Sedentarism and physical inactivity is highly prevalent globally, and are associated with a wide range of chronic diseases and premature deaths. The interest in sedentary behaviour is justified by a growing body of evidence that points to a relationship between this lifestyle and the increase in the prevalence of obesity, diabetes and cardiovascular disease. It has been known throughout history that being inactive is unhealthy, but nowadays almost one-third of the world's population is inactive, thus representing a major public health problem.
El sedentarismo y la inactividad física son altamente prevalentes globalmente y están asociados a un amplio rango de enfermedades crónicas y muerte prematura. El interés en la conducta sedentaria está justificado por la creciente evidencia que apunta hacia una relación entre esta conducta y el incremento en la prevalencia de obesidad, diabetes y enfermedad cardiovascular. A través de la historia es bien conocido que ser inactivo no es saludable, pero hoy día casi un tercio de la población del mundo es inactiva, lo que representa un serio problema de salud pública.
Many readers will be aware of the dose/response relationship that exists between exercise and health: the greater the physical activity (PA), the better the individual's overall health. However, few studies have focused on the consequences of lack of PA, and this will be the main subject of this article.
It is easier to understand the significance of the change in human beings from a nomadic to a sedentary lifestyle by looking back on our evolutionary history.
About 3.7 million years ago, one of the first hominids to walk on two feet appeared in Ethiopia: Australopithecus afarensis. Bipedalism allowed these hominids to use their hands to grasp branches and stones as tools or weapons, and to gather food (fruits, seeds, roots, etc.), while their long legs allowed them to travel farther and depend less on trees. In addition, their slightly curved hands, shorter fingers, and arched feet allowed them to climb trees, while the medial arch of the foot allowed them to run after their prey or flee from predators or enemy tribes.1
The design of the human organism (encoded in its genes) is known to be the result of millions of years of biological evolution. Nearly all the human genome was formed before the transition from hunting and gathering to farming, and this is believed to have been the optimal genome - the one that enabled us to adapt to the changing environmental conditions faced by our ancestors at each stage of our evolution.
In nature, obtaining food always requires high muscle energy expenditure. This is true of both carnivores (running in pursuit of prey) or herbivores (looking for the best foliage and, in smaller animals, watching out for predators). The capacity of our metabolism to adapt to cycles of abundance and food shortage (the thrifty genotype) was a beneficial factor in the evolution of our ancestors.2 When food was abundant, our thrifty metabolism took over, allowing us to accumulate large amounts of energy in the form of fatty deposits and muscle glycogen. Individuals with the thrifty phenotype were less likely to die out during periods of famine, since they were more efficient at using the energy stored in their body. Muscle proteins were conserved, and muscle contraction was more efficient, increasing their likelihood of finding food and surviving the crisis.2
It is also interesting to note the impact on the central nervous system, which controls all bodily movements at all time variables, from milliseconds to hours, days, months and years, leading to the evolutionary-induced expansion of certain regions of our cerebral cortex.1 As a result, PA strengthened both muscle and brain cells.
Homo sapiens (“wise man”, because he had certain skills absent in his predecessors) appeared in Africa 300,000 years ago and ranged over the continent for 200,000 years before spreading to the rest of the world, even as far as Australia. It was this expansion that sparked a major cognitive revolution about 70,000 years ago, further expanding our ecological niches, defined as the way in which we interact with our environment. In fact, this intellectual “big bang” facilitated the development of amazing cognitive skills, such as the ability to learn, understand and anticipate complex phenomena, memorise a great deal of detail, and establish multiple communications with the environment, particularly with other humans.3 About 10,000 years ago, several human groups discovered ways to produce certain foods, compelling them to create settlements and abandon their nomadic lifestyle.3
This summary of our evolution shows that human beings are active by nature. They spent most of their evolutionary history wandering over the land, and only transitioned to sedentary lifestyle about 10,000 years ago, when they became farmers.
Even the most ancient civilisations knew that reducing the amount of physical effort made in our daily life causes the organs that govern bodily movement to lower their output and adapt their operative capacity to the lower demands of their social group. However, Hippocrates (377 b.c.) believed in the benefits of PA, and warned that4: “All parts of the body which have a function, if used in moderation and exercised in labors in which each is accustomed, become thereby healthy, well developed and age more slowly, but if unused they become liable to disease, defective in growth and age quickly”.
However, reliable scientific evidence of the relationship between physical inactivity and the risk of chronic disease only began to emerge in the mid 1950s5, sparking interest in research into the four basic aspects of the problem6–10:
- a.
The increased use of technology to accomplish daily tasks, making humans more sedentary.
- b.
The physiological evidence of specific effects that sedentary behaviour has on our metabolism and health.
- c.
Instruments, such as accelerometers and questionnaires, can now be used to objectively and reliably measure the time spent physically inactive.
- d.
The difficulties involved in motivating individuals to become more active and engage in more strenuous PA in order to reduce sitting time. This is the most pressing area of study.
The situation is further complicated by the fact that sedentary behaviour does not simply mean less PA, but involves a set of individual attitudes in which sitting or lying becomes the predominant postural form, thus greatly reducing energy expenditure. Furthermore, sedentary behaviour is found in a multitude of places and situations: at work, at school, at home, in our means of transport and our leisure activities, and is accompanied by other harmful habits, such as increased caloric intake or smoking.
In recent decades, sedentary behaviour has become a serious problem that has been aggravated over time by the introduction of new technological inventions. These devices, which are designed to make our lives easier, have ultimately increased our immobility, since working, playing, shopping or doing housework no longer requires the same physical effort needed 50 years ago. Today, everything can be done using a computer, a washing machine, a dryer, a car and other devices developed to reduce our muscle activity and increase our sedentary behaviour.
Sedentary behaviour as a diseaseThe morbidity associated with sedentary behaviour came increasingly under the spotlight in the 1990s, through programmes introduced in several countries to encourage PA and health. These programmes, which were basically devised to disseminate PA and health recommendations, are based on the notion that the general population is unaware of the importance and need for PA, and, therefore, do not engage in such activities.
Given the scale of the problem, the World Health Organization (WHO) released a report in 2004,11 subsequently updated in 2010,12 that lists sedentary behaviour as the fourth greatest risk factor for mortality (6% of deaths recorded worldwide).
A more recent report estimated that physical inactivity is responsible for:13
- –
6% of the burden of disease from coronary heart disease (CHD).
- –
7% of type 2 diabetes mellitus (DM2).
- –
10% of breast cancer.
- –
10% of colon cancer.
- –
Inactivity is responsible for 9% of premature mortality or >5.3% of the 57 million deaths that occurred worldwide in 2008.
If inactivity were decreased by 10% or 25%, >533,000 and >1.3 million deaths, respectively, may be averted each year.13 By eliminating physical inactivity, the life expectancy of the world's population is estimated to increase by 0.68 (0.41 to 0.95) years.13
Physical inactivity also carries a heavy economic burden. A report published in 2016 with data from 142 countries (93.2% of the world's population) estimated the direct health costs and disability-adjusted life-years (DALYs) for various diseases:14
- –
Physical inactivity cost health-care systems 53.8 billion international dollars (Int’l$) in 2013.
- –
Physical inactivity-related deaths contribute to Int’l$ 13.7 billion in productivity losses.
- –
Physical inactivity was responsible for 13.4 million DALYs worldwide.
- –
High-income countries bear a larger proportion of economic burden (80.8% of health-care costs and 60.4% of indirect costs), whereas low-income and middle-income countries have a larger proportion of the disease burden (75.0% of DALYs).
As for prevalence, a recent study estimates that more than one in four adults (28% or 1.8 billion people) are physically inactive (one in three in some countries)15, and women are less active than men, with more than 8% difference between the sexes (32% in men vs. 24% in women). High-income countries have the highest levels of inactivity (32%) compared to 26% and 16%, respectively, in middle- and low-income countries. These results highlight the urgent need to prioritise actions aimed at creating an environment conducive to increasing PA.
Sedentary behaviour as a risk factorThe extent of the problem and the role of PA as a risk factor for disease is outlined in the WHO report published in 2014.16 Briefly:
- –
The risk of death from any cause is higher among adults with insufficient PA compared with those who practise at least the minimum recommendation of 150minutes of moderate physical exercise per week or equivalent.
- –
23% of adults aged 18 years or older did not do enough PA. Women were less active than men, and older people were less active than young people.
- –
Worldwide, 81% of adolescents (aged 11 to 17) did not do enough PA in 2014, with girls being less active than boys; and 84% and 78%, respectively, did not meet the WHO global recommendations on physical activity for health.
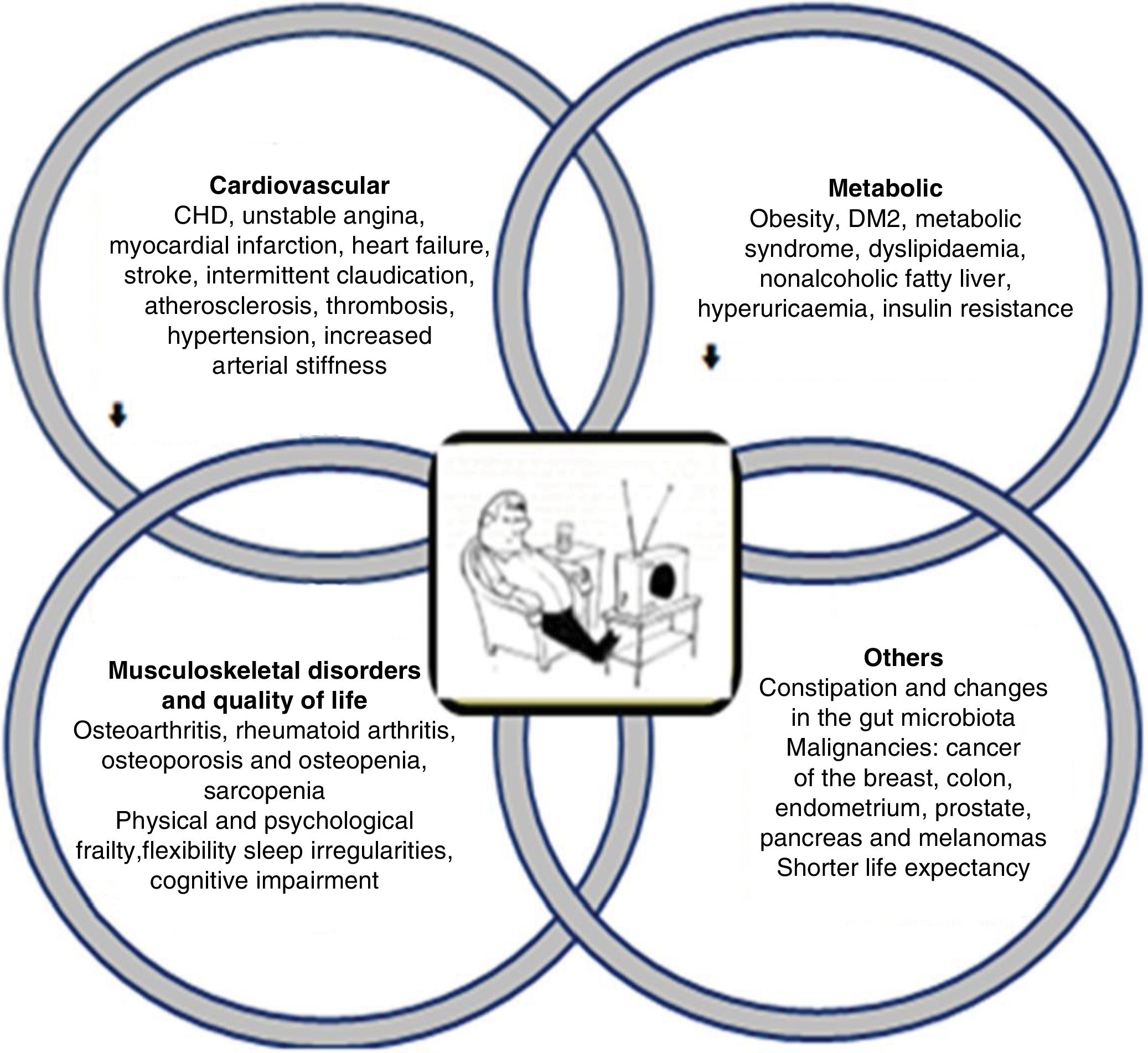
The clinical consequences of sedentary behaviour on various bodily systems are wide-ranging and inter-related (Fig. 1). They can be summarised as functional and/or organic alterations:8,10,17–28
- –
Metabolic: obesity, insulin resistance, DM2, dyslipidaemia, metabolic syndrome, hyperuricaemia.
- –
Cardiovascular diseases: CHD, unstable angina, myocardial infarction, heart failure, stroke, intermittent claudication, atherosclerosis, thrombosis, hypertension, increased arterial stiffness.
- –
Pulmonary alterations: asthma, chronic obstructive pulmonary disease.
- –
Neurological diseases: intellectual dysfunction, dementia, depression, mood disorder and anxiety, Alzheimer's disease.
- –
Musculoskeletal disorders: osteoarthritis, rheumatoid arthritis, osteoporosis and osteopenia, sarcopenia.
- –
Greater physical frailty, especially in the elderly, which, in turn, increases the risk of morbidity and mortality.
- –
Quality of life: decreased psychological well-being, psychological frailty, inability to perform activities of daily living and social interactions, functional restriction, loss of balance, flexibility and reaction and sleep irregularities (difficulty falling asleep, frequent waking during the night, or waking up very early in the morning).
- –
Constipation and changes in the gut microbiota.
- –
Malignancies, such as cancer of the breast, colon, endometrium, prostate, pancreas and melanomas.
- –
Shorter life expectancy.
Clinical consequences of sedentary behaviour. The pathophysiological effects of sedentary behaviour encompass a wide range of disorders, particularly cardiovascular and metabolic alterations, favouring or accelerating progression to diabetes or atherosclerotic cardiovascular disease.
Logically, metabolic and cardiovascular alterations are the most common and the most characteristic of the burden of disease, because once established they gradually progress, despite aggressive treatment. The other alterations, however, can be reversed or improved by exercise programmes and pharmacological therapy, if necessary.
A recently identified consequence of sedentary behaviour is the loss of metabolic flexibility,8,29,30 that is, the ability to adapt substrate oxidation rates in response to changes in fuel availability. The inability to switch between the oxidation of lipids and carbohydrates appears to be an important feature of chronic disorders such as obesity and type 2 diabetes. Evidence has shown that high levels of physical activity predict metabolic flexibility, while physical inactivity and sedentary behaviours trigger a state of metabolic inflexibility, even in subjects who meet PA recommendations.8,29,30
Definition of termsIn their Terminology Consensus Project,31 the Sedentary Behaviour Research Network established and defined the following terms:
- –
PA: any body movement generated by the contraction of skeletal muscles that raises energy expenditure above resting metabolic rate. It is characterised by its modality, frequency, intensity, duration, and context of practice.
- –
Physical inactivity: the non-achievement of physical activity guidelines.
- –
Exercise: a subcategory of PA that is planned, structured, repetitive, and that favours physical fitness maintenance or development.
- –
Sport: part of the PA spectrum and corresponds to any institutionalised and organised practice, based on specific rules.
- –
Sedentary behaviours: any waking behaviours characterised by an energy expenditure ≤1.5 METs, while in a sitting, reclining, or lying posture.
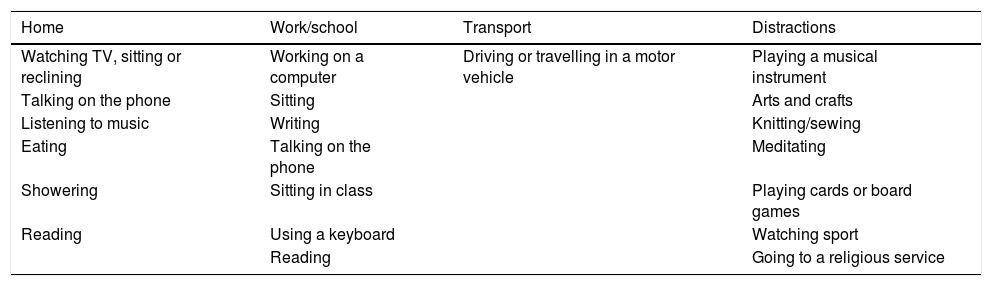
Table 1 lists some activities with an energy expenditure of less than 1.5 METs, and, therefore, classed as sedentary. These activities should be borne in mind when estimating sedentary behaviour, as patients will not usually consider them to be sedentary.
Sedentary activities with energy expenditure <1.5 MET.
| Home | Work/school | Transport | Distractions |
|---|---|---|---|
| Watching TV, sitting or reclining | Working on a computer | Driving or travelling in a motor vehicle | Playing a musical instrument |
| Talking on the phone | Sitting | Arts and crafts | |
| Listening to music | Writing | Knitting/sewing | |
| Eating | Talking on the phone | Meditating | |
| Showering | Sitting in class | Playing cards or board games | |
| Reading | Using a keyboard | Watching sport | |
| Reading | Going to a religious service |
MET: metabolic equivalent; TV: television.
Taken from Young et al.17
It is important to note that although the terms sedentary behaviour and physical inactivity are used indistinctly, there is a clear distinction between them. Sedentary behaviour involves spending a great deal of time engaging in low-energy-expenditure activities (<1.5 MET), whereas physical inactivity is an almost total absence of PA.16,17
It is interesting to note that an increase in the time devoted to sedentary behaviours correlates with an increase in cardiovascular and metabolic risk factors. The effect of sedentary behaviours on these markers is independent of sociodemographic factors, diet, body mass index and PA.17 These findings are important, since they show that the effect of sedentary behaviours on these variables is not modulated by a higher caloric intake, but by a reduction in energy expenditure.17
As sedentarism is a learned behaviour of human beings that has increased exponentially during the 21st century, the risk factors or conditions that favour it are not yet known. However, various lines of research have identified the following general factors, particularly in younger individuals:32–35
- a.
Demographic: demographic factors include sex, age and ethnicity. Numerous publications show that women are less active than men and older children, and adolescents are less active than younger children. Among women, those of African descent are less active than Caucasians.
- b.
Personal: certain personal factors, such as underlying diseases (cardiovascular disease, diabetes, asthma, chronic orthopaedic diseases) or disability, predispose to sedentary behaviours due to the child's tendency to remain sedentary or to their preference for activities that demand less energy expenditure. Other factors include: self-perceived lack of time, inappropriate relationship with peers and an activity they find boring or unattractive. Individual factors that are positively associated with PA are: self-confidence to engage in exercise, personal ability, positive attitude towards PA, interest in self-improvement and ability to enjoy PA. Age is an important factor in this category, since research has revealed that children up to the age of 8engage in moderate to vigorous PA, but start to become less active from the age of 1136, making this a crucial period for PA interventions.
- c.
Family: this is perhaps the most important factor, since the preferences and habits of the parents will affect the extent to which the child is encouraged to engage in PA or certain motor activities. Watching TV is more influenced by the parents’ attitude towards this activity than by the number of TVs in the home. Other situations, such as both parents’ growing commitment to their jobs, and single-parent families, may affect the possibility of engaging in extracurricular PA.
- d.
Social and environmental: the lack of, or difficulty in accessing, green spaces and safe sports facilities in large cities, restrictions on supervision by qualified personnel, education budget limitations, changes in curricular priorities, impoverishment and civil insecurity are some of the many factors that discourage participation in and limit access to PA both during and out of school hours.
As mentioned above, our modern lifestyle reduces the time we spend doing PA. In fact, over the last decade, several studies have shown that excessive sitting time can increase the risk of death, irrespective of whether or not we do exercise.
A review published in 201237 used data from 2002 to 2011 to estimate the proportion of deaths attributable to the “chair effect” in the population of 54 countries, with the following results:
- –
More than 60% of people worldwide spend more than three hours a day sitting (the average in adults is 4.7hours/day).
- –
Sitting time is responsible for 3.8% of deaths (approximately 433,000 deaths/year).
- –
Among the territories studied, mortality due to sitting time was higher in countries from the Western Pacific region, followed by countries in Europe, the Eastern Mediterranean, America and Southeast Asia.
The authors calculated that reducing sitting time by about two hours (that is, 50%) would result in a 2.3% decrease in mortality (3 times less), although there is no conclusive proof of a causal relationship. Even a more modest reduction in sitting time, of 10% or half an hour a day, could have an immediate impact on all-cause mortality (0.6%) in the countries evaluated, and eliminating sitting time would increase life expectancy by 0.20 years in the countries studied.
In 2017, the “Termómetro del sedentarismo en España: Informe sobre la inactividad física y el sedentarismo en la población adulta española” [Thermometer of sedentary behaviour in Spain: Report on physical inactivity and sedentary behaviour in Spanish adults] published by the Fundación España Activa [Active Spain Foundation] and the Centro de Estudios del Deporte [Sports Studies Centre] of the Universidad Rey Juan Carlos38 showed an alarming upward trend:
- –
Physical inactivity is responsible for 13.4% (over 52,000) of deaths per year in Spain. This means that 6.6 people die every hour from this cause compared to 3.7 deaths reported in the meta-analysis carried out by Rezende et al.37
- –
Nearly half of all Spanish adults do not practise any sport and do not do any exercise or any other physically demanding activity in their spare time.
- –
The least qualified social classes (lower occupational category) are less active in their free time, while those with higher qualifications are less active during their working hours. In other words, the greater the economic development, the higher the level of sedentary behaviour, and, therefore, the greater the associated health risks.
Although sedentary behaviour affects all age groups, the extreme age groups are the most affected for the following reasons:13,15,16,39–41
- a.
Schoolchildren and adolescents: logically, due to the impact on health in adulthood, which increases the risk of obesity, DM2 and hypertension. Because of the size of this age group, more effort is obviously needed to ensure adequate levels of PA in all social classes.
- b.
Women are the most affected, since inactivity rate among women is 8% higher than in men. This gender gap has widened steadily over the 21st century, perhaps as a result of cultural norms, traditional roles, or lack of social and community support from an early age.
- c.
The elderly: as older people tend to be more physically inactive, the economic costs of inactivity are likely to increase notably and place a heavy burden on healthcare budgets. In a study conducted in Germany, the potential effects of interventions aimed at promoting PA in the over-65s compensated for the negative effect of ageing and reduced inactivity-related healthcare costs.41 In other words, this single action was doubly beneficial.
Cultural differences also affect levels of physical activity. An example of this is Switzerland, where the population is divided into three distinct language groups: French, Italian and German.42 An analysis of regional differences showed that the per capita burden of physical inactivity is nearly double in French and Italian speaking regions compared to the German speaking population, perhaps due to a higher prevalence of physical inactivity, higher per capita healthcare spending, and higher disease prevalence.
Of course, the foregoing is also true of the correlation between physical inactivity and social strata or the stage of development of the country. The higher the population density and the human development index (HDI), the greater the percentage of physical inactivity in the population. For example, estimates have shown that in low- and middle-income countries, individuals working in the white-collar industry compared to agriculture were 84% more likely to be physically inactive, and greater economic development in these countries brings about changes in their occupational structure, resulting in increased physical inactivity levels.43,44 Moreover, between 2001 and 2016, the percentage of inactivity in high-income countries (where sedentary behaviour is most harmful) increased from 31.6 to 36.8%. In the same period, inactivity in low-income countries remained at 16%.15
Conclusion and recommendationsSedentary behaviour is increasing rapidly in most countries, and is now a public health problem that will worsen over the coming years. An analysis of the time spent doing PA in five major countries (China, the USA, the United Kingdom, Brazil and India) showed a significant decrease compared to previous years, and this downward trend is expected to increase in the future.45 In the USA, for example, the average sitting time increased from 26hours per week in 1965 to 38hours per week in 2009, and from 30hours per week in 1960 to 42hours per week in 2005 in the United Kingdom.
Although public policies and research into PA are much more developed today than they were decades ago, strategies to change sedentary behaviour are timid and only just emerging, and little progress has been made in recent years.
The universal recommendation is for adults to engage in moderate-intensity PA for 30minutes per day, preferably most days of the week46, although “usual” PA has now been included as a strategy to reduce sedentary behaviour3,9,16,46.
In view of the benefits of PA, physicians should recommend a minimum level of daily exercise. Even a low level of PA, if strenuous, can also be beneficial in reducing cardiovascular risk, especially for those with risk factors or a history of vascular disease. The following are just some of the recommendations published by working groups engaged in promoting PA, both individually and at the community level3,9,16,46:
- a.
Organise large-scale, intensive campaigns in prominent locations in the community.
- b.
Encourage people to use the stairs instead of lifts or escalators.
- c.
Promote physical education/sports in schools and universities.
- d.
Organise social activities (such as walking groups).
- e.
Introduce individually-tailored behavioural change programmes; specifically, limit recreational screen time in children and adolescents.
- f.
Facilitate access to locations suitable for PA.
- g.
Motivate people to reduce sitting time to two hours or less, with active pauses every hour and short stretching sessions or walks.
In summary, in the fight against sedentary behaviour, remember that: “A little PA is better than none. More PA is better than less PA”, and that doctors are under the obligation of setting an example in their community by living a more active, healthier lifestyle, and “walking their talk”.
FundingNone.
Conflicts of interestThe author declares that this review has received no commercial or financial contributions that could represent a potential conflict of interest.