Esophageal cancer is the seventh most common malignant neoplasm in the world1. Esophagectomy continues to be the mainstay of treatment for these patients. During surgery, restoring the continuity of the digestive tract is critical, both in terms of risk of postoperative complications as well as subsequent quality of life. The most common technique for reconstruction is the creation of a gastric tube. The problem arises when the stomach is not available, which can be due to the ingestion of caustic substances compromising the esophagus and stomach, previous gastrectomy, or gastric extension of a distal esophageal tumor. In these cases, the alternatives include the right or left colon and free jejunal interposition with vascular anastomosis. Another less used alternative is Roux-en-Y reconstruction. The use of the jejunum was first described by Roux in 19072. The jejunum is an ideal choice because of its size match with the esophagus, the capacity for intrinsic peristalsis after reconstruction, and the fewer anastomoses required. The main drawback is the difficulty to mobilize the jejunum from the abdominal cavity to the mediastinum while maintaining optimal perfusion3.
Indocyanine green (ICG) fluorescence is an emerging intraoperative method. It enables us to evaluate the patient for and optimize lymphadenectomy, while also evaluating tissue perfusion in order to avoid using tissues with poor perfusion, thereby preventing postoperative ischemic complications4–6. Thus, the use of indocyanine green could be a good tool when Roux-en-Y reconstruction is planned (in which perfusion is essential) by evaluating jejunal duct perfusion conditions throughout the surgery and avoiding the need to perform a vascular anastomosis.
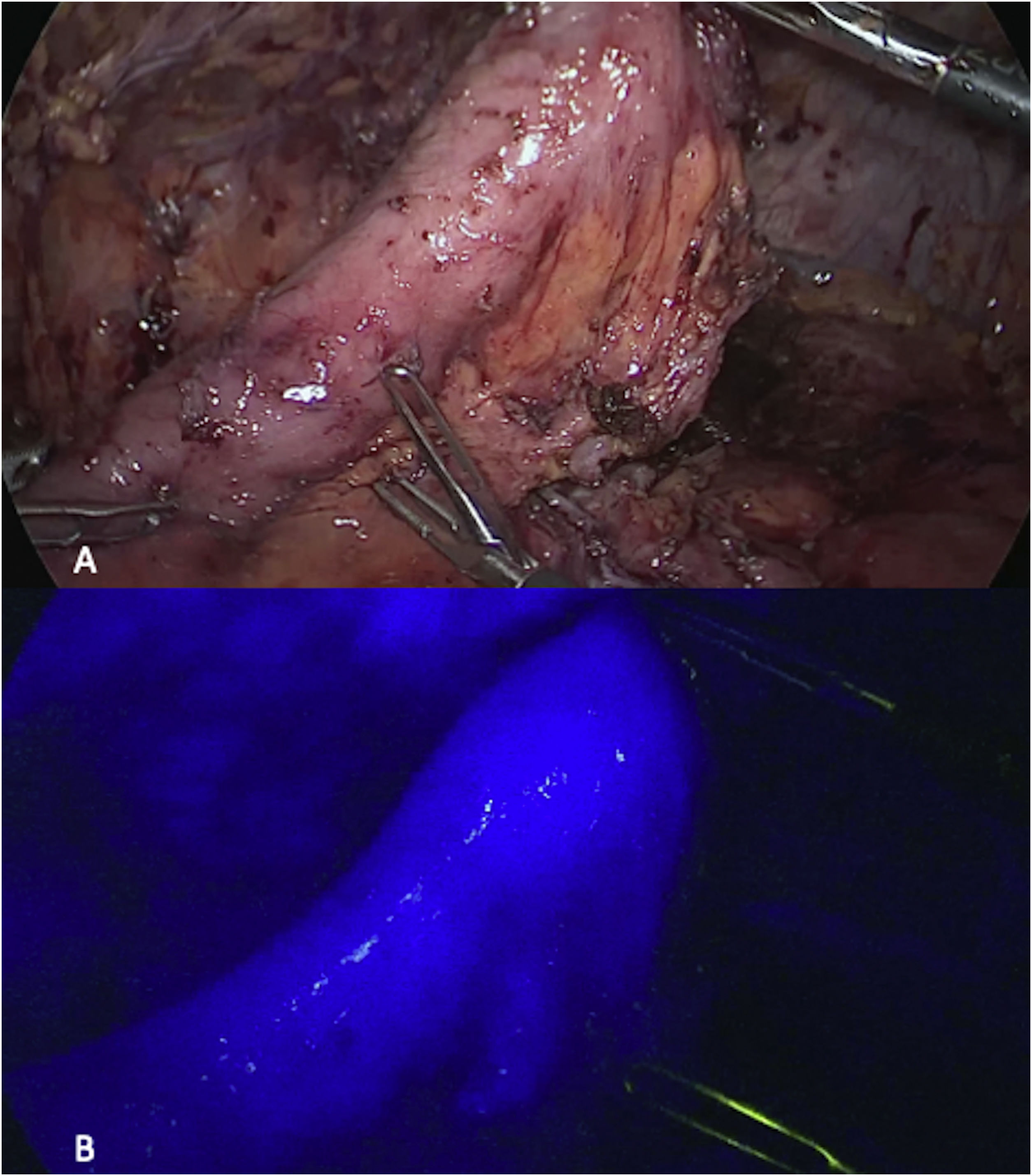
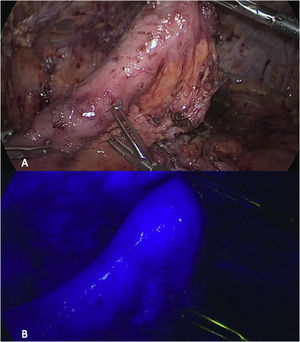
We present the case of a 57-year-old man with a previous open total gastrectomy due to gastric cancer. During follow-up, a 2 cm lesion was found in the esophageal mucosa immediately above the esophagus-jejunal anastomosis, and the biopsy confirmed adenocarcinoma. The extension study was negative, so we planned to perform surgical resection using a minimally invasive Ivor-Lewis type surgery with Roux-en-Y reconstruction. The abdominal phase began with a laparoscopic approach, releasing the adhesions from the previous surgery. After restoration of the anatomy, we performed complete dissection of the anterior esophageal-jejunal anastomosis together with the posterior dissection of the jejunum 10 cm below the anastomosis using a linear endostapler. With the distal jejunum free, we started to mobilize the mesentery, evaluating the vascular distribution and jejunal perfusion using indocyanine green. After identifying the jejunal arch by direct vision, we began dissecting the vessels while avoiding injury to the main jejunal vascular supply in order to achieve better mobilization of the jejunum. The final jejunal perfusion was evaluated to confirm optimal vascular supply before ending the abdominal phase (Fig. 1A, B).
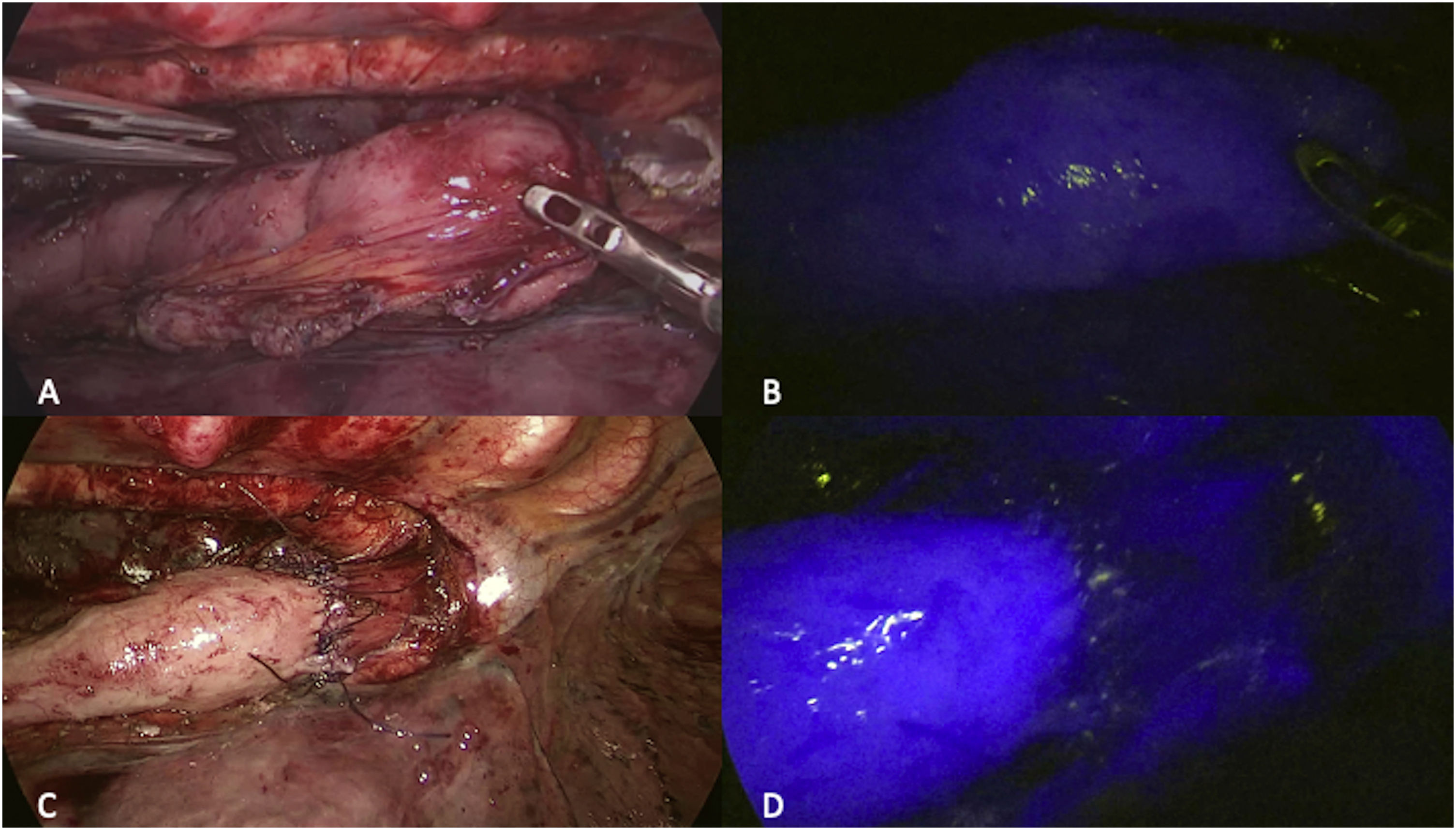
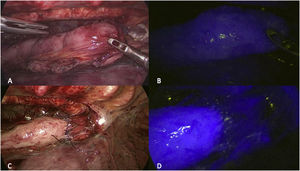
The semiprone position was used for the thoracic phase. Complete dissection of the esophagus was performed down to the area of the azygous vein. The proximal margin was dissected with a harmonic scalpel. The jejunal loop was mobilized to the area of the anastomosis to confirm that there was no tension in the tissues (Fig. 2A). Another indocyanine green test was used to assess adequate perfusion when lifting the jejunum, before performing the anastomosis (Fig. 2B). An anastomosis was performed manually in two planes, ensuring that it was tension-free, and a nasogastric tube was placed before suturing the anterior side of the anastomosis. The final Roux-en-Y evaluation was performed after completing the esophagojejunal anastomosis, demonstrating adequate and optimal perfusion of the jejunal loop (Fig. 2C,D).
During the postoperative period, intake was initiated on day 3, and the patient was discharged on day 7 without any postoperative complications. The pathological study confirmed a moderately differentiated adenocarcinoma with negative proximal and distal margins; the 13 lymph nodes were all negative. A computed tomography scan and endoscopy were performed at 12 months of follow-up, and no signs of tumor recurrence were found.
The use of Roux-en-Y for the posterior reconstruction of an esophagectomy has been previously described in the literature and is considered an alternative if the stomach is not available. Despite this, it is not frequently used due to the risk of jejunal loop ischemia and possible difficulty in mobilizing the jejunum through the chest. This is the first case report using indocyanine green for the preparation and evaluation of the perfusion of the jejunal duct, both in the abdominal and thoracic phases of the surgery. ICG fluorescence is a new tool that makes this type of atypical reconstruction safer and, therefore, it may be considered an adequate and valuable technique in select cases.
Please cite this article as: Navarrete A, Humeres R. Uso de verde de indocianina para la reconstrucción con Y-de-Roux posterior a esofagectomía mínimamente invasiva. Cir Esp. 2022;100:55–57.