Chronic inflammation plays a considerable role in atherosclerosis and may occur simultaneously in different arteries. This condition is referred to as multisite arterial disease (MSAD). We aimed to investigate the association between inflammatory markers and MSAD.
MethodsIn this cross-sectional study we included 526 patients with peripheral artery disease (PAD). Patients with PAD were evaluated by conventional or computed tomography angiography for the presence of coronary artery disease (CAD) and those with at least 30% stenosis were included in the study. Patients were divided into two groups: either MSAD+(PAD and CAD), Group 1) or MSAD- (only PAD without CAD, Group 2). Inflammatory markers were compared between the two groups.
ResultsAmong all patients, 293 had MSAD while 233 had only PAD. The MSAD+group had higher neutrophil-to-lymphocyte ratio (NLR) and platelet-to-neutrophil ratio (PLR) (5.08±0.19, 4.67±0.51, and 207.1±6.23, 169.3±10.8, respectively, p<0.001). In multivariate analysis, HT [odds ratio (OR): 2.40 (1.61-3.59)); p<0.002], male gender [OR: 2.03 (1.29-3.17); p=0.002], DM [OR:1.56 (1.03-2.36); P=0.035], NLR [OR: 1,08 (1.02-1.16); p=0.021, and PLR [OR:1.05 (1.03-1.08); p<0.001] were found to be associated with MSAD.
ConclusionNLR and PLR are correlated with MSAD and may indicate the extent of atherosclerosis.
La inflamación crónica juega un papel importante en la aterosclerosis, pudiendo producirse de manera simultánea en diferentes arterias. Esta condición se define como enfermedad arterial de múltiples vasos (MSAD). Nuestro objetivo fue estudiar la asociación entre los marcadores inflamatorios y MSAD.
MétodosEn este estudio transversal incluimos 526 pacientes con enfermedad arterial periférica (EAP), quienes fueron evaluados mediante angiografía convencional o angiografía por tomografía computarizada para cribar la presencia de enfermedad de las arterias coronarias (EAC), incluyéndose en el estudio a aquellos pacientes con un 30% mínimo de estenosis. Se dividió a los pacientes en dos grupos: Grupo 1: MSAD+(EAP y EAC); Grupo 2: MSAD-(sólo EAP sin EAC). Se compararon los marcadores inflamatorios entre los dos grupos.
ResultadosDe entre todos los pacientes, 293 tenían MSAD, mientras que 233 tenían solo EAP. El Grupo MSAD+tenía mayor índice neutrófilos/linfocitos (INL) e índice plaquetas/neutrófilos (IPN) (5,08±0,19; 4,67±0,51; y 207,1±6,23; 169,3±10,8, respectivamente, p<0,001). En el análisis multivariante se encontró que HT (odds ratio [OR]: 2,40 [1,61-3,59]; p<0,002), sexo masculino (OR: 2,03 [1,29-3,17]; p=0,002), DM (OR:1,56 [1,03-2,36]; p=0,035), INL (OR: 1,08 [1,02-1,16]; p=0,021), e IPL (OR:1,05 [1,03-1,08]; p<0,001) estaban asociados a MSAD.
ConclusiónINL e IPN están correlacionados con MSAD, lo cual puede ser indicativo del alcance de la aterosclerosis.
Atherosclerotic cardiovascular disease (CVD) is the leading cause of death worldwide. Atherosclerosis is a multisystemic chronic inflammatory disease of large and medium-sized arteries that causes coronary artery disease (CAD), stroke, and peripheral arterial disease (PAD).1 When atherosclerosis is present in at least two major vascular territories it is defined as multisite artery disease (MSAD). MSAD is common when atherosclerotic involvement is detected in one vascular territory, ranging from 10 to 15% of patients with CAD to 60 to 70% of patients with severe carotid stenosis or lower extremity artery disease (LEAD). MSAD is invariably associated with worse clinical outcomes.2
The hallmark hypothesis of atherosclerosis is lipoprotein aggregation. However, clinical and experimental data suggest that inflammation plays an important role in atherothrombosis, regardless of cholesterol level.3 New inflammatory markers have been identified in recent years and an association has been found with many CVD.2,4 The neutrophil-to-lymphocyte ratio (NLR), monocyte-to-HDL ratio (MHR), lymphocyte-to-monocyte ratio (LMR), platelet-to-lymphocyte ratio (PLR), plasma atherogenic index (PAI), and cardiac risk ratio (CRR) can also be indicators of systemic inflammation and atherosclerosis. These parameters not only are relevant but also predict the risk of atherosclerotic CVD.5,6 Therefore, they are deemed to have a direct relationship with atherosclerotic burden. Nevertheless, the role of inflammatory markers in MSAD is not clearly known. In this study, we aimed to evaluate the association between inflammatory markers and MSAD in patients with PAD.
MethodsIn this cross-sectional study, we included 526 patients diagnosed with lower and upper extremity, and carotid arterial disease between January 2010 - January 2020. Those patients with PAD were either referred or admitted to our clinic was diagnosed with conventional angiography, computed tomography or Doppler ultrasound. All patients underwent coronary angiography or coronary computed tomography to rule out CAD. Patients were divided into two groups according to the presence of MSAD. Group 1 represented patients with both peripheral and coronary stenosis (MSAD+) (n:293), while group 2 represented those with only PAD without CAD (MSAD-) (n:233).
To enhance quality of care, consecutive patients data are documented in a central data bank. Demographic variables, cardiovascular risk factors and laboratory parameters were obtained from medical records. Patients gave written informed consent in our clinic to provide data for quality control and publications. This study was approved by the Institutional Local Ethics Committee. Patients under 18 and over 85 years old, pregnant, cancer, acute coronary syndrome (ACS), those with chronic inflammatory disease (such as Crohn's disease, rheumatoid arthritis, vasculitis), hepatic disorders, presence of active infection or lack of data were excluded from the study.
Laboratory analysisAll participants laboratory results collected from patient records. Samples of blood tests performed after 12hours of fasting on admission to hospital. Blood samples were centrifuged at speed of 1600 bpm for 15minutes. Roche Cobas C501 autoanalyser system (Roche, Rotkreuz, Switzerland) was used for all biochemical parameters [such as fasting blood glucose, serum creatinine, sodium, potassium, total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein (HDL-C), triglyceride (TG)]. Blood samples were taken into standardized tubes containing dipotassium ethylenedinitrilo tetraacetic acid for complete blood count (CBC). And XN-2000 Hematology system (Bornbarch, Norderstedt, Germany) was used for CBC analysis. All measurements made in our laboratory are regularly validated by relevant establish. Neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), monocyte-to-High Density Lipoprotein ratio (MHR), and platelet-to-lymphocyte ratio (PLR) were calculated by dividing corresponding variables. The plasma atherogenic index (PAI) was calculated as the logarithm [log (TG/HDL-C)] of the ratio of plasma TG to HDL, measured in milligrams per deciliter. Cardiac risk ratio (CRR) was calculated as total cholesterol to HDL cholesterol ratio.
DefinitionsThe following definitions were used: hypertension (HT), blood pressure ≥140/ 90mmHg and/or antihypertensive treatment7; diabetes mellitus (DM), fasting plasma glucose 126mg/dl (6.94 mmol/l) and/or glucose lowering treatment8; hyperlipidemia (HL), total plasma cholesterol levels of>200mg/dl or plasma LDL cholesterol levels of ≥155mg/dl or triglyceride levels of ≥150mg/dl or HDL cholesterol levels in male ≤40mg/dl and in women ≥50mg/dl and/or lipid lowering agents.9 Smokers were defined as participants who reported smoking currently and regularly (at least five cigarettes per day).
PAD is known as a chronic arterial occlusive disease of the lower extremities caused by atherosclerosis. In our study, PAD was defined if there was at least 30% or more stenosis in lower extremities demonstrated by imaging methods.10 In addition, PAD was graded according to the stenosis severity; 30-50%, 50-70%, and>70%.
CAD is characterized by atherosclerotic plaque accumulation in the epicardial arteries, whether obstructive or non-obstructive. Patients who had at least 30-50% or more coronary stenosis and patients undergoing percutaneous transluminal coronary angioplasty or stenting, and those who had undergone coronary bypass surgery were defined as having CAD.11 Severity of the stenosis of both PAD and CAD were evaluated by two independent operators. Intraclass correlation coefficient value was 0.976 (95% CI: 0.965–0.992; p<0.001) between operators. Also, ischemic stroke definition was accepted as follows; caused by a blockage of a blood vessel in the brain that leads to the brain being starved of oxygen, the neurologic signs and symptoms must last longer than 24hours or the brain infarction is demonstrated by imaging techniques, and must have diagnosed by a neurologist.9 Relevant guideline recommendations were usually taken into account for definitions.
Statistical analysisStatistical analyses were conducted using SPSS software version 23.0. Variables were analyzed using visual and analytical methods to determine normal distribution. Mean and standard deviation was used for descriptive statistics. Chi-square test was used to compare nominal and categorical variables (gender, hypertension, and diabetes mellitus). Parametric and non-parametric data was compared using independent sample t-test and Man Whitney U test respectively. Results are shown as mean±standard deviation for continuous variables. In addition, binary logistic regression analysis was performed to determine the associated factors for multiple arterial diseases. Factors with p values <0.1 in univariate analysis were entered into the multivariate model. Two sided P-value <0.05 was considered statistically significant.
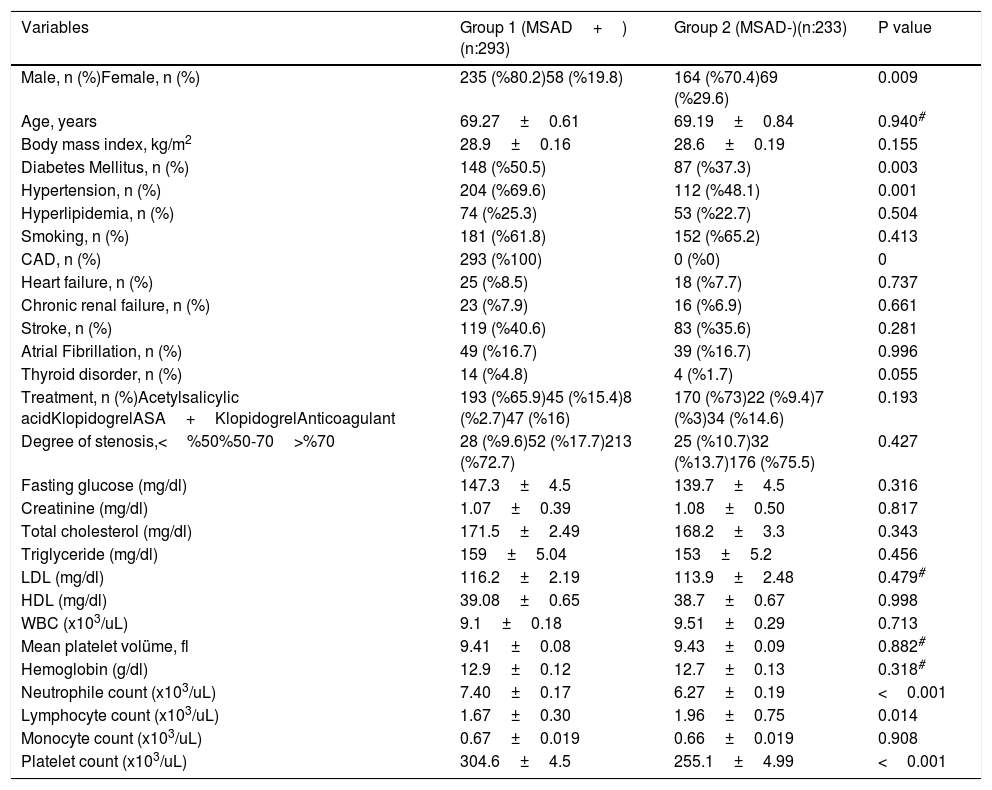
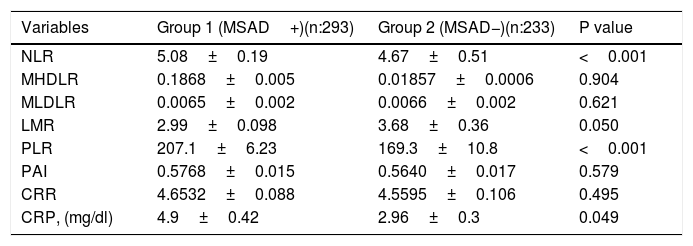
ResultsMean ages of group-1 and group-2 were 69.27±0.61 and 69.19±0.84, respectively. There were significant differences between the groups with regard to gender, DM, and HT. Demographic characteristics and laboratory findings of individuals are summarized in Table 1. Regarding inflammation markers, NLR and PLR was higher in the MSAD+group (p<0.001). However other inflammation markers were similar between groups (Table 2).
Baseline demographic and clinical characteristics of the patients.
| Variables | Group 1 (MSAD+)(n:293) | Group 2 (MSAD-)(n:233) | P value |
|---|---|---|---|
| Male, n (%)Female, n (%) | 235 (%80.2)58 (%19.8) | 164 (%70.4)69 (%29.6) | 0.009 |
| Age, years | 69.27±0.61 | 69.19±0.84 | 0.940# |
| Body mass index, kg/m2 | 28.9±0.16 | 28.6±0.19 | 0.155 |
| Diabetes Mellitus, n (%) | 148 (%50.5) | 87 (%37.3) | 0.003 |
| Hypertension, n (%) | 204 (%69.6) | 112 (%48.1) | 0.001 |
| Hyperlipidemia, n (%) | 74 (%25.3) | 53 (%22.7) | 0.504 |
| Smoking, n (%) | 181 (%61.8) | 152 (%65.2) | 0.413 |
| CAD, n (%) | 293 (%100) | 0 (%0) | 0 |
| Heart failure, n (%) | 25 (%8.5) | 18 (%7.7) | 0.737 |
| Chronic renal failure, n (%) | 23 (%7.9) | 16 (%6.9) | 0.661 |
| Stroke, n (%) | 119 (%40.6) | 83 (%35.6) | 0.281 |
| Atrial Fibrillation, n (%) | 49 (%16.7) | 39 (%16.7) | 0.996 |
| Thyroid disorder, n (%) | 14 (%4.8) | 4 (%1.7) | 0.055 |
| Treatment, n (%)Acetylsalicylic acidKlopidogrelASA+KlopidogrelAnticoagulant | 193 (%65.9)45 (%15.4)8 (%2.7)47 (%16) | 170 (%73)22 (%9.4)7 (%3)34 (%14.6) | 0.193 |
| Degree of stenosis,<%50%50-70>%70 | 28 (%9.6)52 (%17.7)213 (%72.7) | 25 (%10.7)32 (%13.7)176 (%75.5) | 0.427 |
| Fasting glucose (mg/dl) | 147.3±4.5 | 139.7±4.5 | 0.316 |
| Creatinine (mg/dl) | 1.07±0.39 | 1.08±0.50 | 0.817 |
| Total cholesterol (mg/dl) | 171.5±2.49 | 168.2±3.3 | 0.343 |
| Triglyceride (mg/dl) | 159±5.04 | 153±5.2 | 0.456 |
| LDL (mg/dl) | 116.2±2.19 | 113.9±2.48 | 0.479# |
| HDL (mg/dl) | 39.08±0.65 | 38.7±0.67 | 0.998 |
| WBC (x103/uL) | 9.1±0.18 | 9.51±0.29 | 0.713 |
| Mean platelet volüme, fl | 9.41±0.08 | 9.43±0.09 | 0.882# |
| Hemoglobin (g/dl) | 12.9±0.12 | 12.7±0.13 | 0.318# |
| Neutrophile count (x103/uL) | 7.40±0.17 | 6.27±0.19 | <0.001 |
| Lymphocyte count (x103/uL) | 1.67±0.30 | 1.96±0.75 | 0.014 |
| Monocyte count (x103/uL) | 0.67±0.019 | 0.66±0.019 | 0.908 |
| Platelet count (x103/uL) | 304.6±4.5 | 255.1±4.99 | <0.001 |
P<0.05 statistical significance, # Mann Whitney U test,±: standard deviation, n: individual number. MSAD: Multiple arterial disease, CAD: Coronary artery disease, LDL: Low Density Lipoprotein, HDL: High Density Lipoprotein, WBC: white blood cell.
Inflammatory markers between groups.
| Variables | Group 1 (MSAD+)(n:293) | Group 2 (MSAD−)(n:233) | P value |
|---|---|---|---|
| NLR | 5.08±0.19 | 4.67±0.51 | <0.001 |
| MHDLR | 0.1868±0.005 | 0.01857±0.0006 | 0.904 |
| MLDLR | 0.0065±0.002 | 0.0066±0.002 | 0.621 |
| LMR | 2.99±0.098 | 3.68±0.36 | 0.050 |
| PLR | 207.1±6.23 | 169.3±10.8 | <0.001 |
| PAI | 0.5768±0.015 | 0.5640±0.017 | 0.579 |
| CRR | 4.6532±0.088 | 4.5595±0.106 | 0.495 |
| CRP, (mg/dl) | 4.9±0.42 | 2.96±0.3 | 0.049 |
P<0.05 statistical significance, NLR: Neutrophil / lymphocyte ratio, MHDLR: Monocyte / HDL ratio, MLDLR: Monocyte / LDL ratio, LMR: Lymphocyte / Monocyte ratio, PLR: Platelet / Lymphocyte ratio, PAI: Plasma atherogenic index, CRR: Cardiac risk ratio, CRP: C-reactive protein.
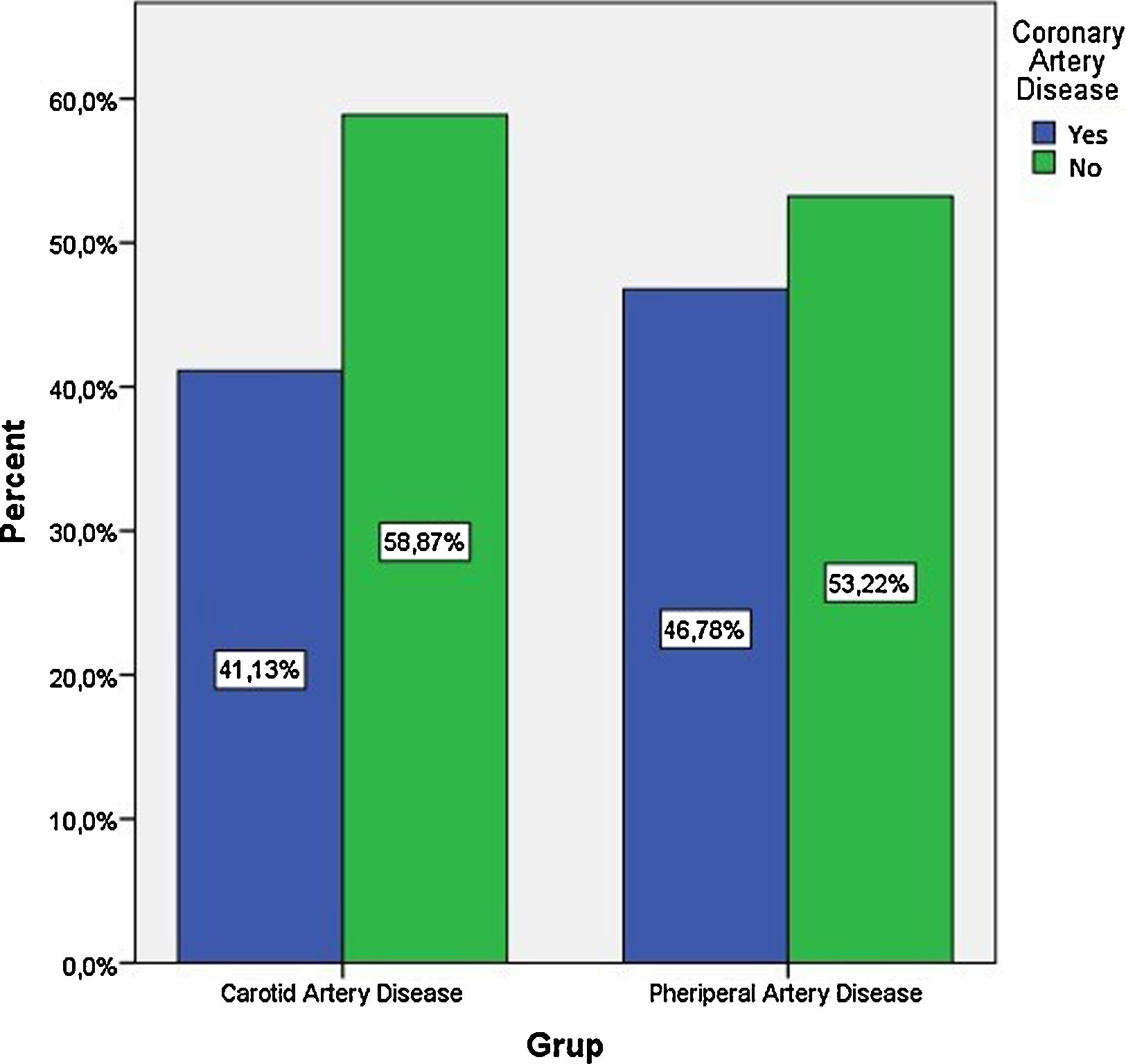
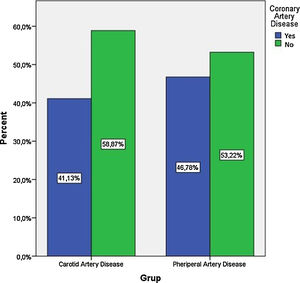
The frequency of coronary artery disease between patients with peripheral and carotid artery disease was not different (59% vs. 53% p>0.05), Figure 1.
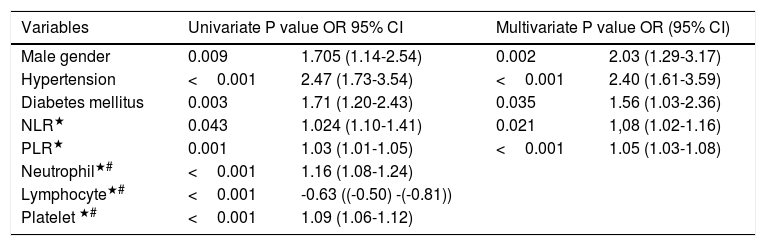
In logistic regression analysis, HT [odds ratio (OR): 2.40 (1.61-3.59)); p<0.002], male gender [OR: 2.03 (1.29-3.17); p=0.002], DM [OR:1.56 (1.03-2.36); P=0.035], NLR [OR: 1,08 (1.02-1.16); p=0.021], and PLR [OR:1.05 (1.03-1.08); p<0.001] were found to be associated with MSAD (Table 3)
Univariate and Multivariate Logistic Regression Analysis for the Presence MSAD.
| Variables | Univariate P value OR 95% CI | Multivariate P value OR (95% CI) | ||
|---|---|---|---|---|
| Male gender | 0.009 | 1.705 (1.14-2.54) | 0.002 | 2.03 (1.29-3.17) |
| Hypertension | <0.001 | 2.47 (1.73-3.54) | <0.001 | 2.40 (1.61-3.59) |
| Diabetes mellitus | 0.003 | 1.71 (1.20-2.43) | 0.035 | 1.56 (1.03-2.36) |
| NLR★ | 0.043 | 1.024 (1.10-1.41) | 0.021 | 1,08 (1.02-1.16) |
| PLR★ | 0.001 | 1.03 (1.01-1.05) | <0.001 | 1.05 (1.03-1.08) |
| Neutrophil★# | <0.001 | 1.16 (1.08-1.24) | ||
| Lymphocyte★# | <0.001 | -0.63 ((-0.50) -(-0.81)) | ||
| Platelet ★# | <0.001 | 1.09 (1.06-1.12) | ||
P<0.05 statistical significance, CI: Confidence interval, OR: Odds Ratio Model -2 Log Likelihood: 534.55, Nagelkerke R square: 0.401. ★ Odds ratio referred one unit change of corresponding variable. #These parameters are not entered the model to in order to prevent multicollinearity.
To our knowledge this is the first study to evaluate the association between inflammation markers and MSAD. Among various clinical presentations of atherosclerosis, MSAD is defined as the simultaneous presence of clinically significant atherosclerotic lesions in at least two major vascular territories. It is known that cardiovascular outcomes are linked to atherosclerotic burden. Currently, the role of inflammation in the development of atherosclerotic CVD is obvious. According to our study findings, HT [odds ratio (OR): 2.40 (1.61-3.59)); p<0.002], male gender [OR: 2.03 (1.29-3.17); p=0.002], DM [OR:1.56 (1.03-2.36); P=0.035], NLR [OR: 1,08 (1.02-1.16) p=0.021], and PLR [OR:1.05 (1.03-1.08); p<0.001] were associated with MSAD.
The development and progression of atherosclerosis is a multifactorial process, and different arterial beds are affected by similar atherosclerotic risk factors. The relationship between NLR and CVD has not been fully elucidated. However, it is thought that systemic factors such as inflammation, endothelial dysfunction, and oxidative stress may play a role.12 The relationship of these markers with the progression of atherosclerosis and their prognostic significance in cardiovascular disease were evaluated in previous studies. It was found that the progression rate of atherosclerosis was significantly higher in patients with high NLR and that this was a predictor of the progression of atherosclerosis.13 In patients with stroke, NLR is an independent mortality predictor in the short and long term.14 Also, NLR is a predictor of mortality in patients with ischemic CAD, both in stable CAD15 and in ACS.11,12 However, there has been no study to date investigating the association between NLR and MSAD. We found that NLR was associated with MSAD. Hence, we can assume that NLR was linked to the extent of atherosclerosis.
Previous studies have shown that concomitant LEAD (clinical or subclinical) is also associated with worse outcomes in patients undergoing coronary artery bypass grafting.18 This is also true for carotid artery patients. In a study including 276 patients with non-cardioembolic ischemic stroke / transient ischemic attack, coronary computed tomography detected coronary stenosis (>50%) in 18% of cases, and the prevalence was 4-fold higher in the case of carotid stenosis>50%.19 In our study, the prevalence of CAD was 53.22% and 58.87% in LEAD and carotid artery disease, respectively. Our findings were consistent with previous studies.16,17
Increased platelet activation also plays an important role in the initiation and progression of atherosclerosis.20 Higher platelet counts may reflect increased platelet activation, and those also have been found to be involved in the development of atherosclerosis and ACS.21 In addition, low lymphocyte counts show a depressed immune response that is associated with adverse outcomes in cardiovascular disorders.22 In a meta-analysis involving 6627 participants, it was shown that high PLR level was associated with all-cause mortality and cardiovascular events in patients with ACS, both in-hospital and in the long term period.5 In addition, it was shown that PLR was directly correlated with the severity of coronary and carotid artery stenosis.23,24 Another study demonstrated PLR was not only correlated with carotid artery stenosis but also predicted stroke in patients who underwent carotid endarterectomy.25 On the other hand, several studies have demonstrated an association between inflammatory markers and the incidence, severity, response to treatment, and prognosis of PAD.22,23 In our study, while PLR and platelet values were higher in MSAD patients, only platelets predicted the presence of MSAD. CRP was also higher in MSAD. In conclusion, elevation of several inflammatory parameters in MSAD might suggest a close relationship between inflammation and the extent of atherosclerosis.
Limitations of the studyThere are a few limitations of our study that should be considered. The major limitation of this study was the retrospective and single center design. The small number of cases was another drawback. Our results for NLR and PLR variables may have been affected by confounding factors such as age, gender, BMI, and medical treatments. Our results need to be tested with more comprehensive studies in which the effects of these situations can be limited. Although baseline demographic comparisons did not differ significantly between groups, this may have affected our results. The anti-inflammatory effects of some drugs such as statins could not be ruled out, since they are commonly used in these patient groups. We also could not investigate the association of highly sensitive CRP with MSAD since it was not regularly used in routine clinical practice.
ConclusionIn this study, we demonstrated that NLR and PLR may be associated with MSAD. In other words, the degree of inflammation could be deemed to indicate the extent of atherosclerosis. NLR and PLR are simple and widely available inflammatory parameters and may be used as surrogate markers for diffuse atherosclerosis.
Authors’ contributionsConcept and design of study: ZY, MA Analysis and interpretation of data. ZY, MA, SVE Drafting and critical revision of the article. ZY, MA, SVE
DisclosureNo competing financial interests exist.
FundingThe study did not have any supporters.
Conflict of interest statementOn behalf of all authors, the corresponding author states that there is no conflict of interest.