Our objective was to assess a laparoscopic training model for general surgery residents.
MethodsTwelve general surgery residents carried out a training programme, consisting of a theoretical session (one hour) and a hands-on session on simulator (7h) and on animal model (13h). For the first and last repetitions of simulator tasks and the Nissen fundoplication technique, time and scores from the global rating scale objective structured assessment of technical skills (OSATS) were registered. Before and after the course, participants performed 4 tasks on the virtual reality simulator LAPMentor™: (1) hand–eye coordination, (2) hand–hand coordination, (3) transference of objects and (4) cholecystectomy task, registering time and movement metrics. Moreover, the residents completed a questionnaire related to the training components on a 5-point rating scale.
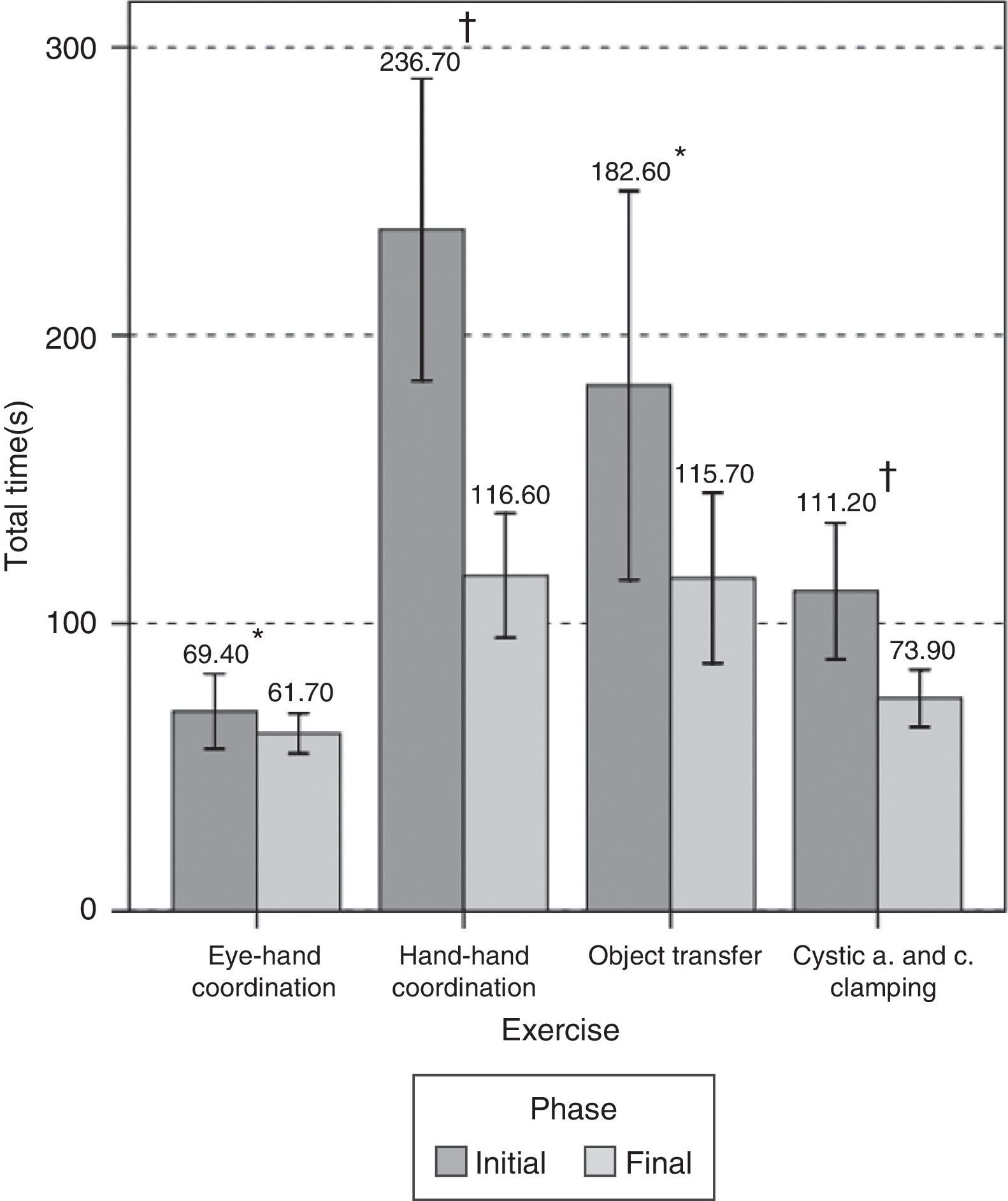
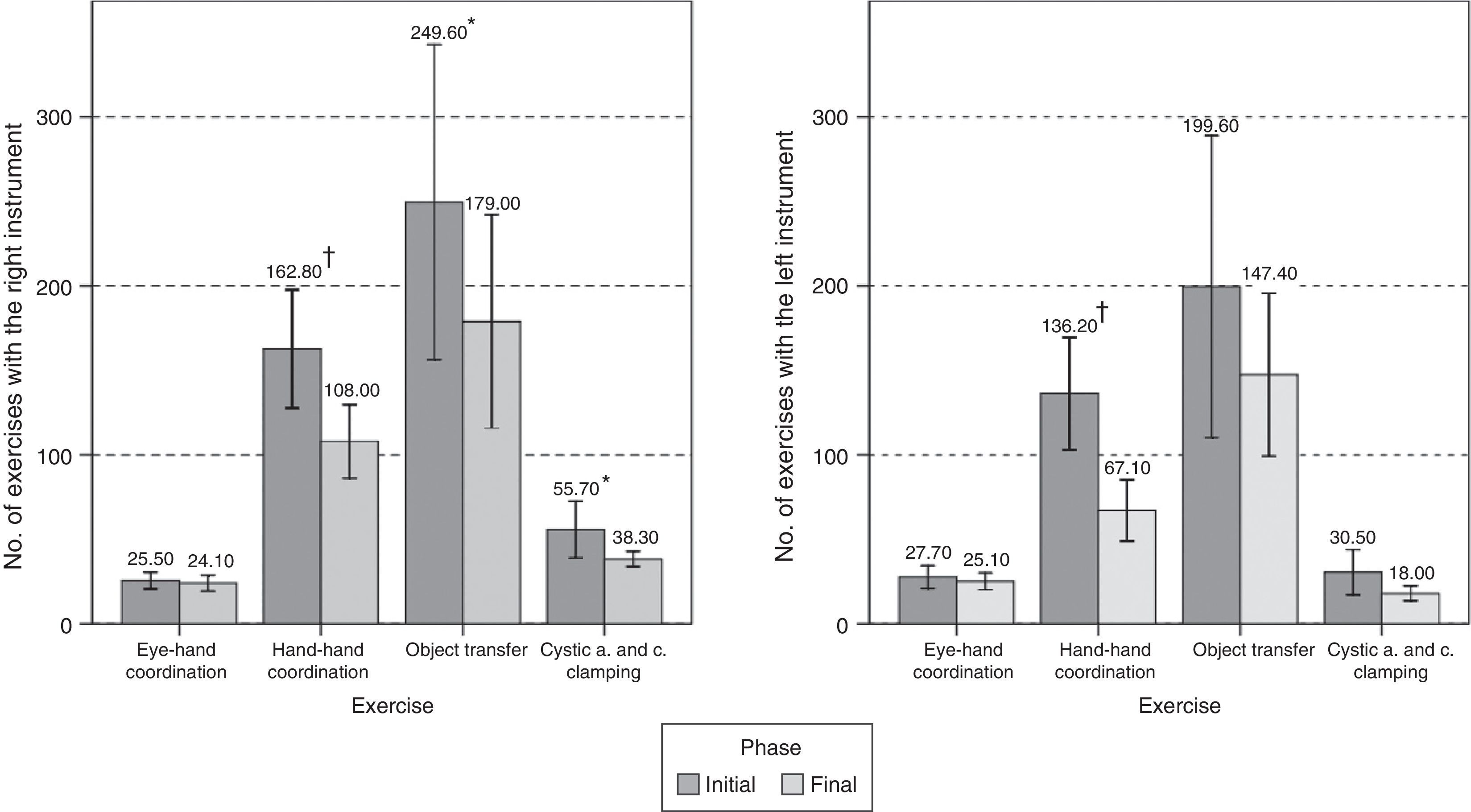
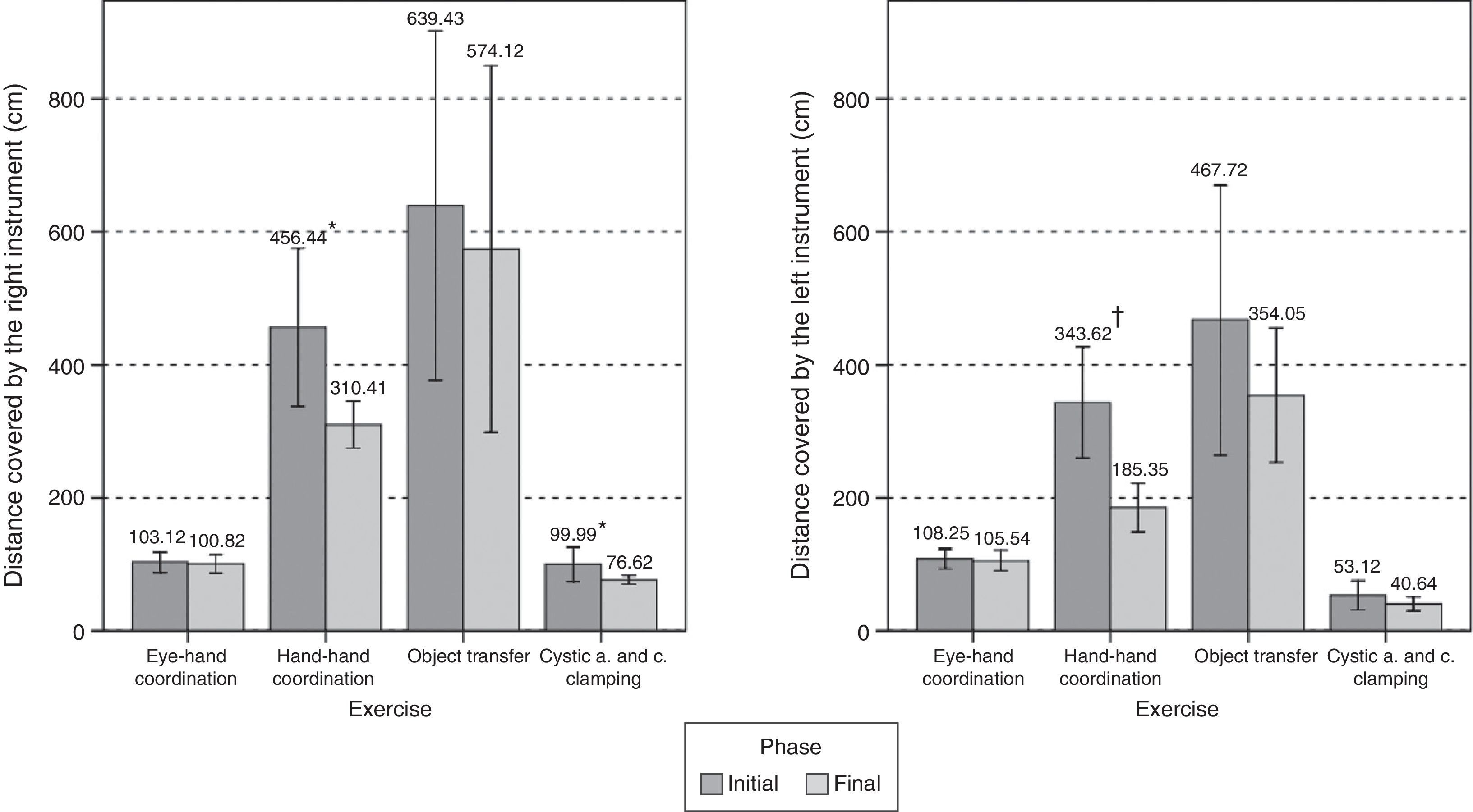
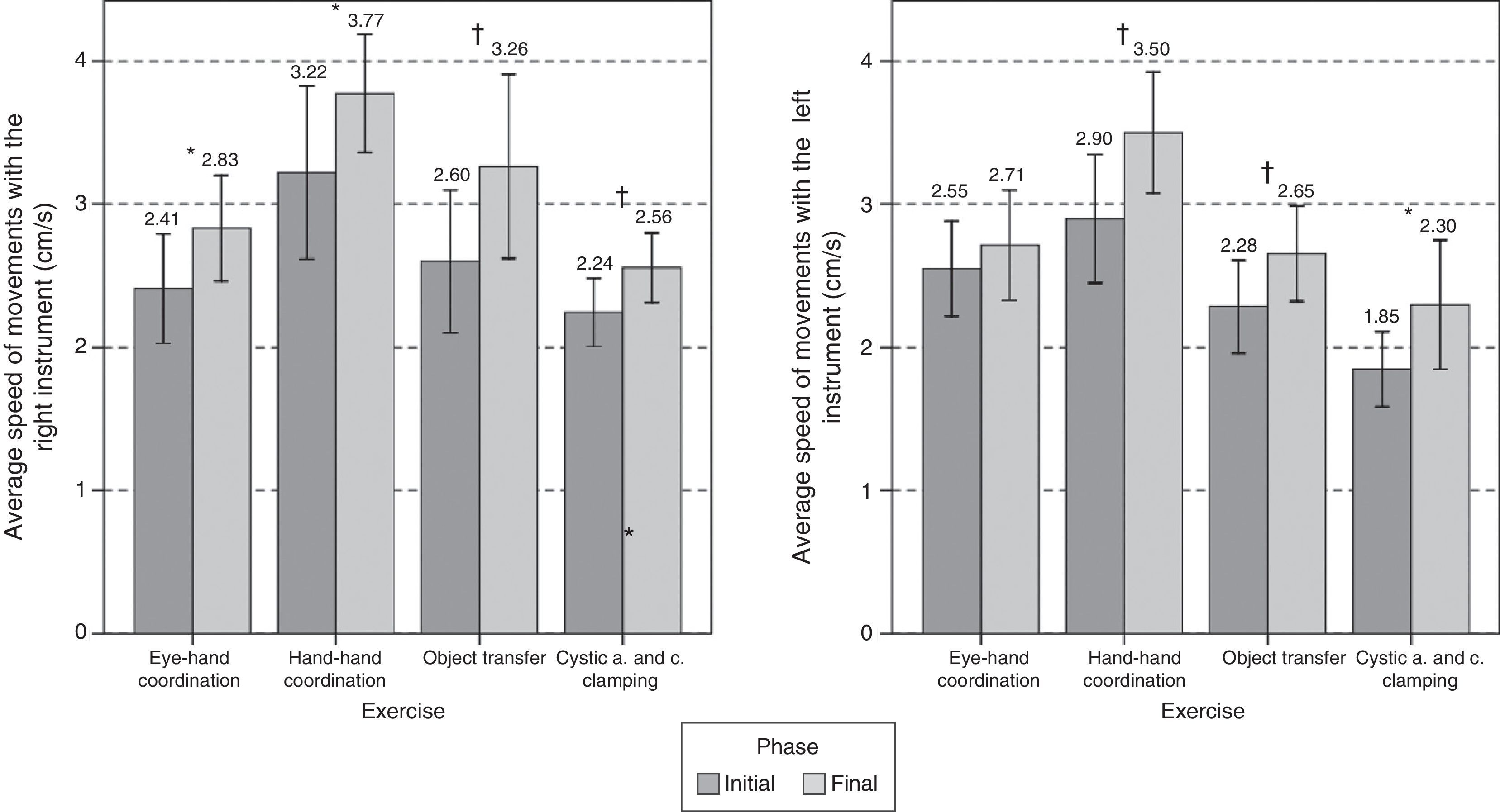
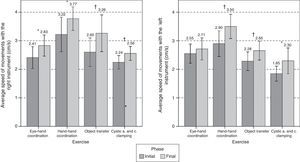
ResultsThe last repetition of the tasks and the Nissen fundoplication technique were performed faster and with a higher OSATS score. After the course, the participants performed all LAPMentor™ tasks faster, increasing the speed of movements in all tasks. Number of movements decreased in tasks 2, 3 and 4; as well as path length in tasks 2 and 4. Training components were positively rated by residents, being the suture task the aspect best rated (4.90±0.32).
ConclusionsThis training model in digestive laparoscopic surgery has demonstrated to be valid for the improvement of basic and advanced skills of general surgery residents. Intracorporeal suturing and the animal model were the best rated training elements.
Nuestro objetivo fue validar un modelo de formación en cirugía laparoscópica para residentes de cirugía general.
MétodosDoce residentes de cirugía general realizaron un programa formativo, consistente en una sesión teórica (una hora) y una sesión práctica en simulador (7h) y modelo animal (13h). En la primera y última repetición de los ejercicios y la funduplicatura de Nissen, se registró el tiempo y la puntuación de la escala de puntuación global objective structured assessment of technical skills (OSATS). Antes y después del curso, los participantes realizaron 4 ejercicios en el simulador virtual LAPMentor™: 1) coordinación ojo-mano, 2) coordinación mano-mano, 3) transferencia de objetos y 4) ejercicio de colecistectomía, registrándose las métricas de tiempo y movimiento. Además, rellenaron un cuestionario sobre los elementos formativos en una escala del 1 al 5.
ResultadosLa última repetición de los ejercicios y de la funduplicatura de Nissen se realizaron más rápido y con mejor puntuación OSATS. Tras el curso, los participantes realizaron todos los ejercicios en LAPMentor™ más rápido, aumentando la velocidad de movimientos en todos ellos. El número de movimientos disminuyó en los ejercicios 2, 3 y 4, así como la distancia recorrida en los ejercicios 2 y 4. Los elementos del programa fueron valorados positivamente. El ejercicio de sutura fue el aspecto mejor valorado (4,90±0,32).
ConclusionesEste modelo de formación en cirugía laparoscópica ha demostrado ser válido para la mejora de habilidades básicas y avanzadas de médicos residentes de cirugía general. La sutura intracorpórea y el modelo animal fueron los elementos formativos mejor valorados.
Different learning methods and training programmes have recently been described to gain skills in laparoscopic surgery.1,2 These programmes combine clinical training, such as fellowships in hospitals, and non-clinical training, such as practical modules that usually last 2–3 days, in which the use of simulators is combined with experimental models.3
The first type of training, which is mainly used in the United States and Canada, has given good training results. However, in Europe there is no common policy in this area, nor has any uniform model been suggested or developed at a community level.4
On the other hand, intensive practical courses are one of the training options most in demand, as they are compatible with surgeons’ lack of time and meets their need for additional training in advanced techniques.4 Additionally, it has also been said that courses of this type should be a basic requisite for residents.5,6 Nevertheless, they must be validated as useful learning tools.
Parallel to the development of different training modes, methods of evaluating surgical skills have evolved that make it possible to monitor learning. Of these methods, virtual simulator metrics stand out, together with observational evaluation tools and movement monitoring systems.7
The aim of this study is to objectively determine the utility of our model of laparoscopic surgery training for the acquisition of skills by general and digestive surgery residents.
MethodsStudy Subjects12 residents took part in this study. They came to our centre for a basic course on laparoscopic surgery in the year 2012. The inclusion criteria were final year general and digestive surgery residents (R4 and R5) who had also performed at least 10 laparoscopic operations as the main surgeon. Before the course, the participants filled out a demographic questionnaire which also recorded information on their previous experience in laparoscopic simulation.
Training ProgrammeAll training activities were approved by the Ethics and Animal Well-Being Committee of our Centre, and they fulfilled the requisites specified in the regulations in force at the time the study was carried out (Directive 2010/63/EU, Royal Decree 1201/2005 and Law 32/2007).
The practical courses in laparoscopic surgery lasted for 2 and a half days. The programme was based on a theoretical part (1h) and a practical part using the Simulap® physical simulator (7h) and experimental animals (13h). The theoretical part consisted of sessions on training, ergonomics, instrumentation and devices, together with laparoscopic towers. The practical part in the simulator took place on the first day of the course, and exercises were performed in increasing order of difficulty: eye–hand coordination, hand–hand coordination, cutting, dissection and suture. During the following day and a half in vivo practice took place in a porcine model, given the anatomical similarity of its gastrointestinal apparatus to that of human beings.8 During this phase those attending practiced Nissen's fundoplication and gastrojejunal anastomosis with a suture inside the body. Before practice using the simulator and animal model, the course professors carried out a demonstration to explain each exercise, the surgical technique involved and comparative porcine and human anatomy. During all of the practice on the experimental model, the animals were treated by inhaled anaesthesia, and they were under veterinary supervision at all times to supply them with the necessary anaesthesia and analgesia. On the other hand, the surgeons were supervised and tutored by surgeons with vast experience in clinical and experimental laparoscopic surgery.
The Evaluation of Surgical SkillsBefore starting the course and after it had ended the surgeons carried out 4 exercises on the LAPMentor™ virtual reality simulator (Simbionix Corporation, Cleveland, OH, United States). Execution of the exercises was evaluated using the metrics generated by LAPMentor™: total time, number of movements, distance covered and average speed of left and right instrumentation. These 4 exercises are described below.
Exercise 1. Eye–hand coordination, in which the aim is to touch 20 balls, 10 blue ones (with the right hand) and 10 red ones (with the left hand), following the random order shown on screen.
Exercise 2. Hand–hand coordination, with the mission of extracting 9 balls from a gel and depositing them in a recipient.
Exercise 3. The transfer of objects. This consists of placing 2 objects in the position indicated by the simulator by transferring them from one hand to the other.
Exercise 4. Placing clips and cutting the artery and cystic duct.
Finally, during the phase of training in the simulator and experimental model the time taken to execute the first and last repetition of the exercises and Nissen's fundoplication was recorded. The exercises and procedures were evaluated blind on the validated overall scoring scale “objective structured assessment of technical skills” (OSATS)9 by 2 expert surgeons who were not involved in the study.
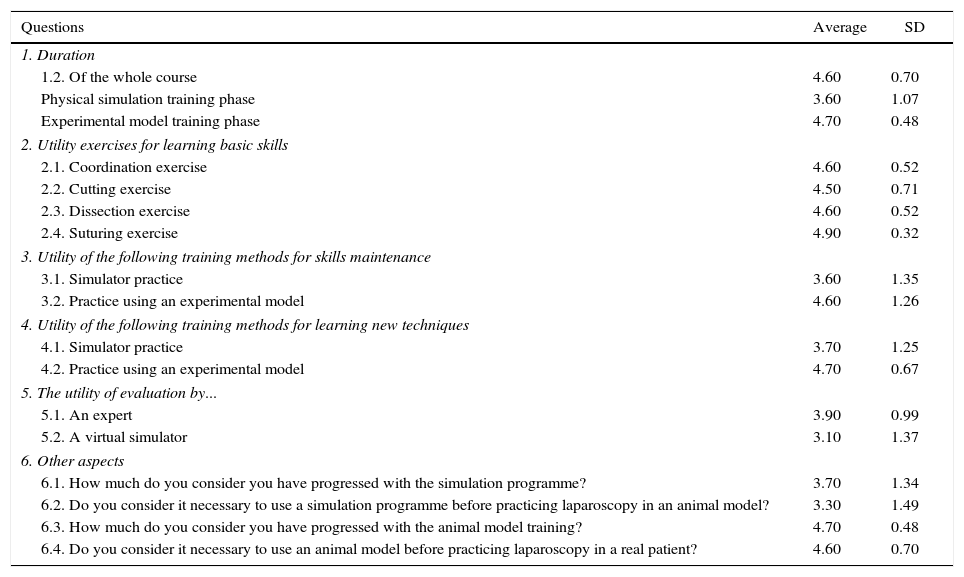
Subjective EvaluationAt the end of the course the participants filled out a subjective questionnaire on the parts of the training programme (Table 1), using an evaluation of the Likert type, from 1 (very negative) to 5 (very positive).
Results of the Subjective Questionnaire on Training Programme Elements (Scale 1–5).
| Questions | Average | SD |
|---|---|---|
| 1. Duration | ||
| 1.2. Of the whole course | 4.60 | 0.70 |
| Physical simulation training phase | 3.60 | 1.07 |
| Experimental model training phase | 4.70 | 0.48 |
| 2. Utility exercises for learning basic skills | ||
| 2.1. Coordination exercise | 4.60 | 0.52 |
| 2.2. Cutting exercise | 4.50 | 0.71 |
| 2.3. Dissection exercise | 4.60 | 0.52 |
| 2.4. Suturing exercise | 4.90 | 0.32 |
| 3. Utility of the following training methods for skills maintenance | ||
| 3.1. Simulator practice | 3.60 | 1.35 |
| 3.2. Practice using an experimental model | 4.60 | 1.26 |
| 4. Utility of the following training methods for learning new techniques | ||
| 4.1. Simulator practice | 3.70 | 1.25 |
| 4.2. Practice using an experimental model | 4.70 | 0.67 |
| 5. The utility of evaluation by... | ||
| 5.1. An expert | 3.90 | 0.99 |
| 5.2. A virtual simulator | 3.10 | 1.37 |
| 6. Other aspects | ||
| 6.1. How much do you consider you have progressed with the simulation programme? | 3.70 | 1.34 |
| 6.2. Do you consider it necessary to use a simulation programme before practicing laparoscopy in an animal model? | 3.30 | 1.49 |
| 6.3. How much do you consider you have progressed with the animal model training? | 4.70 | 0.48 |
| 6.4. Do you consider it necessary to use an animal model before practicing laparoscopy in a real patient? | 4.60 | 0.70 |
SD: standard deviation.
The computer programme Statistical Package for the Social Sciences, version 15.0 (SPSS, Chicago, USA) was used for the statistical study. In connection with the sample size, in a previous study that used the OSATS scale, it was determined that the minimum number of participants for there to be a minimum relevant difference of 1.3, with an α of 0.05 and a statistical power of 0.80 had to be 9.10 Wilcoxon's non-parametric test was used for associated samples to compare the initial and final results obtained in the simulator exercises, in Nissen's fundoplication and in the LAPMentor™. Cronbach's alpha coefficient was calculated to determine the reliability between evaluators for the OSATS scores. A value of P<.05 was considered to be significant.
ResultsAll of the participants completed all of the phases of the training activity. The population consisted of 9 women and 3 men. Half of the surgeons were right-handed.
8 participants had taken part as assistants in more than 50 and less than 100 laparoscopic procedures, while the others had assisted in more than 10 and less than 50 surgical procedures. 6 surgeons had very little experience with physical simulation, while the others had none. 10 participants had no experience in hybrid and virtual reality simulation, while the others had little experience.
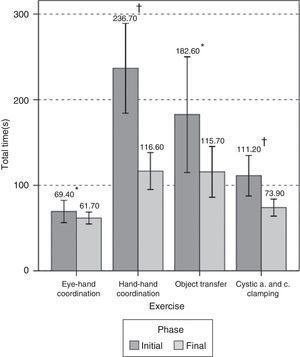
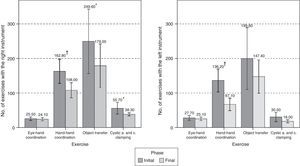
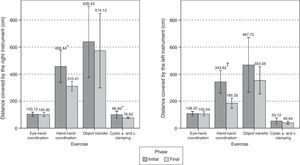
LAPMentor™ EvaluationAfter the course the surgeons carried out all of the LAPMentor™ exercises, with higher scores than the basal ones. They therefore performed the exercises more quickly (Fig. 1). The number of movements decreased significantly in exercises 2, 3 and 4 (Fig. 2), as did the distance covered in exercises 2 and 4 (Fig. 3). Speed of movement increased significantly in all of the exercises (Fig. 4).
The participants were significantly faster in the final repetition of the simulator exercises (8.39±4.55min vs 6.33±4.14min; P=.004) and Nissen's fundoplication (89.81±27.08min vs 63.29±17.38min; P=.005) and they increased their score on the OSATS scale (simulator: 18.99±1.27 vs 21.22±1.39; P=.001; Nissen's fundoplication: 17.8±1.48 vs 21.9±1.66; P=.004). Cronbach's alpha coefficient among the evaluators was 0.85.
Subjective Evaluation of the Training ElementsThe participants indicated that the duration of the course was appropriate (4.60±0.70), as a whole and in terms of the time for practice using the simulator (3.60±1.07) and the experimental model (4.70±0.48).
The highest-scoring question was “The utility of the suture exercise for learning skills” (4.90±0.32).
The other simulator exercises were not considered to be so positive, although in all cases they scored more than 3 points (Table 1). On the other hand, the lowest-scoring question was “The utility of virtual reality simulator evaluation”, which scored an average of 3.10±1.37. Nevertheless, an average score of 3.90±0.99 was awarded for “The utility of expert evaluation” and “The need for evaluation of the execution of the exercise”.
The surgeons considered the animal model to be more useful than the simulator. This was so for learning new techniques (4.70±0.67 vs 3.70±1.25) and for maintaining skill levels (4.60±1.26 vs 3.60±1.35). Moreover, the participants believe that they progressed more with training using the animal model (4.70±0.48) than they did with the physical simulator (3.70±1.34) (Table 1).
DiscussionThis study shows that the laparoscopic surgery training programme described is useful for general and digestive surgery residents’ learning and improving surgical skills. The participants also expressed a high level of satisfaction with the duration of the programme and its educational elements.
Our training model is based on a sequential learning system.11 The first level includes basic training in laparoscopic surgery and includes the physical simulation phase using the Simulap® (CCMIJU, Caceres, Spain) simulator, which was validated beforehand in terms of its appearance, content and construction.12 In this phase exercises were performed in order of increasing difficulty, thereby shortening the learning curve for more complex exercises such as sutures and also giving rise to substantial economic savings.13 We also believe that this gradual learning process using a simulator is necessary to achieve higher performance in the practical part using an animal model, so that usage of the latter can be reduced.
Of the practical exercises using the simulator, intracorporeal suture was considered to be the most useful exercise for the acquisition of skills. This may be influenced by the closer practical connection of this exercise with surgical techniques, as well as the higher degree of personal satisfaction stemming from learning a complex task that is highly useful in many surgical procedures.
In spite of the improvement in skills achieved by using simulation, animal models are the most realistic means of learning more demanding manoeuvres and more complete surgical procedures.14,15 The second level of our training programme is therefore dedicated to acquiring more advanced skills by practicing surgery on an experimental model. Throughout this phase of training the participants reduce the time taken for surgery while increasing the quality of their surgical technique.
In the subjective evaluation, the participants considered the animal model to be more useful than the simulator for learning new techniques and maintaining skills, and they believed they progressed more with this model. The participants also considered practice on an animal model to be very necessary before undertaking clinical laparoscopy (4.60±0.70) and they were strongly in agreement with the duration of training with the animal model (4.70±0.48). These results are similar to those obtained by Palter et al.,16 who stated that residents prefer the animal model to physical simulation, while placing virtual reality in last place.
The high level of acceptance by surgeons of animal models is probably due to the fact that they offer more realistic surgery than other synthetic or virtual models, thereby providing them with a more satisfactory experience. Nevertheless, on the basis of our experience, when a new surgeon attempts a procedure on an animal without the necessary basic skills, the training will probably prove frustrating and counterproductive.
While surgeons consider that it is necessary for their surgical skills to be evaluated, they expressed their preference for this to be carried out by an expert surgeon rather than a virtual simulator. Although virtual simulators have been shown to be useful as tools in the evaluation of skills,17 tutoring and evaluation by an expert surgeon seems to be the most acceptable option during training.
The objective evaluation tools selected in our study are the virtual reality simulator LAPMentor™, which has already proven the constructive validity of the exercises used in our study,17–20 and the overall evaluation scale OSATS,9 given that it is currently the most widely used and validated.7
The results obtained in the LAPMentor™ indicate that with the intensive training programme the participants become more efficient in their movements, by reducing the number of unnecessary movements and moving more quickly and automatically.
Sarker et al.21 evaluated the courses “Core skills in laparoscopic surgery” (CSLS) promoted by the Royal College of Surgeons, using the same virtual reality simulator and eye–hand and hand–hand exercises. In this case they only used physical simulation in a 17 hour course, and they did not evaluate the speed of movements. These authors obtained a higher number of significant differences in the eye–hand exercises than we did, although unlike our results, theirs did not include the distance covered by the left hand. The differences in the eye–hand coordination exercises may be due to the fact that this is a very basic exercise, and the small size of our sample.
To overcome this limitation we will try to increase this number in future courses to obtain more solid validation. Another aspect to be taken into account is the duration of the course. According to the results obtained, more studies are required to determine if the time dedicated to simulation could be reduced, as well as to define when the time and execution quality plateau is reached in the experimental model. i.e., the aim is to define an objective indicator that reliably and effectively indicates when a resident is ready to use a technique in clinical practice, at first under supervision, to determine the transfer of skills from the training programme to clinical practice in a hospital.
The digestive laparoscopic surgery model presented in this study has been proven to be valid for improving the basic and advanced skills of resident surgeons. Intracorporeal suture and the animal model were the highest scoring training elements.
Conflict of InterestsThe authors have no conflict of interests to declare.
The authors would like to thank the participants in this study for their readiness and help, as well as all of the CCMIJU staff involved.
Please cite this article as: Enciso S, Díaz-Güemes I, Usón J, Sánchez-Margallo FM. Validación de un modelo de formación intensivo en cirugía digestiva laparoscópica. Cir Esp. 2016;94:70–76.