Statins are the first line of treatment in patients with severe hypercholesterolemia (SH). However, despite the knowledge regarding its effectiveness and security for preventing cardiovascular diseases, treatment is a major challenge.
Material and methodsA prospective observational study was conducted by telephone survey to determine cardiovascular risk factors, annual monitoring, statins use and persistence and new-onset cardiovascular events (CVE) after 5 years in patients with HS including in a programme for detection of familial hypercholesterolemia.
Results115 participants were analysed, the median age was 56 ± 10 being 74% females. 63.4% of women and 43% of men had been correctly controlled in the last year. Patients on lipid lowering drugs stratified by sex was 38.8% in women and 26.7% in men, however, only 22 participants (31.8%) were persistence with statins since 2015.Overall, 48% of the patients presented a CVE and 3.4% died. Multivariate analysis did not reveal predictors for CVE.
ConclusionsIn our population with SH we found a high risk to present a CVE and a dramatic low use and persistence with the treatment.
Las estatinas son la primera línea de tratamiento en pacientes con hipercolesterolemia severa (HS). A pesar de la evidencia disponible sobre su eficacia y seguridad para prevenir eventos cardiovasculares, el correcto tratamiento sigue siendo un desafío.
Materiales y métodosEstudio observacional prospectivo diseñado para determinar mediante entrevista telefónica la presencia de factores de riesgo, seguimiento clínico anual, persistencia/uso de estatinas y aparición de nuevos eventos cardiovasculares (ECV) después de 5 años, en pacientes con HS incluidos en un programa de Detección de Hipercolesterolemia Familiar.
ResultadosSe evaluaron 115 participantes, la edad media fue de 56 ± 10 siendo el 74% mujeres. El 63.4% de las mujeres y el 43% de los hombres refirió estar bajo seguimiento y control clínico en el último año. El 38.8% de las mujeres recibió estatinas versus el 26.7% de los hombres, y, solo 22 participantes (31.8%) fueron persistentes con el tratamiento desde 2015. El 15.5% de los participantes presentó un ECV no fatal y el 3.4% fatal. En el análisis multivariado no se detectaron predictores para presentar un ECV.
ConclusionesEn nuestra población con HS encontramos un alto riesgo de presentar un ECV y una dramática baja tasa de uso y persistencia al tratamiento con estatinas.
Hypercholesterolaemia specifically related to increased levels of LDL-cholesterol (LDL-C) is one of the most relevant risk factors for atherosclerotic cardiovascular disease. In Argentina, there is an estimated self-reported prevalence of hypercholesterolaemia of 28% in the adult population.1 Severe hypercholesterolaemia (SH) is considered when LDL-C levels exceed 190 mg/dl, a condition that requires the initiation of intensive pharmacological treatment, and familial hypercholesterolaemia (FH) – a common genetic disease that is underdiagnosed and undertreated – should be considered a potential causal factor.
Statins are the cornerstone in the prevention of atherosclerotic cardiovascular disease, both primary and secondary prevention. They have been shown to reduce mortality and cardiovascular events in several clinical settings and are the first-line indication for patients with SH.2 However, despite all the available evidence regarding their safety and efficacy, most patients are not medicated. This situation is observed not only in primary, but also in secondary prevention and even in high resource countries. The PURE study reported examples of this problem which, in secondary prevention, found that only 66.5% of patients were treated with statins in high per capita income countries as opposed to 3% in low-income countries.3 Furthermore, most patients on treatment do not meet the targets provided in current guideline recommendations. Different studies have shown, for various reasons, how difficult it is to meet the targets in secondary prevention or high CV risk patients. As an example of this situation, the recent EUROASPIRE V study reports that only about 1/3 of patients in secondary prevention reach LDL-C targets.4 The DA Vinci study, referring to patients with SH in Argentina, shows similar results in terms of reaching this lipid target.5
The effectiveness of statins is mainly impaired by low adherence and suboptimal treatment.2 Adherence to lipid-lowering drugs has been shown to fall dramatically during the first year of treatment.6 This adherence failure, together with the low rate of statin use, is a major problem in both primary and secondary prevention, making it imperative that health policies are implemented to improve the long-term use of statins, as cost-effective medication with extensive evidence and a well-proven safety profile.7
The purpose and main objective of this study was to assess the presence of risk factors, clinical follow-up, statin use and new cardiovascular events in patients diagnosed with SH in a region of Argentina within the public health system.
Materials and methodsType of design and study populationThis is a prospective observational study. During the second half of 2020, we conducted telephone follow-up of a subgroup of 115 randomly selected participants with SH, who were included in the Familial Hypercholesterolaemia Detection Programme in Argentina (DA VINCI study) during 2015, which was undertaken in the district of General Pueyrredón, Buenos Aires, Argentina.8
The participants included in the DA VINCI study attended a public health centre and were admitted because they presented total cholesterol greater than 300 mg/dl or LDL-C greater than 190 mg/dl on biochemical analysis. At the start of the screening programme, each participant was asked about their personal and family history of cardiovascular disease, the presence of cardiovascular risk factors, and lipid-lowering medication received. In addition, a complete physical examination was performed, looking for tendinous xanthomas and corneal arcus (stigmata of FH). The Dutch Lipid Clinic Network (DLCN) score was used to clinically diagnose FH, after collecting each of the items corresponding to this score. Standardised enzymatic methods under internal and external quality control were used to determine total cholesterol, triglyceride, LDL-C and HDL-C (HDL-C) levels. Secondary causes of hypercholesterolaemia were ruled out by measuring TSH, creatinine, liver enzymes, and blood glucose.
All the participants enrolled in the study were given a final report written by medical and biochemical professionals for their primary care physician with the final assessment and recommendation for the lipid-lowering treatment to be initiated according to the guidelines of the European Society of Cardiology based on the result of their clinical assessment and biochemical analysis. 9 The patients were also given a report explaining their disease and follow-up to ensure good adherence and continuity of treatment. The contact details of the patient and 2 direct relatives were taken to ensure correct follow-up. All participants gave their informed consent prior to their assessment and agreed to participate in the programme and follow-up. The study was approved by the ethics committee (Res CD 4705/14).8
Study variablesDuring the follow-up telephone interview, the patient's clinical monitoring over the last 12 months was assessed, taking the number of visits to the medical centre and blood tests into account. The presence of cardiovascular risk factors (hypertension, sedentary lifestyle, smoking, diabetes), pre-existing cardiovascular disease, adherence to treatment, and the presence of new cardiovascular events were reassessed. Hypertensive participants were defined as those who reported being treated with antihypertensive drugs and diabetic participants were defined as those who reported being treated with insulin or oral antidiabetic drugs. Sedentary lifestyle was defined as a lack of regular physical activity: less than 30 min of regular exercise per day and less than 3 days per week. Participants who smoked at least one cigarette daily at the time of the survey were considered smokers. We asked for the name of the lipid-lowering drug, the dose and daily intake of the drug to assess the use of statins. Statin use was considered positive when the respondent answered that they took the medication daily and negative when they reported complete discontinuation of the medication or sporadic or intermittent intake. Participants who at the start of the study (2015) were already on daily statin medication and reported continuing to take it daily up to the time of the interview were considered persistent.10 Cardiovascular events were defined according to self-reported admission to hospital or a revascularisation procedure for ischaemic heart disease, admission to hospital for stroke, for heart failure, for a peripheral revascularisation procedure (bypass or endovascular); events that occurred after recruitment in 2015. A death event was defined by verbal autopsy on the immediate family member contacted.
Statistical analysisCategorical data are presented as total number of participants and percentages (n [%]). Continuous data are shown using the mean for central tendency and standard deviation for dispersion in cases of normal distribution (mean ± standard deviation). In the case of non-normally distributed continuous data, median for central tendency and percentiles for dispersion (p25-p75) were used as summary measures. Categorical variables were analysed using χ2 with Fisher's correction, when necessary, with differences with a p-value of less than .05 considered significant. Numerical variables with normal distribution were analysed using the Student’s t-test. Predictors of cardiovascular events with statistical significance in the bivariate analysis were adjusted for age and sex by logistic regression method. STATA 11 software (Stata Corp., College Station, TX, USA) was used for statistical analysis of the data).
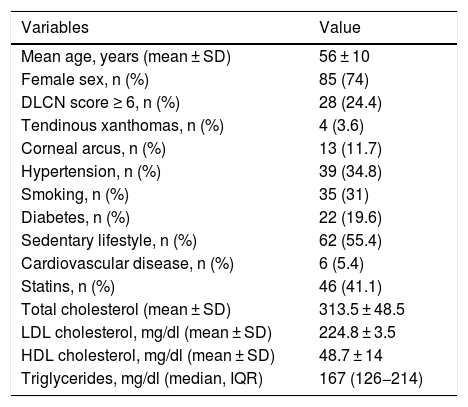
ResultsThe total patient sample comprised 115 participants with a diagnosis of SH. Table 1 shows the demographic (mean age, sex), clinical (DLCN score, presence of tendinous xanthomas, corneal arcus, arterial hypertension, smoking, diabetes, sedentary lifestyle, and presence of pre-existing cardiovascular disease), the use of statins, and lipid values of this subgroup recruited in 2015. The average age of participants was 56 years, and 74% were female. Forty-two participants (36.5%) presented at least one modifiable cardiovascular risk factor (diabetes, smoking, hypertension, or HDL-C below 40 mg/dl in men and 50 mg/dl in women) and 33 (28.7%) had at least 2 risk factors.
Demographic and clinical characteristics, and lipid levels of patients at the start of the study (2015).
| Variables | Value |
|---|---|
| Mean age, years (mean ± SD) | 56 ± 10 |
| Female sex, n (%) | 85 (74) |
| DLCN score ≥ 6, n (%) | 28 (24.4) |
| Tendinous xanthomas, n (%) | 4 (3.6) |
| Corneal arcus, n (%) | 13 (11.7) |
| Hypertension, n (%) | 39 (34.8) |
| Smoking, n (%) | 35 (31) |
| Diabetes, n (%) | 22 (19.6) |
| Sedentary lifestyle, n (%) | 62 (55.4) |
| Cardiovascular disease, n (%) | 6 (5.4) |
| Statins, n (%) | 46 (41.1) |
| Total cholesterol (mean ± SD) | 313.5 ± 48.5 |
| LDL cholesterol, mg/dl (mean ± SD) | 224.8 ± 3.5 |
| HDL cholesterol, mg/dl (mean ± SD) | 48.7 ± 14 |
| Triglycerides, mg/dl (median, IQR) | 167 (126−214) |
DLCN: Dutch Lipid Clinic Network score; HDL-C: HDL cholesterol; IQR: Interquartile Range; LDL-C: LDL cholesterol; SD: Standard Deviation.
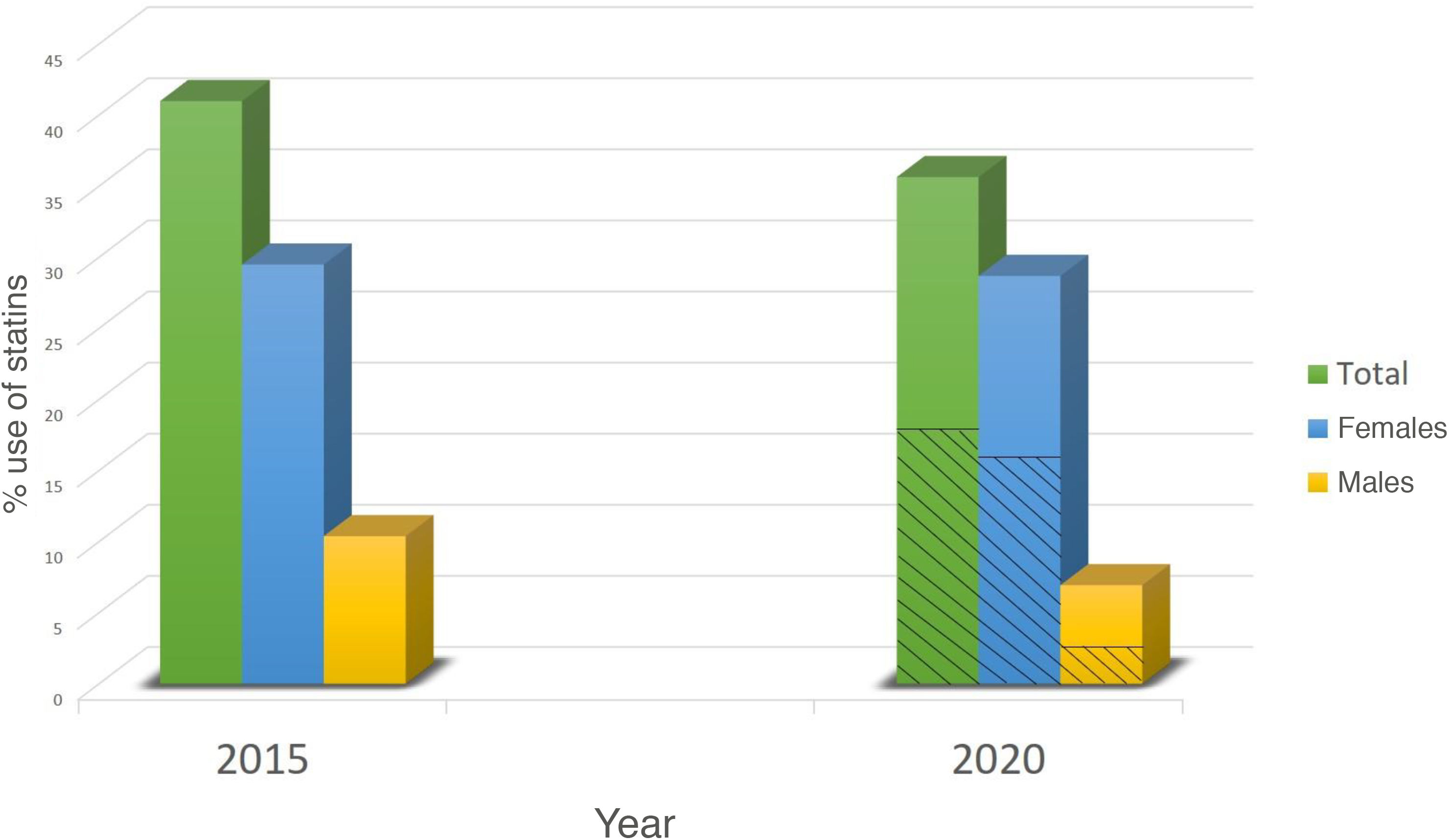
During the interview undertaken in 2020, 52 women (63.4%) and 13 men (43%) reported being under follow-up and having had clinical monitoring in the last year; this gender difference was at the limit of statistical significance (p = .057). Although at the start of the study (2015), 46 participants (41%) were receiving daily statin medication, only 19 (34.7%) of them reported continuing with it at 5 years; these participants were considered persistent. We found no difference in statin persistence between the 28 participants with a DLCN score ≥ 6 (criteria for probable FH) and participants with a score of less than 6. However, of the 69 participants who were not receiving medication in 2015 and who were counselled to start medication, only 22 participants (31.8%) reported currently taking daily statin medication. Stratified by sex, overall, 33 women (38.8%) reported receiving statins vs. 8 men (26.7%) in 2020, p = .187 (Fig. 1). The reported or detected reasons for not starting medication or for discontinuing medication were not receiving adequate monitoring 65%, not being prescribed by the GP 16%, difficulty in accessing the health centre to obtain the medication 13%, myalgias 4%, and personal reasons 2%.
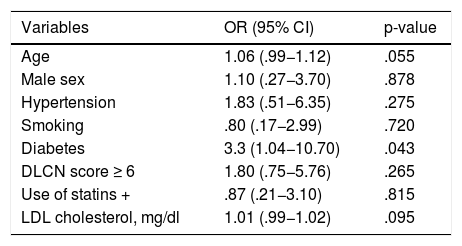
During the period of assessment (2015–2020), 18 participants (15.5%) reported admission to hospital for cardiovascular disease (ischaemic heart disease, heart failure, peripheral vascular disease, or ischaemic stroke) and 4 participants (3.4%) died during follow-up due to ischaemic heart disease. None of the 19 persistent participants had cardiovascular events, in contrast, 3 participants (12%) of the 25 non-persistent participants did have events (p = .12). Finally, we found a statistically significant association between having diabetes and the risk of having a cardiovascular event. The odds ratio in patients with diabetes was 3.3 (95% confidence interval 1.04−10.70), with a p-value of .043 (Table 2). However, this association lost statistical significance when adjusting for age and sex (p = .082).
Univariate analysis of predictors for cardiovascular events.
| Variables | OR (95% CI) | p-value |
|---|---|---|
| Age | 1.06 (.99−1.12) | .055 |
| Male sex | 1.10 (.27−3.70) | .878 |
| Hypertension | 1.83 (.51−6.35) | .275 |
| Smoking | .80 (.17−2.99) | .720 |
| Diabetes | 3.3 (1.04−10.70) | .043 |
| DLCN score ≥ 6 | 1.80 (.75−5.76) | .265 |
| Use of statins + | .87 (.21−3.10) | .815 |
| LDL cholesterol, mg/dl | 1.01 (.99−1.02) | .095 |
CI: Confidence Interval; DLCN: Dutch Lipid Clinic Network score; LDL-C: LDL cholesterol; OR: odds ratio.
The present study shows a prospective approach in a group of patients with SH, with no secondary causes, with indication for statin treatment, in a population belonging to the public health system of a region of the Province of Buenos Aires that to date has not been studied in our country. After 5 years of follow-up, we observed a low percentage of statin persistence and use, and a high incidence of cardiovascular events commensurate with undertreatment, even though the diagnosis of SH and the therapeutic recommendation were correctly made in this population.
The results of this study show a high proportion (64.3%) of participants at extreme risk for cardiovascular disease who are not adequately monitored and are not receiving lipid-lowering medication. These figures are slightly higher than those reported in previous studies in other parts of the world, where approximately 50% of the candidate patients in the SH population were not receiving statins and, due to this lack of medication in follow-up, had increased cardiovascular risk.11 Moreover, when we analysed the 28 participants with probable FH, we found that only 37% were persistent with statin use at 5 years. In the population diagnosed with FH, there is little published data on adherence to lipid-lowering medication, indicating a radically opposite percentage to that observed in our study; in the CASCADE-HF study, only 25% of patients were not receiving statins, and approximately 15% were not given them due to statin intolerance or allergy.12
In our population, most of the reasons reported for discontinuing medication were financial or a failure in follow-up or treatment behaviour on the part of the primary care physician. The latter situation was potentially aggravated by the COVID-19 pandemic in 2020, partly due to fear of attending the medical establishment for monitoring and due to the reduction or discontinuation of outpatient consultations that affected the public system as it reorganised to meet the demands of the pandemic.13
Regarding cardiovascular events, there are no follow-up cohorts of patients with SH. Taking follow-up data into account from population-based cohorts with FH, the Spanish SAFEHEART registry has reported a 5-year incidence of a non-fatal cardiovascular event in 5.1% of subjects and fatal cardiovascular events in .5%.14 Independent predictors of risk in this population were age, male sex, presence of hypertension, obesity, smoking, LDL-C and lipoprotein levels (a).14 In our SH population we detected a surprisingly higher number of cardiovascular events; 15% of non-fatal cardiovascular events and 3.4% of fatal cardiovascular events. These differences could be explained by low statin use (40% in our population vs. 84.2% in the SAFEHEART population) and our participants had increased baseline cardiovascular risk because of a higher prevalence of diabetes.14 Also, compared to national data, our subgroup had a higher prevalence of diabetes (19% vs. 12%), higher smoking (33% vs. 24%), and sedentary lifestyle (55% vs. 44%).1
There is a national programme of the Argentinian Ministry of Health that seeks to provide essential medicines (based on World Health Organisation recommendations) to the country's public primary healthcare centres (CAPS).15 These essential drugs include treatment for the prevention and management of cardiovascular diseases, and currently include simvastatin 20 mg and rosuvastatin 20 mg. Despite the availability of these drugs, training in the use of medicines and supplies distributed by the Drugs Programmes and Projects Coordination and Rational Therapeutics Training Programmes in Primary Health Care (TRAPS), multiple barriers have resulted in the ongoing inappropriate management of patients with hypercholesterolemia. These barriers include organisational problems with the distribution of medication to the CAPS, the low degree of compliance with the proposed regulations to guide the general practitioner in prescribing medication, errors or omissions by primary care physicians, communication problems with the patient, and lack of time in the consultation.
We should first mention as a limitation of this study that, as it was conducted in the public sector and in a specific region, the sample selected in the cross-section is not representative of the general population. Secondly, we mentioned that the data collected on taking medication, because we used an indirect method (interview), are dependent on the patient's answers and intentions. Another limitation is that we were not able to analyse the last LDL-C value in the participants followed up in 2020 because most did not have the final results. As for the events reported, although they were collected by self-report or family interview in the case of deceased participants, only hard events (hospitalisation, revascularisation, death) were considered, reducing the possibility of false positives. Finally, given the small sample size, we did not have sufficient power to find statistically significant predictors in the multivariate analysis for cardiovascular events. Nevertheless, it does alert us to the real situation of a highly vulnerable sector of the population, which is important information for adopting more specific health behaviours.
ConclusionThe data from follow-up of this series of patients with SH, which includes patients with a clinical diagnosis of FH, show the low use of lipid-lowering treatment in the public sector in Argentina, mostly due to a lack of control, prescribing, and medical follow-up. However, from this finding, we can observe the higher incidence of fatal and non-fatal cardiovascular events compared to other cohorts of patients with similar characteristics in other countries. Although statins have been included as essential medicines and are provided free of charge in the CAPS, there are still many cultural, organisational, socio-economic, and educational barriers that are impeding the correct treatment of this population at high cardiovascular risk.
FundingNo specific grants from agencies in the public, commercial or non-profit sectors were received for this study.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Facundo Blautzik, Rodrigo Cardoso, Macarena Sanchez Pardo, and Facundo Sampayo, of the University FASTA Mar del Plata, for their collaboration in setting up the database.
Please cite this article as: Matta MG, Saenz B, Schreier L, Corral A, Sarobe A, Corrall P. Estudio prospectivo sobre uso y persistencia de tratamiento hipolipidemiante en pacientes con hipercolesterolemia severa. Clin Investig Arterioscler. 2021;33:308–313.