The latest cardiovascular risk guides, European and American, establish hard lipid control objectives, that suppose a therapeutic challenge for both, doctor and patient. The objective of this study is determine the degree of adequacy of low-density lipoprotein cholesterol levels (LDLc) presented by patients with very high cardiovascular risk in our healthcare area, with respect to European and American cardiovascular risk guidelines.
MethodsThis is an observational and retrospective study of 446 patients discharged between June 2017 and June 2018 with a diagnosis of acute coronary syndrome, ischemic stroke and peripheral arterial disease. We have defined a series of variables among which we want to highlight the levels of LDLc at admission, and its follow-up at discharge, in order to know the degree of lipid control according to current European guidelines, which set the threshold to consider optimal control in patients of very high cardiovascular risk, below 55 mg/dl.
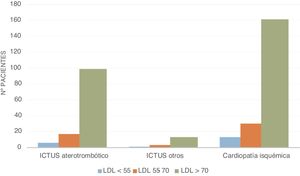
ResultsThe revised data indicates a control of the patients in 36.6% according to the 2016 guidelines (LDLc <70 mg/dl) and 14.8% according to the current 2019 guidelines (LDLc <55 mg/dl), 75.3% of them received lipid lowering treatment. We have also found that the number of absolute events increases exponentially depending on the levels of LDLc, being more evident in patients with acute coronary syndrome.
ConclusionsIn this study, we demonstrated that the adequacy of the vascular risk clinical practice guidelines is insufficient in the population with very high vascular risk, in line with other published studies, further studies would be needed to determine the causes. A solution to this problem could be collaboration with the Internal Medicine service that has been launched in our healthcare area in order to derivate patients to the Vascular Consultation whom could be beneficiated by the administration of the PCSK9 inhibitors.
Las últimas guías de riesgo cardiovascular tanto europeas como estadounidenses, establecen unos objetivos de control lipídico muy exigentes que suponen un reto terapéutico tanto para el médico como para el paciente. El objetivo de este estudio es conocer el grado de adecuación de los niveles de colesterol unido a lipoproteínas de baja densidad (cLDL) que presentan los pacientes de muy alto riesgo cardiovascular de nuestra área sanitaria, con respecto a las guías de riesgo cardiovascular europeas y estadounidenses.
MétodosSe trata de un estudio observacional y retrospectivo de 446 pacientes dados de alta entre junio 2017 y junio 2018 con diagnóstico de síndrome coronario agudo, ictus isquémico y enfermedad arterial periférica. Hemos definido una serie de variables entre las que queremos destacar las cifras de cLDL al ingreso y su evolución tras el alta con el objetivo de conocer el grado de control lipídico acorde a las guías europeas actuales, que sitúan el umbral para considerar un control óptimo en pacientes de muy alto riesgo cardiovascular, por debajo de los 55 mg/dl.
ResultadosLos datos revisados indican un control en el 36,6% de los pacientes según las guías de 2016 (cLDL<70 mg/dl) y del 14,8% según las actuales de 2019 (cLDL<55 mg/dl), de todos ellos recibían tratamiento hipolipemiante el 75,3%. También hemos evidenciado que el número de eventos absolutos aumenta exponencialmente en función de las cifras de cLDL, siendo más evidente en los pacientes con síndrome coronario agudo.
ConclusionesEn este estudio, demostramos que la adecuación de las guías de práctica clínica de riesgo vascular es insuficiente en la población de muy alto riesgo vascular, lo que está en consonancia con otros estudios publicados, harían falta más estudios para determinar las causas. Una solución para este problema podría ser la colaboración con el servicio de Medicina Interna que se ha puesto en marcha en nuestra área sanitaria para derivar a la consulta de Riesgo Vascular a aquellos pacientes candidatos a la administración de los inhibidores de PCSK9.
The degree of lipid control has been the starting point for countless debates in the medicine of today, addressed during both primary care consultations and specialised cardiovascular risk consults. The main objective they focus on is secondary prevention in those patients who have already presented a cardiovascular event, which places them in the very high risk category.
The latest updates of the leading guidelines on lipid control tend to be increasingly stringent in terms of cholesterol levels, proposing optimisation of the levels currently considered to reflect control. Thus, recommended LDL-C levels for these patients according to the European Society of Cardiology Guidelines on Management of Dyslipidaemia (ESC/EAS 2019)1 and the American Endocrinology Guidelines for the Management of Dyslipidaemia and the Prevention of Cardiovascular Disease (AACE/ACE 2017)2 have recently been modified. Whereas previously, according to the guidelines published in 2016, the target figure was set at less than 70 mg/dl, LDL-C levels below 55 mg/dl are now contemplated as optimal control for these patients.
Despite the trend towards lower and lower LDL-C, studies carried out to date, such as REPAR3 and EURASPIRE4, reveal that there is still some way to go before these ambitious goals are met.
Therefore, as a result of this need to improve the control of these patients, the main objective of this study was to determine the degree of alignment of lipid control in relation to the primary cardiovascular risk guidelines in our health management area. To this end, we used the computer tools available to us, with the intention of discerning our starting point, so as to enhance the quality of care in our healthcare area in a multidisciplinary manner.
Material and methodsWe designed an observational, descriptive, retrospective, multicentre, retrospective study, conducted in agreement with Primary Care of the Southern Health Area of Cordoba and the Internal Medicine Department of the Hospital Infanta Margarita. The sample was collected through the minimum basic set of hospital discharge data.
It included 446 patients who were discharged between June 2017 and June 2018 with a diagnosis of acute coronary syndrome, ischaemic stroke, or peripheral arterial disease. No exclusion criteria were applied, although analytical control data could not be obtained for all patients; consequently, the statistical study was finally conducted with 352 patients.
Using computerised medical records in the DIRAYA programme, data were collected with respect to the variables of age, sex, smoking status, and the presence or absence of the following diseases in their history: type 2 diabetes mellitus, arterial hypertension, chronic renal failure, and previous cardiovascular events (those described above).
Other laboratory values were similarly collected, such as: serum creatinine (mg/dl), total cholesterol (mg/dl), LDL-C (mg/dl), HDL-C (mg/dl), non-HDL cholesterol (mg/dl), triglycerides (mg/dl), and glycosylated haemoglobin (HbA1c [%]).
Data relative to lipid control and treatment of the selected patients were collected in 2 phases: pre-event (baseline analysis and most recent treatment before the diagnosis of the cardiovascular event studied) and post-event (analytical control and treatment following the cardiovascular event).
In addition, readmissions or deaths of the participants selected were collected between June 2018 and June 2019, as well as information about the healthcare centre the patients corresponded to and their assigned Primary Care Physician for future contacts.
To establish the degree of control, the AACE/ACE 2017 and ESC/EAS 2019 guidelines were used, which set a treatment target of LDL-C of less than 70 mg/dl and less than 55 mg/dl, respectively, for patients at very high cardiovascular risk.
Data were collected using the Microsoft Excel office application for Microsoft 365 MSO (16.0.13801.20240, 32-bit. Version 2102) and statistical analyses were performed using SPSS version 25 (IBM SPSS Statistics for MacOS, Version 25.0. Armonk, NY, USA).
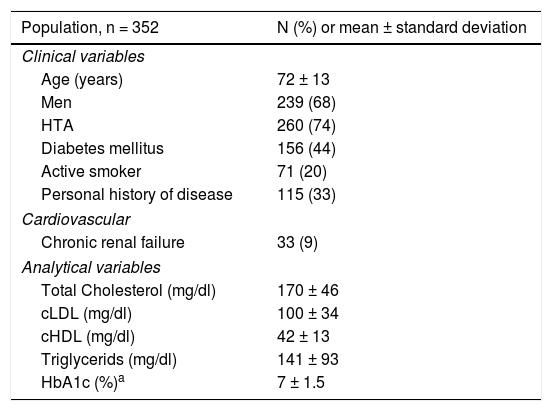
ResultsA total of 446 patients were identified for the specified period of time; of them, 94 were ruled out due to lack of analytical data (no laboratory data, determination made at a different centre, deaths, etc.), so that statistical analyses were conducted with [the data from] 352 patients. As for the different types of events recorded, 212 fall within the spectrum of acute coronary syndrome; 125, ischaemic stroke, and 15, peripheral arterial disease. Other clinical and analytical variables were also analysed and are presented in Table 1.
Clinical variables and analytical determinations in the baseline sample.
| Population, n = 352 | N (%) or mean ± standard deviation |
|---|---|
| Clinical variables | |
| Age (years) | 72 ± 13 |
| Men | 239 (68) |
| HTA | 260 (74) |
| Diabetes mellitus | 156 (44) |
| Active smoker | 71 (20) |
| Personal history of disease | 115 (33) |
| Cardiovascular | |
| Chronic renal failure | 33 (9) |
| Analytical variables | |
| Total Cholesterol (mg/dl) | 170 ± 46 |
| cLDL (mg/dl) | 100 ± 34 |
| cHDL (mg/dl) | 42 ± 13 |
| Triglycerids (mg/dl) | 141 ± 93 |
| HbA1c (%)a | 7 ± 1.5 |
To reach the conclusions of the study, we concentrated chiefly on LDL-C values; 73 patients from of our sample displayed [acceptable] lipid control <70 mg/dl at baseline (20.7%), while the remaining 279 patients (79.3%) had LDL-C values exceeding 70 mg/dl. Other determinations of note were: total cholesterol, 170 ± 46 mg/dl; triglycerides, 141 ± 93 mg/dl; HDL-C 42 ± 13 mg/dl, and HbA1c, 7 ± 1.5%.
Of all those patients whose LDL-C was >70 mg/dl levels at baseline, 75.6% were on statin therapy; 5.8% were taking statin plus ezetimibe; 0.7% were receiving statin plus fibrates; 1% were taking fibrates alone, and 16.8% of the patients were not receiving any lipid-lowering treatment.
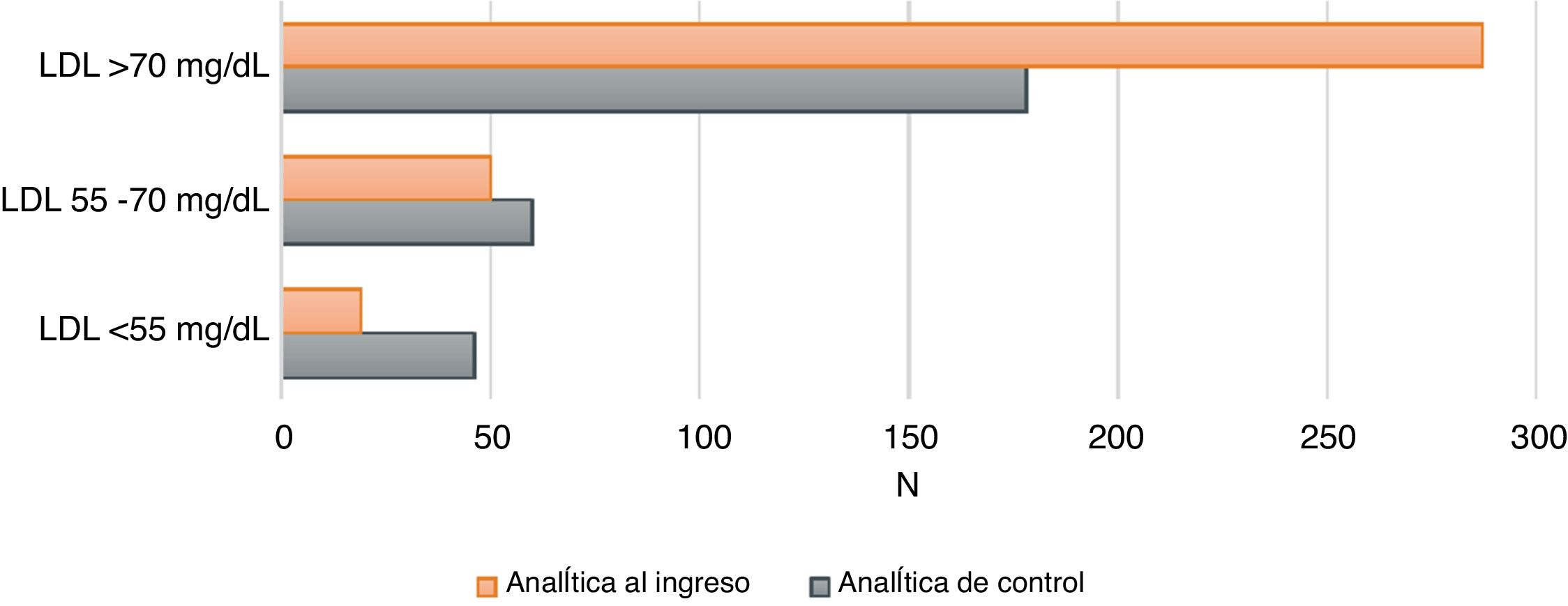
Fig. 1 illustrates how better lipid control is achieved after optimal treatment adjustment at their clinical check-up three months after the event.
Degree of lipid controlThe data reviewed indicate that 36.6% of the patients meet the control criteria set by the 2016 guidelines (LDL < 70 mg/dl) and only 14.8% meet the criteria of the current guidelines (LDL < 55 mg/dl) (of a total of 284 available post-admission control analyses).
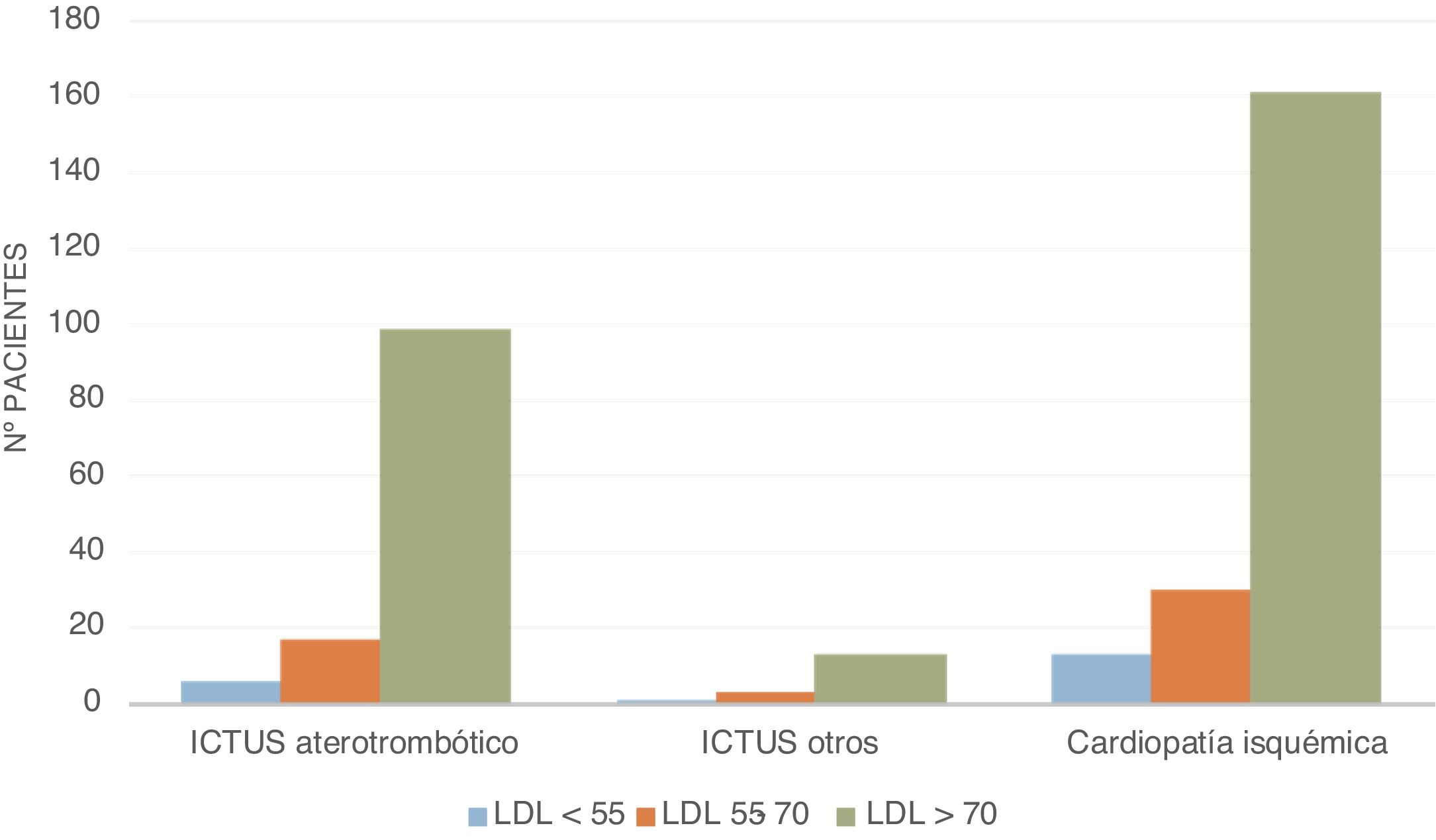
Fig. 2 shows the distribution of the study population according to the event presented, based on the range of LDL-C in the baseline analysis at the time of admission (mg/dl), with most patients exhibiting acute coronary syndrome in relation to LDL-C levels.
As for the relationship between the absolute number of events and LDL-C, 80.62% of the sample had LDL-C levels of >70 mg/dl and only 5.33% had LDL-C levels of <55 mg/dl.
Upon examining the relationship between LDL-C levels and non-modifiable patient factors and other cardiovascular risk factors, increased prevalence was observed in males compared to females and an increase in the absolute number of events in hypertensive patients compared to patients who only had diabetic.
DiscussionOf all the patients reviewed, only 36.6% of them met the lipid control targets set by the 2016 guidelines (LDL-C <70 mg/dl) and 14.8% as per the guidelines currently in force (LDL-C <55 mg/dl).
The data from the present study reveal that there is room for improvement in the degree of lipid control in secondary prevention in very high-risk patients in our healthcare area. If we compare them with published studies applying a similar approach, the data from our area are a long way from, for instance, the figures achieved in the health area of the Hospital Costa del Sol, as reflected in the communication by Martín Domínguez et al.,5 inasmuch as they achieved control figures of up to 75.8% three months following the event. In contrast, our results are more in line with those reported in other international studies, such as REPAR, in which only 26% of patients had LDL-C concentrations below 70 mg/dl, despite 95.3% of patients receiving lipid-lowering drugs, or CODIMET,6 in which more than half of the participants studied did not achieve their targets, also reflecting the fact that high-intensity treatment is the key factor in achieving proper control.7,8
Furthermore, therapeutic inertia may have influenced the poor results of our study, since the vast majority of the patients included were receiving hypolipidemic treatment and yet, after the cardiovascular event occurred, this treatment had not been modified, leaving the possibility open of moving up the treatment ladder with other high-potency lipid-lowering drugs or with pharmacological associations.1
This is where the question arises as to why these results may be so far off the targets set. On the one hand, we may think of a lack of lifestyle modification on the patient’s part, including changes in dietary habits, exercise, or smoking cessation,4 as well as adherence, and therapeutic optimisation,3 a basic pillar of the treatment to maintain optimal cholesterol levels, as demonstrated in previous studies, such as ESPROCOL.9
ConclusionsThe implementation of protocols that focus on optimising the treatment of patients at very high cardiovascular risk, including changes in lifestyle (diet, exercise, smoking, etc.), as well as promoting adherence to treatment, are a basic mainstay in improving LDL-C values. Moreover, our results show that it is essential to optimise treatment, by using high-potency statins or a combination of several lipid-lowering drugs, as well as screening individuals who can be studied at a Vascular Risk consultation to assess the possibility of starting treatment with PCSK9 inhibitors, as it is key that we locate patients with very high LDL-C values that point toward familial hypercholesterolaemia and investigate their diagnosis. To this end, we believe that close collaboration between Internal Medicine and Primary Care is essential.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Aneri M, Fernández G, Gras M, Campaña A, Sánchez R, Sánchez J. Grado de control lipídico de un Área de Gestión Sanitaria en pacientes de muy alto riesgo cardiovascular. Clin Investig Arterioscler. 2021;33:198–202.