Ischaemic heart disease is an important health problem. The characteristics of atherosclerotic plaques determine patient outcome. The aim of this study was to determine the histological grade of coronary atherosclerotic lesions in deceased patients after coronary artery bypass graft surgery, and to identify the complications of the severe plaques.
MethodA descriptive, cross-sectional, prospective study was carried out on 21 anatomical pieces of deceased patients over a period of 3 years. The epicardial coronary arteries were sectioned transversally every 1cm, and the odd numbered fragments and the regions of the anastomosis with the grafts were selected. They were embedded in paraffin, stained with haematoxylin-eosin, and the histological slides were studied using an Olympus BHM microscope.
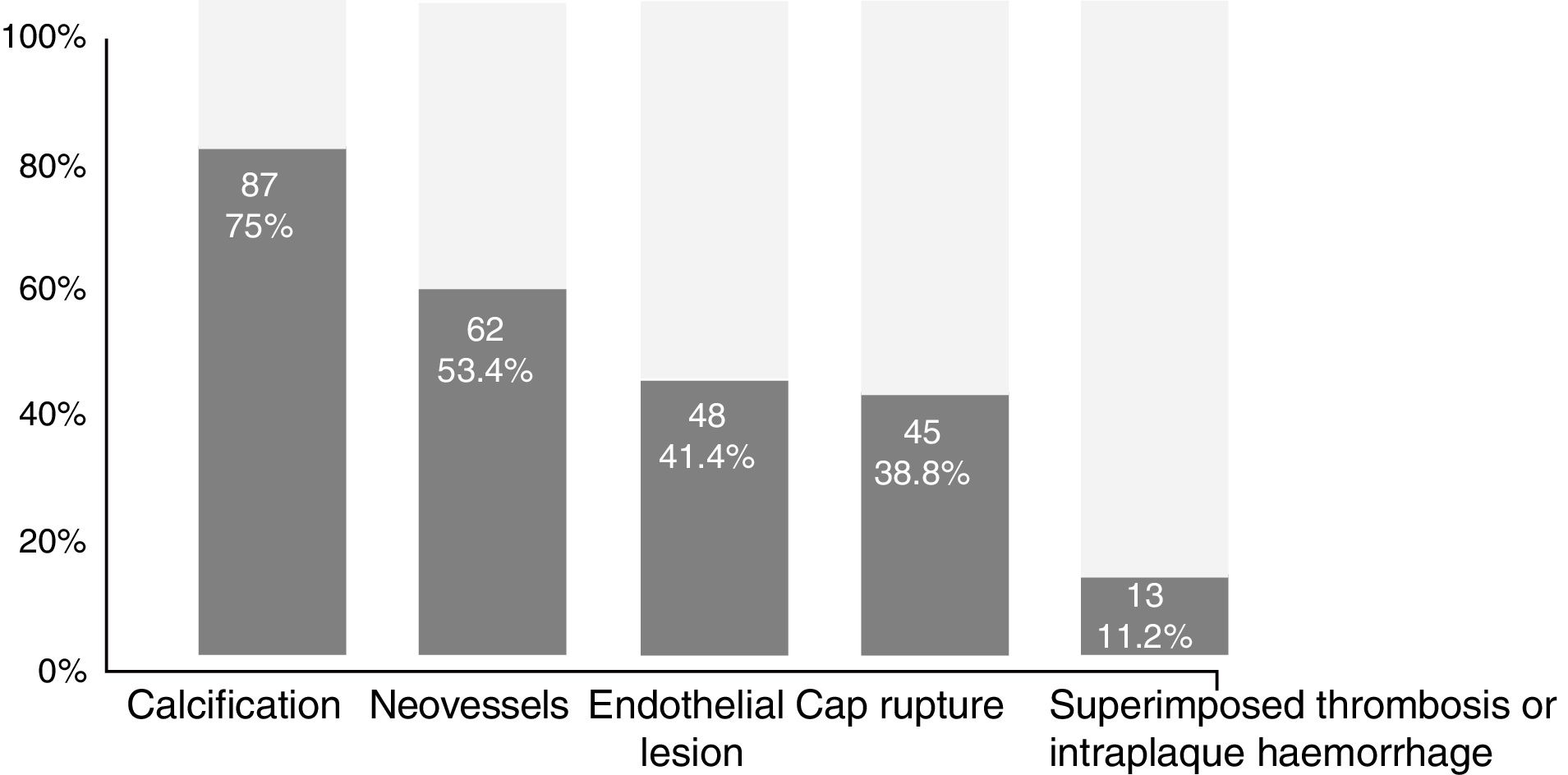
ResultsAn age over 50 years (85.7%), male gender (81.0%), and smoking (66.7%) predominated. Peri-operative infarction (38.1%) and cardiogenic shock (33.3%) were the main direct causes of death. The majority of the grafts were of venous origin (64.6%), and 149 lesions were detected, of which 116 (77.8%) were severe plaques, and 47.4% of them were located in the left anterior descending artery. The large majority (81.9%) of the lesions were located in the arterial segments proximal to the graft. A total of 255 histological complications were detected in the severe plaques, with 75.0% showing calcification. Hypertensive patients had more plaques with more complications, but no statistically significant association was found between these variables.
ConclusionsSevere plaques predominated, mostly located in the proximal segments of the coronary arteries, and the left anterior descending was the most affected artery. Calcification was the most observed complication in the severe plaques.
La cardiopatía isquémica constituye un importante problema de salud. Las características de las placas de ateroma condicionan la evolución de los pacientes. El objetivo fue determinar el grado histológico de las lesiones ateroscleróticas de las coronarias en fallecidos tras una revascularización miocárdica quirúrgica e identificar las complicaciones de las placas graves.
MétodosEstudio descriptivo, transversal, prospectivo, de 21 piezas anatómicas de fallecidos durante un período de 3 años. Las coronarias epicárdicas se seccionaron transversalmente cada 1cm y se seleccionaron los fragmentos impares y las regiones de la anastomosis con los injertos. Se incluyeron en parafina, se colorearon con hematoxilina-eosina y las láminas histológicas se describieron con un microscopio Olympus BHM.
ResultadosPredominaron la edad mayor de 50 años (85,7%), el sexo masculino (81,0%) y el tabaquismo (66,7%). El infarto perioperatorio (38,1%) y el shock cardiogénico (33,3%) fueron las principales causas directas de muerte. La mayoría de los injertos fueron venosos (64,6%). Se detectaron 149 lesiones: 116 (77,8%) fueron placas graves y el 47,4% de ellas se localizaban en la descendente anterior. El 81,9% de las lesiones se localizaron en los segmentos arteriales proximales al injerto. Se identificaron 255 complicaciones histológicas en las placas graves; el 75,0% presentó calcificación. Los hipertensos tenían más placas con más complicaciones, pero no se encontró relación estadística significativa entre estas variables.
ConclusionesPredominaron las placas graves, localizadas mayoritariamente en los segmentos proximales de las coronarias, y la descendente anterior fue la más afectada. La calcificación fue la complicación más observada en las placas graves.
Cardiovascular diseases are a major health problem in developed countries.1 In Latin America and Cuba, they are the leading cause of death.2,3 Coronary artery disease due to atherosclerosis is also a major cause of death and one of the leading causes of occupational disability, with subsequent impacts on the economy and the quality of life of these patients.4
These diseases accounted for more than a quarter of all deaths worldwide in 2000 and this figure is expected to increase by 2050.2
Coronary arteries, under the influence of risk factors, are affected by specific pathological processes—such as atherosclerosis—which damage the intima and other layers of the arterial wall, causing myocardial ischaemia.4,5 Some patients with acute coronary syndrome die within the first few hours of the onset of symptoms, with about 10% dying within the first few weeks. Those who survive, which is now the majority of patients thanks to advances in therapy, have a lower life expectancy and are five times more likely to die within the subsequent five years than those without a history of heart disease.4
Atherosclerosis is currently considered a global health problem, but the condition is as old as man himself because there are descriptions of atheroscleroic plaque in Egyptian mummies dating back to 500 years BC. In this sense, it is worth mentioning that, despite scientific and technical advances, the interest shown by the professionals involved and the vast economic resources allocated for the study of this disease, the clinical and pathological manifestations and pathomorphological characteristics of the disease have always remained the same.6,7
Regardless of the development of innovative techniques and methods, which have helped perfect the study of atherosclerosis over recent decades, there is still much to be done and more research is required to gain a better understanding of the disease. Therefore, the objective of this research is to study issues that have not yet been explored in much detail, i.e. histological characterisation of atherosclerotic lesions from coronary arteries of deceased patients after coronary artery bypass graft surgery, identification of plaque features that define such lesions as severe, and determination of their relationship with clinical variables.
MethodA descriptive, cross-sectional, prospective study was conducted using post-mortem specimens from coronary arteries obtained from 21 patients who had died after coronary artery bypass graft surgery at Cardiocentro Ernesto Che Guevara de Santa Clara (Cuba) over three years.
Inclusion and exclusion criteriaDuring the assessment period, 56 patients had heart surgery and died due to any cause after the heart surgery. This research only included those who had undergone coronary artery bypass graft surgery. Good histological slide quality was also an essential criterion for this research, which is why it was not necessary to exclude anyone from the study sample.
Primary data collectionOnce the post-mortem protocol had been studied, the clinical records were then reviewed and a data collection form was prepared (Appendix 1, supplementary material).
Demographic variables (age, gender and skin colour), clinical and surgical variables (risk factors, medical history, clinical diagnosis, type and number of coronary artery bypass grafts) and variables relating to the angiogram results were obtained from the clinical records.
Ante-mortem diagnoses were extracted from the clinical records and post-mortem protocols and were placed in chronological order, stating the basic and direct causes of death.
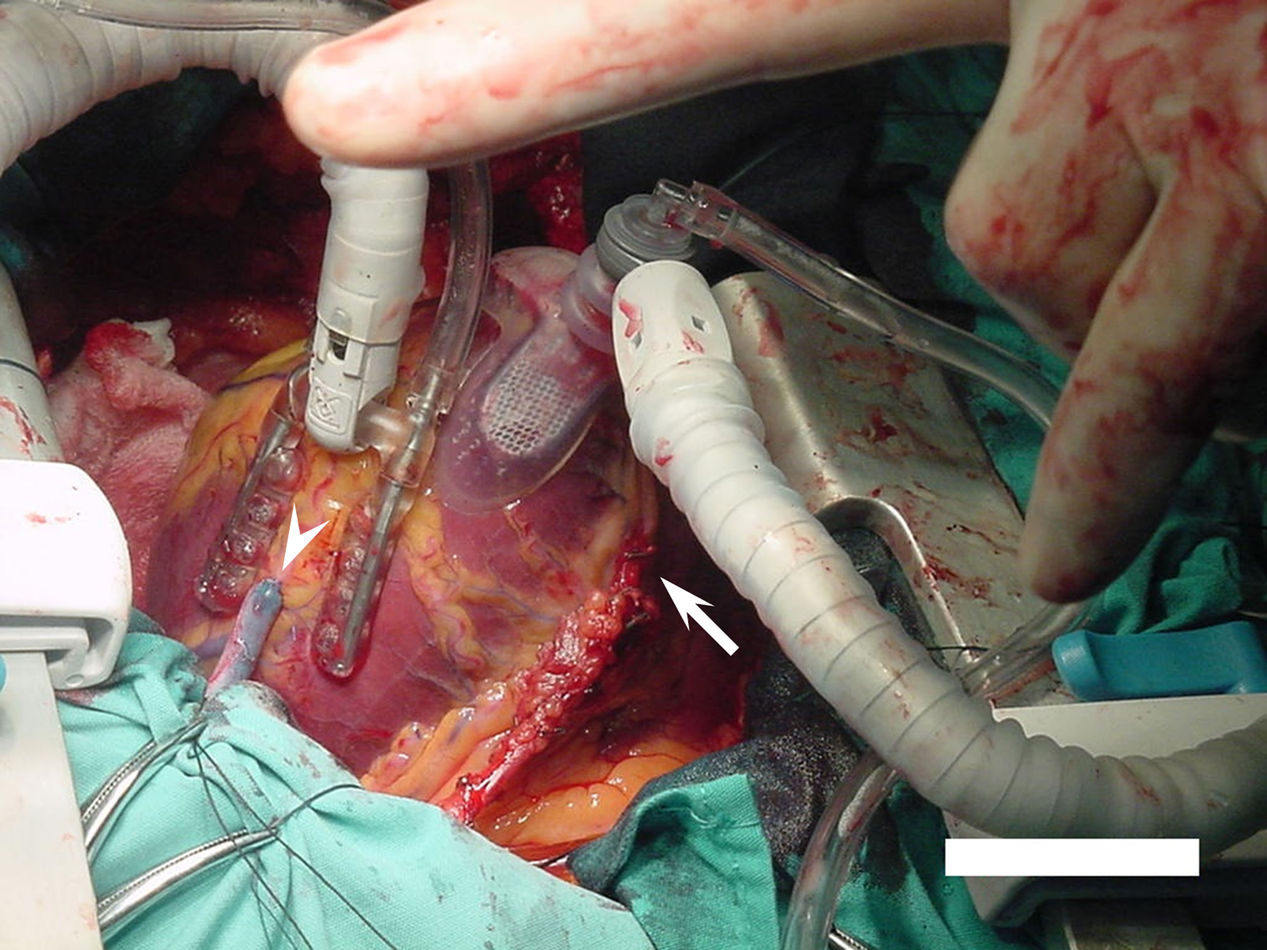
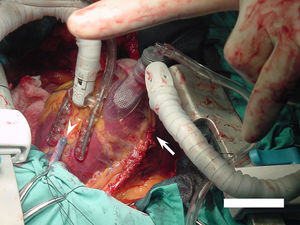
Processing of anatomical partsDuring each post-mortem, the heart was separated from the rest of the organs, the pericardium was opened and the aorta and pulmonary arteries were sectioned 2cm above the graft anastomoses and valve, respectively, and the vena cava and pulmonary veins were sectioned at the point where they enter the atria. Once the heart had been separated, the coronary arteries were dissected and extracted with minimal epicardial fat and the bypass grafts, all of which was fixed in 10% formalin for 24h.
Processing of coronary arteries and graftsThe 48 coronary arteries in which a graft had been implanted were measured longitudinally from the distal-most part to the ostium in the corresponding aortic sinus. They were then sectioned transversely in the same order and direction, making cuts every 1cm for the macroscopic examination, taking care not to disturb the graft-to-artery anastomoses. This resulted in 242 arterial segments that were processed for study.
Macroscopic analysisOdd-numbered sections were selected so that each coronary artery was described starting from the distal-most fragment. The graft and the technique used for grafting the vessel to the corresponding coronary artery was also described along with the type of anastomosis (arterio-venous or arterio-arterial). The coronary artery-bridge location, whether in an even- or odd-numbered section, was always respected, which was used as a reference to delimit the proximal and distal portions of each artery in relation to the graft. If any atherosclerotic lesion was observed, its location was specified and its size was described along with the subjective presence or absence of calcium and the percent occlusion of the vascular lumen. To determine the latter, the cross-section virtually divided into four parts was evaluated and the result of the observation was expressed as a percentage (%) in order to qualitatively define the occlusion as mild, moderate or severe based on the observer's criteria in accordance with the joint recommendations of the American College of Cardiology and the American Heart Association.8
Microscopic analysisSlide preparation and microscopic interpretationA histological study was performed on each section subjected to macroscopic analysis. For this purpose, they were labelled with the vessel name and code number according to section level. A decalcification process (less than 24h) was then carried out before they were processed using the paraffin embedding technique. The blocks were prepared by placing the specimen in such a way that any cuts made would pass through the entire thickness of the vessels. A vertical microtome was used to cut serial sections, with an average thickness of 5μm. Haematoxylin and eosin (H&E) staining was used to prepare 290 histological slides, which were analysed using an Olympus BHM microscope.
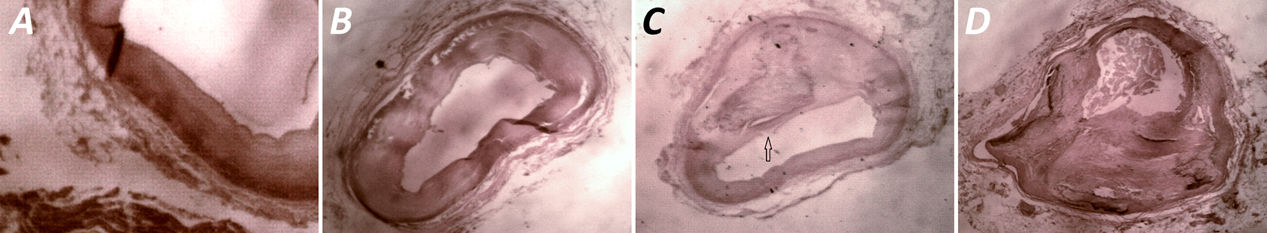
A 10× lens was used to obtain panoramic information of the section, specifying the presence of the entire blood vessel and, in the case of the graft site, the presence of both graft portions (coronary artery and graft). Vascular permeability was determined using a 20× lens and, in the event of occlusion, the most likely aetiology was specified. Occlusion due to atherosclerotic plaque on the wall was defined using the same method and classification used for macroscopic observation. A 40× lens was then used for the descriptive study of the wall of the vessel affected by the atherosclerotic lesion. The descriptive study included tissue details defining the lesion as fatty streak, fibrous plaque and severe plaque (Supplementary Fig. 1) according to the classification of the American Heart Association.9
VariablesAtherogenic risk factors: classic factors that have a positive interdependence (cause–effect) relationship with the disease: hyperlipidaemia, diabetes mellitus, hypertension, smoking and obesity.7
Direct cause of death: disease or pathological condition that directly caused death.10,11
Basic cause of death: disease that started the process resulting in the patient's death.10,11
Fatty streak: grade I atherosclerotic lesion, initial lesion or band of fat. It consists of cells containing fat-filled vacuoles known as foam cells, lipophages or atherocytes. It seldom protrudes into the arterial lumen and, if it does, this is only very slightly so blood flow is not modified.1,6,9
Fibrous plaque: grade II atherosclerotic lesion where the central core of extracellular lipids—with cholesterol crystals and abundant foam cells—is usually surrounded by a collagenised and hyalinised fibrous cap that gives this lesion its name. It contributes to narrowing of the arterial lumen.1,6,9
Severe plaque: grade III atherosclerotic lesion. This is a fibrous plaque that has undergone one or more of the following modifications (complications): (a) injury to the endothelium; (b) weakening or rupture of the fibrous cap with early thrombus formation; (c) presence of platelet groups aggregated and adhered to the endothelium that starts thrombus formation or established thrombosis in the arterial wall; (d) neovascularisation; (e) intraplaque haemorrhage; or (f) calcium deposits in the arterial intima and media.1,6,9
Portion proximal/distal to the graft: segment of coronary artery before/after the graft placement site.
Mild, moderate and severe occlusion due to atherosclerotic plaque: when the lesion affects less than 50%, between 50% and 75%, and more than 75% of the vascular lumen, respectively.8
Data processingAll data collected was processed using the SPSS statistics software, version 15 for Windows. A descriptive analysis of the variables (number and percentage) was performed and the Monte Carlo significance test associated with the Fisher's exact test was applied to determine ratios.
Ethical considerationsThis paper was approved by the Research Ethics Committee of Cardiocentro Ernesto Che Guevara and the Universidad de Ciencias Médicas de Villa Clara [University of Medical Sciences of Villa Clara] (Cuba).
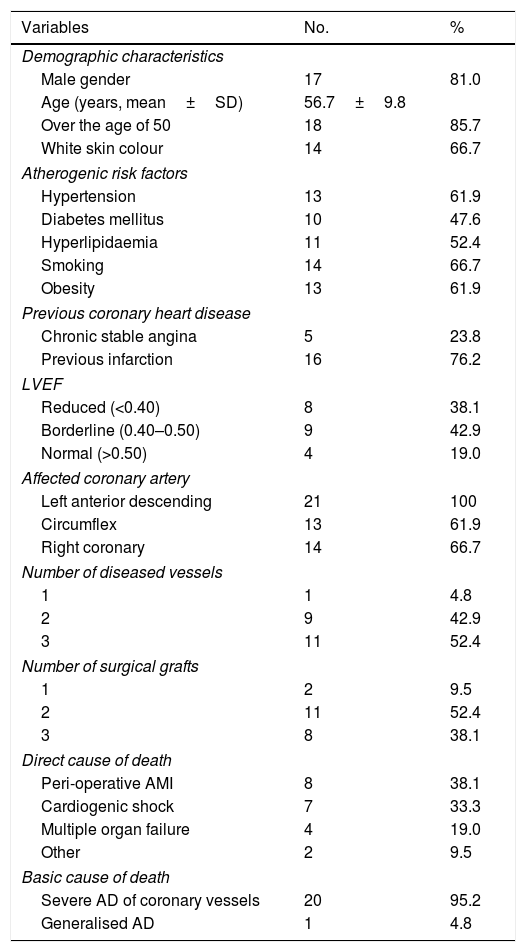
ResultsThe demographic and clinical characteristics and the causes of death of the 21 patients studied are shown in Table 1, where it can be observed that male gender (81.0%), age over 50 years (85.7%) and white skin (66.7%) predominated. Smoking was the most common atherogenic risk factor (66.7%), three-quarters of the deceased patients suffered a previous myocardial infarction and only one in five patients had a normal left ventricular ejection fraction. The left anterior descending artery was most commonly affected in all patients, 52.4% had triple-vessel coronary artery disease and the same percentage received two grafts. Peri-operative infarction and cardiogenic shock combined accounted for 71.4% of the direct causes of death. Severe neurological dysfunction and acute respiratory failure were classified as “other”.
Demographic and clinical characteristics and causes of death in study patients (n=21).
| Variables | No. | % |
|---|---|---|
| Demographic characteristics | ||
| Male gender | 17 | 81.0 |
| Age (years, mean±SD) | 56.7±9.8 | |
| Over the age of 50 | 18 | 85.7 |
| White skin colour | 14 | 66.7 |
| Atherogenic risk factors | ||
| Hypertension | 13 | 61.9 |
| Diabetes mellitus | 10 | 47.6 |
| Hyperlipidaemia | 11 | 52.4 |
| Smoking | 14 | 66.7 |
| Obesity | 13 | 61.9 |
| Previous coronary heart disease | ||
| Chronic stable angina | 5 | 23.8 |
| Previous infarction | 16 | 76.2 |
| LVEF | ||
| Reduced (<0.40) | 8 | 38.1 |
| Borderline (0.40–0.50) | 9 | 42.9 |
| Normal (>0.50) | 4 | 19.0 |
| Affected coronary artery | ||
| Left anterior descending | 21 | 100 |
| Circumflex | 13 | 61.9 |
| Right coronary | 14 | 66.7 |
| Number of diseased vessels | ||
| 1 | 1 | 4.8 |
| 2 | 9 | 42.9 |
| 3 | 11 | 52.4 |
| Number of surgical grafts | ||
| 1 | 2 | 9.5 |
| 2 | 11 | 52.4 |
| 3 | 8 | 38.1 |
| Direct cause of death | ||
| Peri-operative AMI | 8 | 38.1 |
| Cardiogenic shock | 7 | 33.3 |
| Multiple organ failure | 4 | 19.0 |
| Other | 2 | 9.5 |
| Basic cause of death | ||
| Severe AD of coronary vessels | 20 | 95.2 |
| Generalised AD | 1 | 4.8 |
AD: atherosclerotic disease; AMI: acute myocardial infarction; LVEF: left ventricular ejection fraction.
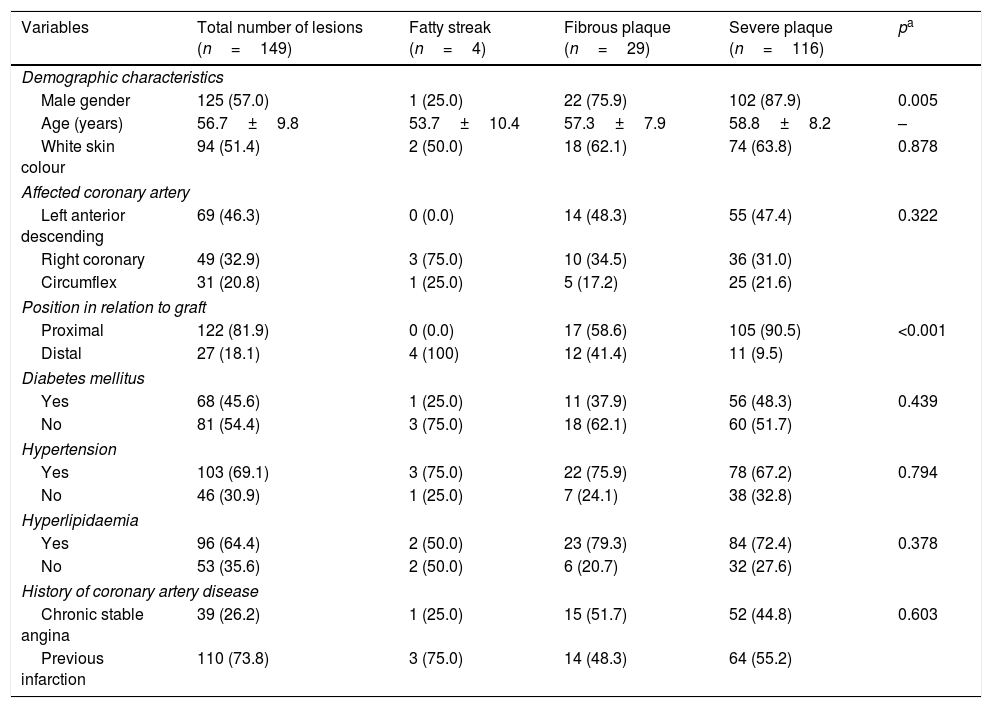
As expected in deceased patients, severe plaque predominated, accounting for 77.8% of the 149 atherosclerotic lesions found in all coronary arteries studied (Table 2). Severe plaque was also more common, with a statistically significant difference, among men (87.9%; p=0.005) and in the arterial segment prior to the graft (90.5%; p<0.001). However, no statistical relationship was found with regard to skin colour (p=0.878), the affected coronary artery (p=0.322), the presence of risk factors such as hypertension (p=0.794), diabetes mellitus (p=0.439) or hyperlipidaemia (p=0.378), or a history of any form of coronary heart disease (stable angina or previous infarction, p=0.603).
Characteristics of the atherosclerotic lesion in relation to anatomical and clinical variables.
| Variables | Total number of lesions (n=149) | Fatty streak (n=4) | Fibrous plaque (n=29) | Severe plaque (n=116) | pa |
|---|---|---|---|---|---|
| Demographic characteristics | |||||
| Male gender | 125 (57.0) | 1 (25.0) | 22 (75.9) | 102 (87.9) | 0.005 |
| Age (years) | 56.7±9.8 | 53.7±10.4 | 57.3±7.9 | 58.8±8.2 | – |
| White skin colour | 94 (51.4) | 2 (50.0) | 18 (62.1) | 74 (63.8) | 0.878 |
| Affected coronary artery | |||||
| Left anterior descending | 69 (46.3) | 0 (0.0) | 14 (48.3) | 55 (47.4) | 0.322 |
| Right coronary | 49 (32.9) | 3 (75.0) | 10 (34.5) | 36 (31.0) | |
| Circumflex | 31 (20.8) | 1 (25.0) | 5 (17.2) | 25 (21.6) | |
| Position in relation to graft | |||||
| Proximal | 122 (81.9) | 0 (0.0) | 17 (58.6) | 105 (90.5) | <0.001 |
| Distal | 27 (18.1) | 4 (100) | 12 (41.4) | 11 (9.5) | |
| Diabetes mellitus | |||||
| Yes | 68 (45.6) | 1 (25.0) | 11 (37.9) | 56 (48.3) | 0.439 |
| No | 81 (54.4) | 3 (75.0) | 18 (62.1) | 60 (51.7) | |
| Hypertension | |||||
| Yes | 103 (69.1) | 3 (75.0) | 22 (75.9) | 78 (67.2) | 0.794 |
| No | 46 (30.9) | 1 (25.0) | 7 (24.1) | 38 (32.8) | |
| Hyperlipidaemia | |||||
| Yes | 96 (64.4) | 2 (50.0) | 23 (79.3) | 84 (72.4) | 0.378 |
| No | 53 (35.6) | 2 (50.0) | 6 (20.7) | 32 (27.6) | |
| History of coronary artery disease | |||||
| Chronic stable angina | 39 (26.2) | 1 (25.0) | 15 (51.7) | 52 (44.8) | 0.603 |
| Previous infarction | 110 (73.8) | 3 (75.0) | 14 (48.3) | 64 (55.2) | |
Data expressed as n (%) or mean±standard deviation.
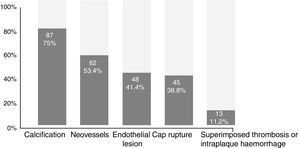
Fig. 1 shows the distribution of the 255 complications found in the 116 cases of severe plaque, where the presence of calcium (75.0%) and neovascularisation (53.4%) predominated.
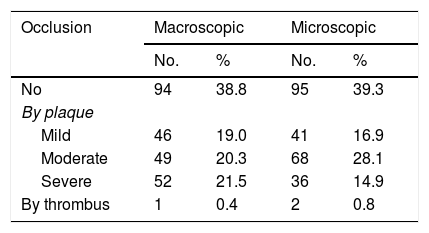
The permeability behaviour of the 242 arterial segments from the native vessels studied is shown in Table 3, which shows there is little variation between the macroscopic and microscopic observation methods when vessel occlusion is mild or absent. However, differences are more evident when occlusion is more serious (moderate and severe), with no statistically significant differences (p>0.05) found.
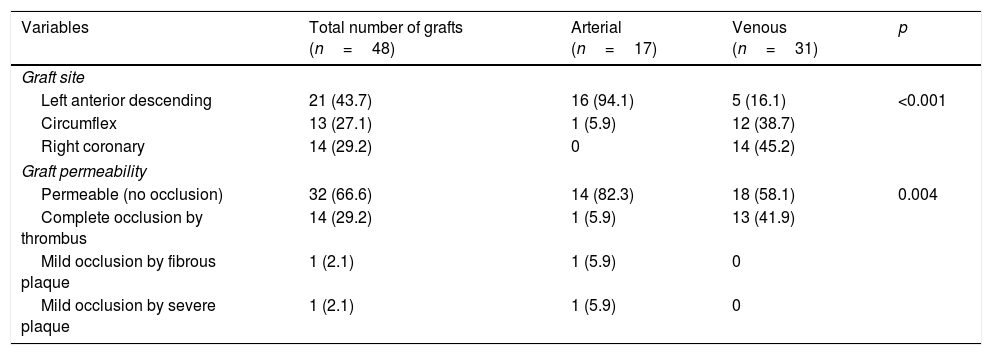
All three coronary arteries were affected and received grafts. Venous grafts predominated (64.6%), but the use of arterial grafts was significantly higher in the left anterior descending artery (94.1%; p<0.001), although it is important to note that 16.1% of venous grafts were grafted into this major artery (Table 4). A statistically significant relationship (p=0.004) was also found between the type of graft and its permeability since 41.9% of venous grafts were completely blocked by thrombi. Contrary to what might be expected, since this was a study involving deceased patients, two-thirds of the grafts were permeable and only one of the arterial grafts (5.9%) had thrombi.
Graft-related variables.
| Variables | Total number of grafts (n=48) | Arterial (n=17) | Venous (n=31) | p |
|---|---|---|---|---|
| Graft site | ||||
| Left anterior descending | 21 (43.7) | 16 (94.1) | 5 (16.1) | <0.001 |
| Circumflex | 13 (27.1) | 1 (5.9) | 12 (38.7) | |
| Right coronary | 14 (29.2) | 0 | 14 (45.2) | |
| Graft permeability | ||||
| Permeable (no occlusion) | 32 (66.6) | 14 (82.3) | 18 (58.1) | 0.004 |
| Complete occlusion by thrombus | 14 (29.2) | 1 (5.9) | 13 (41.9) | |
| Mild occlusion by fibrous plaque | 1 (2.1) | 1 (5.9) | 0 | |
| Mild occlusion by severe plaque | 1 (2.1) | 1 (5.9) | 0 | |
Data are expressed as n (%).
Coronary artery bypass graft surgery has, for many decades, been one of the main pillars of treatment for patients with severe coronary artery disease as it improves survival, symptoms and quality of life, but it is not free from complications and the risk of death. Some such complications (peri-operative infarction, cardiogenic shock and multiple organ failure) were found during this investigation, which coincides with reports by other authors regarding the most common causes of death in this subgroup of patients.12–14
Generalised or localised atherosclerosis in the most common and dangerous regions (coronary arteries, cerebral arteries or aorta and their distal branches) is the disease that has been most commonly reported as the trigger of the process leading to the patient's death (basic cause).15,16 This has also been shown in various international studies and other studies conducted in Cuba, based on the Sistema Automatizado de Registro y Control de Anatomía Patológica (Automated Anatomical Pathology Registry and Control System – SARCAP, Cuba).16–18
In our study, severe atherosclerotic disease of the coronary arteries was the predominant basic cause, which is to be expected for this specific subgroup of patients. This result agrees with reports by the National Statistics Office of the Ministry of Public Health of Cuba3,10 and with papers published in other countries.13,14,19,20
Both types of autologous grafts (arterial and venous) are used in coronary artery bypass graft surgery.21,22 However, unlike the results found during our research, the use of several arterial grafts is preferred, not only from the left internal mammary artery but also from the right internal mammary, radial and gastroepiploic arteries.21–25
Almost two-thirds of the grafts in the sample studied were venous grafts, and with regards to arterial grafts, only the left internal mammary artery was used (Supplementary Fig. 2). This, together with the placement of saphenous vein grafts in the left anterior descending artery in five patients, may have affected the patients’ unfavourable outcome.
There is no doubt that the choice of graft (arterial or venous) affects survival.26 Spasm causes peri-operative infarction, but is easier to diagnose during electrical and haemodynamic monitoring. Complete occlusion by thrombi, which is more likely in deceased patients, was found in 29.2% of all grafts and in 41.9% of the venous grafts in this study.
Thrombotic occlusion is the main cause of early saphenous vein graft failure (first month after surgery),21,27 which coincides with our results, since the individuals studied died during that period and the main cause of graft occlusion was precisely the presence of thrombosis in the saphenous vein graft.
Histological aspects and complicationsSevere plaque is the evolutionary biological continuity of fibrous plaque progression. The incidence of risk factors in the progression and severity of the atherosclerotic process is known, which is why we believe that the coexistence of several risk factors in individuals from the study sample determined the predominance of the advanced atherosclerotic lesion and the low presentation rate of the initial lesion: fatty streak. The majority of patients were over the age of 50, and the older they were, the more the disease had progressed and the longer they had been exposed to risk factors and inadequate lifestyles, which explains why the morphological transformation process of the lesions occurred with sufficient intensity. This coincides with the findings of other studies, in which the predominance of fibrous and severe plaque has been observed in elderly individuals.1,2,6,20,28
The most important coronary artery is the left anterior descending artery.29 Several studies, like our own, have found that this is the artery most affected by atherosclerosis and in which severe plaque is more common.20,30–32 However, due to the small size of our sample, we found no statistical significance because only 14 of the 29 fibrous plaques and 55 of the 116 severe plaques were detected in this artery.
Vyas et al.33 found that, in 113 post-mortems performed on patients who had died from non-cardiac causes, 83 (73.45%) showed evidence of atherosclerosis, 82% were men, the most commonly affected artery was the left anterior descending artery (69%) and 22% had triple-vessel coronary artery disease.
The distribution of atherosclerotic plaques in human arteries has been widely studied. In the case of the coronary arteries, it is known that the most affected area is the origin, especially the first 6cm, approximately, which include the proximal and middle segments. Therefore, most grafts are placed distal to these regions during surgery and, moreover, the “relationship with the graft” defined in this research means that most severe plaques are in the proximal region.
The results of our study confirm the findings of other studies in the literature, which suggest that coronary lesions are predominantly found in the proximal and mid portions and are more common in the left anterior descending artery. More distal lesions, although less common, limit the surgical result and are one of the causes of failure within the first few months of surgery due to being distal to the graft placement site.28,29
Coronary artery disease follows a slow and gradual process, but its progression is also based on the onset of acute changes in plaque geometry. Severe atherosclerotic lesions are the most dangerous and are due to the effect of aggravating factors (endothelial dysfunction, haemodynamic changes, inflammation and thrombosis), which alter the histological structure of the fibrous plaques, making them unstable and triggering reduced coronary blood flow and the clinical expression of myocardial ischaemia.28,34,35
Atherosclerosis is the only known vascular disease associated with coronary calcification. This is based on the fact that, in 1912, Faber noticed that Mönckeberg medial calcific sclerosis did not occur in these arteries.1,36 Many studies highlight the presence of calcium as one of the most common complications of advanced atherosclerosis, which is a sign of disease progression and severity. This is why it was considered an important criterion in the 1957 classification established by the WHO and updated by the American Heart Association.9 Many studies agree on the high presence of calcification in advanced atherosclerotic lesions. Some, like our own, address the subject from a histopathological point of view, while others use computed tomography.31,37,38 In this sense, von Kossa staining would have been useful for analysing the calcium deposit and, consequently, the degree of plaque stability. However, paradoxically, this stability is not necessarily proportional to the degree of coronary artery occlusion. In fact, some investigations based on the Multi-Ethnic Study of Atherosclerosis (MESA)39,40 have shown differences between calcification volume and density in vulnerable plaques since these factors are respectively associated, directly and inversely, with cardiovascular risk and the incidence of acute coronary events. Meanwhile, Motoyama et al.41 state that the tomographic characteristics of plaque calcification responsible for acute coronary syndromes, i.e. their morphology, is irregular or patchy.
The properties of the vascular endothelium and endothelial dysfunction are well established and key to the formation of new blood vessels in advanced atherosclerotic plaques. There are studies that agree with ours regarding the existence of neovessels around the lipid core, but such vessels also occur in the medial layer and at the border between the medial and intimal layers.20,42
Atherosclerotic plaque is subject to the action of a combination of factors that induce its rupture. Lesions that tend to rupture have a markedly eccentric configuration. Fissures frequently occur at the point where the fibrous cap joins the adjacent normal arterial wall, a site associated with high circumferential stress. Similar to our study, several authors have reported plaque complications.34,42,43 The most feared is superimposed thrombosis, which was found in 11.2% of this sample, in which all the possible lesions that give atherosclerotic plaques their severity characteristics were also found.34,35,42,43
Macroscopic/microscopic correlationThe majority of studies in patients who have undergone coronary artery bypass graft surgery are in line with ours in terms of low presence of thrombosis in the native artery. Previously, thrombi were usually documented from a morphological point of view. However, today, in the age of thrombolysis, they are much less evident.34,35,43,44 Furthermore, since the patients underwent elective coronary artery bypass graft surgery, we were unlikely to find many cases of this type of thrombosis since this plaque complication gives rise to acute symptoms.
In accordance with the existing literature, the atherosclerotic plaques studied had luminal narrowing repercussions, producing different degrees of occlusion, and the presence of superimposed thrombi was also reported, which produced partial blockages.35,45–47
The usefulness of clinical post-mortems is unquestionable due to all the benefits they bring to medicine and, especially, to mortality analyses. In fact, many doctors consider it to be “the final consultation”.16 However, to complete studies carried out with the naked eye (macroscopic), the use of microscopy is unavoidable. In our study, the results obtained by qualitative macroscopic visualisation were fairly close to the microscopic results. Unfortunately, we did not find similar studies that had focused on investigating how close macroscopic and microscopic observations of the coronary arteries of these patients actually are.
Risk factors and clinical implicationsAtherosclerosis is a disease that begins early in life, but is more prevalent in elderly patients since its clinical manifestations rarely appear before the fourth decade of life.5,6 It is a silent, latent and chronic inflammatory process—which is usually ignored by the patient—affected by lifestyle. Over time, initial lesions can become much more serious, causing changes in blood flow with subsequent clinical manifestations affecting the target organs.48–50
Men have a greater relative risk of atherosclerotic disease than women,12,33,48,51,52 and it has been suggested that female oestrogens may have a beneficial effect in this regard. However, in our investigation, the statistically significant relationship of this variable with the presence of severe plaque should not be taken into consideration due to the clear predominance of the male gender (17/21).
No statistically significant relationship was found in this investigation between diabetes mellitus, hypertension and hyperlipidaemia and the presence of severe plaque, which is explained by the small sample size and the similar severity of coronary heart disease in the patients studied, since the association between these classic risk factors and atherosclerosis is well known. However, this underlines, once again, the need for further studies of atherosclerosis because patients with rare and sometimes unique risk factors who develop acute coronary syndromes, and others with several risk factors who do not develop such syndromes, are found every day in clinical practice.
In the early 20th century, a group of English investigators decided to study the bodies of Egyptian mummies that were over 2000 years old. They analysed aortas, coronary arteries, iliac arteries and other arteries and concluded that the disease has not undergone any morphological changes since these early years in the history of man.1,4,6
So what have we achieved? Moreno53 stated in the first issue of the bicentennial series of The New England Journal of Medicine that there is an article on coronary artery disease,54 which could have been conditioned by the fact that, over the past 200 years, cardiovascular disease, especially coronary artery disease, continues to be the leading cause of death in developed countries, despite technological advances and pharmaceutical industry developments. Are patients who do not adhere to treatment and the necessary changes in lifestyle very undisciplined, or have we not yet managed to find “the key” to predicting and preventing atherothrombotic risk and its clinical manifestations?
Carro7 states that patients with coronary artery disease not only have a high prevalence of risk factors, but their control is very poor, and that only emphasising the importance of controlling such risk factors in secondary prevention implies the consideration that arriving “too late” is fine.
We can therefore state that more research is required to further the study of atherosclerosis as a causative agent in order to change the course of a disease that we have not been able to modify for more than 2000 years. Impressive diagnostic and therapeutic advances, percutaneous coronary intervention, heart surgery and plaque-stabilising agents cannot be our goal. We must not settle for having changed the consequences of this disease, which is what we have managed to do so far, because atherosclerosis affects the entire vascular endothelium, also causing cerebrovascular, renal and other peripheral artery diseases, which could improve and even disappear—despite the hyperbole—if the formation and development of atherosclerotic plaques is reduced, controlled or eliminated.
ConclusionsThis paper addresses an issue that has been explored very little, i.e. the histological characterisation of atherosclerotic plaques obtained from coronary arteries of deceased patients after coronary artery bypass graft surgery, in which severe plaques located primarily in the proximal segments of coronary arteries, before the graft placement site, and in men, predominated. The left anterior descending artery was the most commonly affected artery by the atherosclerotic process. Calcification and neovascularisation were the most commonly observed complications in severe plaques.
FundingNone.
Conflicts of interestNone.
Please cite this article as: Pérez Sorí Y, Herrera Moya VA, Puig Reyes I, Moreno-Martínez FL, Bermúdez Alemán R, Rodríguez Millares T, et al. Histología de la placa de ateroma en arterias coronarias de fallecidos después de una revascularización miocárdica quirúrgica. Clin Investig Arterioscler. 2019;31:63–72.