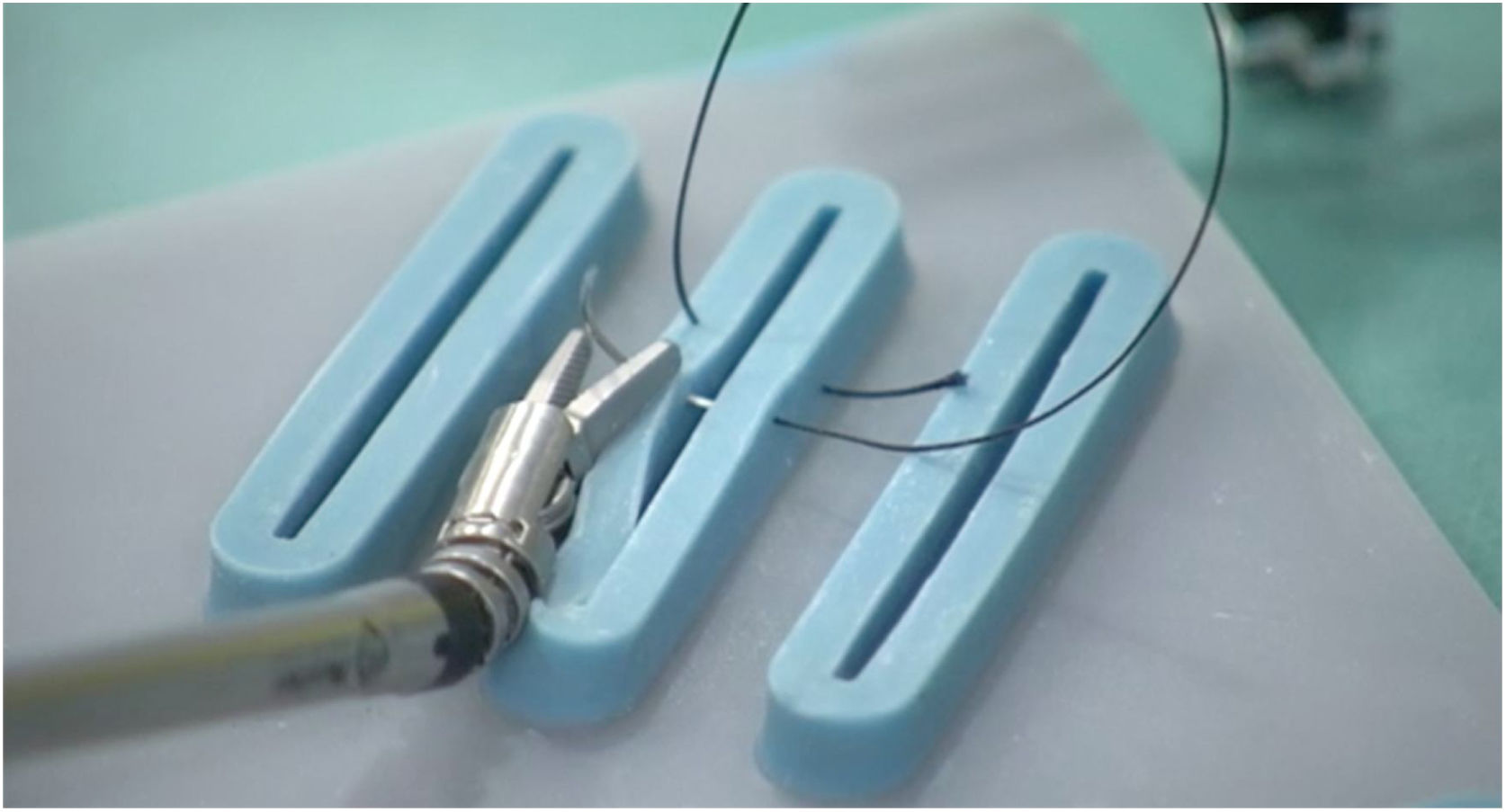
Furthermore, we recommend a sequential approach to handling the instrument, starting the simulation in a pelvi-trainer or model (Fig. 8), continuing with organic tissue and a live animal model (if available), until adequate right-left hand coordination is achieved. Once this goal is met, maximum efficacy with the device will be reached. However, for surgeons who have not undergone a prior training period, it does not seem prudent to make clinical use of this tool, as it could result in increased surgical time and possibly affect patient safety.
None of our patients presented intraoperative complications, which was the primary objective of the study in terms of safety. Given that these 20 cases represent an initial experience in the use of FlexDex®, the adaptation to the tool could have compromised the surgical time; however, it did not increase.
Given these results, it is expected that FlexDex® may evolve to become a functional option that is economically affordable, especially in hospitals with no access to robotic surgery. In our opinion, it could provide an excellent alternative to robotic systems in complex surgical procedures, offering surgeons the precision and control they desire, while maintaining a balance between cost, outcome and patient benefit. In addition, its current needle driver opens the door to the addition of a wide range of end-effectors, allowing for the use of a dissector, scissors or to apply energy, either associated with these terminals or in the form of tissue sealants.
FundingThis study has received no funding of any kind.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Jiménez ML, Castro-Diez L, Aguirrezabalaga-González J, Noguera-Aguilar JF. Sutura laparoscópica mecanizada con FlexDex Surgical System® para ubicaciones anatómicamente difíciles. Cir Esp. 2021;99:222–228.