Edited by:
José Antonio Sainz Bueno
Professor of Obstetrics and Gynecology, Faculty of Medicine, University of Seville, Seville, Spain Professor of Obstetrics and Gynecology, Faculty of Medicine, University of Seville, Seville, Spain Professor of Obstetrics and Gynecology, Faculty of Medicine, University of Seville, Seville, Spain Professor of Obstetrics and Gynecology, Faculty of Medicine, University of Seville, Seville, Spain Professor of Obstetrics and Gynecology, Faculty of Medicine, University of Seville, Seville, Spain
Eugenia Antolín Alvarado
Senior Consultant in Fetal Medicine, Department of Obstetrics and Ginecology, University La Paz Hospital; Member of the Obstetric Group in IdiPAZ- Biomedical Research Institute; Member of the SAMID network, Associate professor UAM University, Madrid, Spain
The introduction of ultrasound into the delivery room is a challenge in our speciality. Imaging techniques are increasingly used in obstetrics, and we are familiar with ultrasound management and the study of pelvic and foetal structures. Ultrasound has been introduced into the study of labour for decades, with a large number of high quality research papers published in the literature. Various approaches and measurements have been described, and there are parameters that have been shown to have high evidence of intrapartum usefulness, such as assessment of foetal head position. Furthermore, the inaccuracy and subjectivity of the traditional evaluation of labour progress by digital vaginal examination has been demonstrated. All this leads us to support the promotion and implementation of this ultrasound to complement our knowledge and decision-making in delivery. The aim of this review is to describe the appropriate method for this ultrasound evaluation and its main applications in labour.
La introducción de la ecografía en la sala de partos supone un reto en nuestra especialidad. Las técnicas de imagen son cada vez más utilizadas en obstetricia, y estamos familiarizados con el manejo ecográfico y el estudio de las estructuras pélvicas y fetales. El ultrasonido se ha introducido en el estudio del trabajo de parto durante décadas, con una gran cantidad de artículos de investigación de alta calidad publicados en la literatura. Se han descrito varios enfoques y mediciones, y hay parámetros que han demostrado tener una alta evidencia de utilidad intraparto, como la evaluación de la posición de la cabeza fetal. Además, se ha demostrado la inexactitud y subjetividad de la evaluación tradicional del progreso del parto mediante examen vaginal digital. Todo esto nos lleva a apoyar la promoción e implementación de esta ecografía para complementar nuestro conocimiento y toma de decisiones en el parto. El objetivo de esta revisión es describir el método adecuado para esta evaluación ecográfica y sus principales aplicaciones en el parto.
Fundamental to the correct management of labour is an understanding of the processes of foetal head engagement, descent, rotation, and flexion. Malposition and/or malpresentation of the foetal head, such as a persistent occiput posterior or transverse position, an excessive foetal head deflection, as well as marked asynclitism, lack of engagement, or a combination of several of these factors can lead to dystocia. All of them are associated with an increased risk of instrumental delivery and increased maternal and neonatal morbidity. In addition, knowledge of foetal head position and station is essential for the correct use of forceps or vacuum extraction. The inability to do so increases the failure rate of the procedure, with sequential application of diverse instruments or subsequent caesarean section. Secondarily, the risk of maternal and neonatal injury may be increased by prolonging the time to delivery.1–3
Assessment of labour progress has traditionally been performed by transvaginal digital palpation, but this has been shown to be inaccurate and subjective (high inter-observer variability), particularly in identifying the position of the foetal head and determining the degree of engagement. Furthermore, this error is exacerbated in abnormal foetal head positions (occiput transverse or posterior) and in the presence of caput succedaneum and asynclitism.4,5
Our expertise with ultrasound has led us to extend its use to the delivery room as it does not require complex technology, using standard convex probes to perform foetal biometry at the bedside. It has proved to be easy to use, painless and reproducible. It also requires no special training once the anatomical landmarks relating to the foetal head and pelvis are known and learnt to identify. In addition, it has been shown to be useful in determining the position of the foetal head, the degree of engagement, and in the diagnosis of foetal malposition and malpresentation.6 Nevertheless, the information obtained by classic digital vaginal examination remains indispensable and intrapartum ultrasound should continue to be complementary to it. These data provide greater accuracy and help us to assess the progress of labour, which is particularly useful in prolonged labour and increases the success rate of vaginal delivery by preventing dystocia.
TechniqueIntrapartum ultrasound must be performed using a combination of transabdominal (TA) and transperineal or translabial (TP) ultrasound, using a two-dimensional convex probe, with wide insonation and low frequencies. The pregnant woman should be in the supine decubitus position and the bladder must be empty. The different measurements can be estimated at rest, during contractions or when the mother is actively pushing.
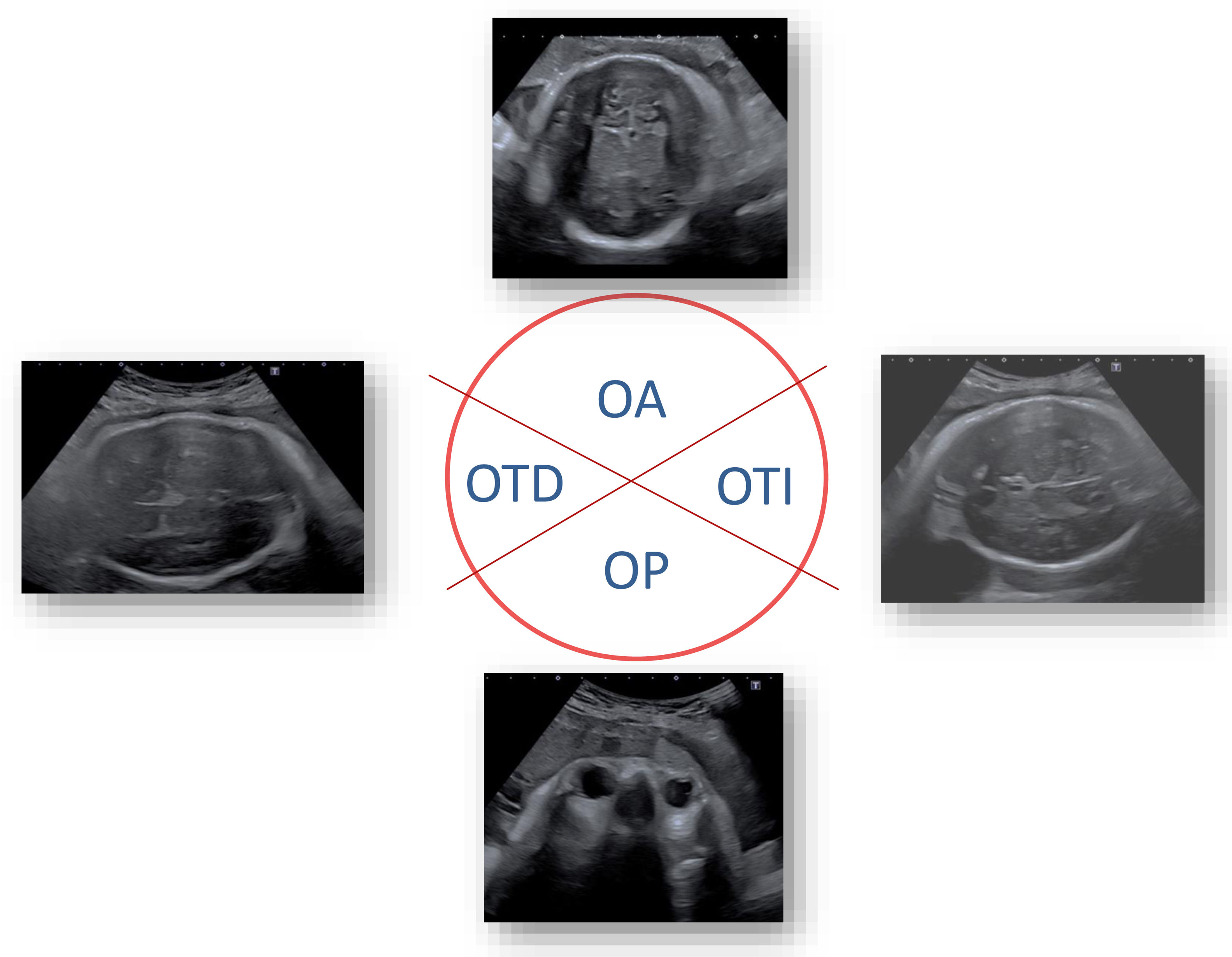
Transabdominal assessmentA cross-section of the maternal suprapubic region (Fig. 1) is acquired to determine the position of the head in relation to the maternal pelvis and to identify foetal brain structures and the midline of the head.7 To describe the position of the foetal head, we compare it to the horary sphere: occiput anterior (OA) position between ≥10:00 and ≤2:00, occiput posterior (OP) between ≥4:00 and ≤8:00, and occiput transverse (OT) between >2:00 and <4:00 or <8:00 and >10:00 (Fig. 2). We can also be on the lookout for head synclitism if none of the parietals precede the sagittal suture in the birth canal.
Representation of the position of the foetal head with respect to the clockwise axis13,21,22. OA: occiput anterior; OTD: right occiput transverse; OTI: left occiput transverse; OP: occiput posterior.
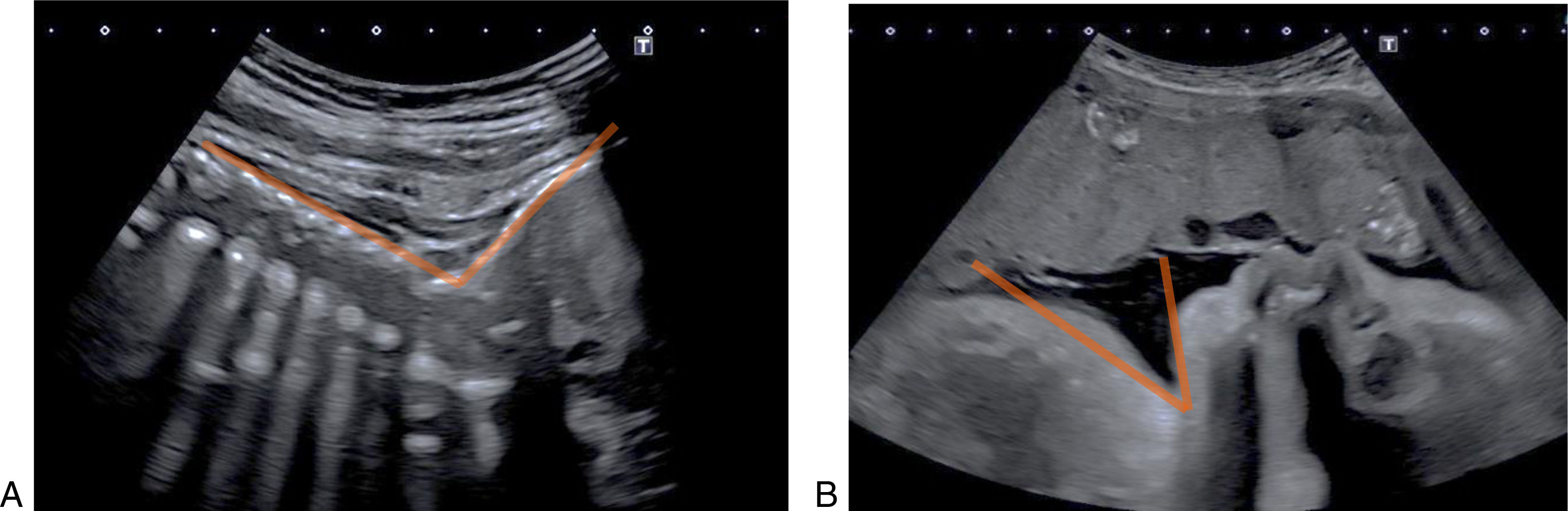
The longitudinal section (Fig. 1) is captured to assess the foetal lie (longitudinal, oblique, transverse) and the degree of head flexion (attitude). In OA and OT foetuses, we measure the relationship between a line tangential to the occiput and another tangential to the foetal spine by means of the occiput–spinal angle (Fig. 3),8 whose increase is associated with progressive head flexion and descent to lower pelvic stations. This angle is not well measured in OP foetuses due to the shadowing of the craniofacial bones in this area, so to determine flexion in these, a sagittal section of the head and thorax is made via the transabdominal approach. This allows the relationship between the chin and thorax to be assessed; the chin is close when the head is flexed, but moves away from the thorax and the cervical spine curves anteriorly when deflexion occurs. This is objectified by the chin–chest angle,9 which is drawn between a line that passes through the long axis of the sternum, and a second line drawn through the skin overlying the lower border of the oral cavity and the chin. The wider the angle, the greater the deflection of the head.
Finally, the suprapubic descent angle10 measures the degree of head engagement via the transabdominal approach. It represents the angle between a longitudinal line across the pubic symphysis and another line from the top of the symphysis tangential to the top of the foetal skull. This measure correlates well with the angle of progression (transperineal approach).
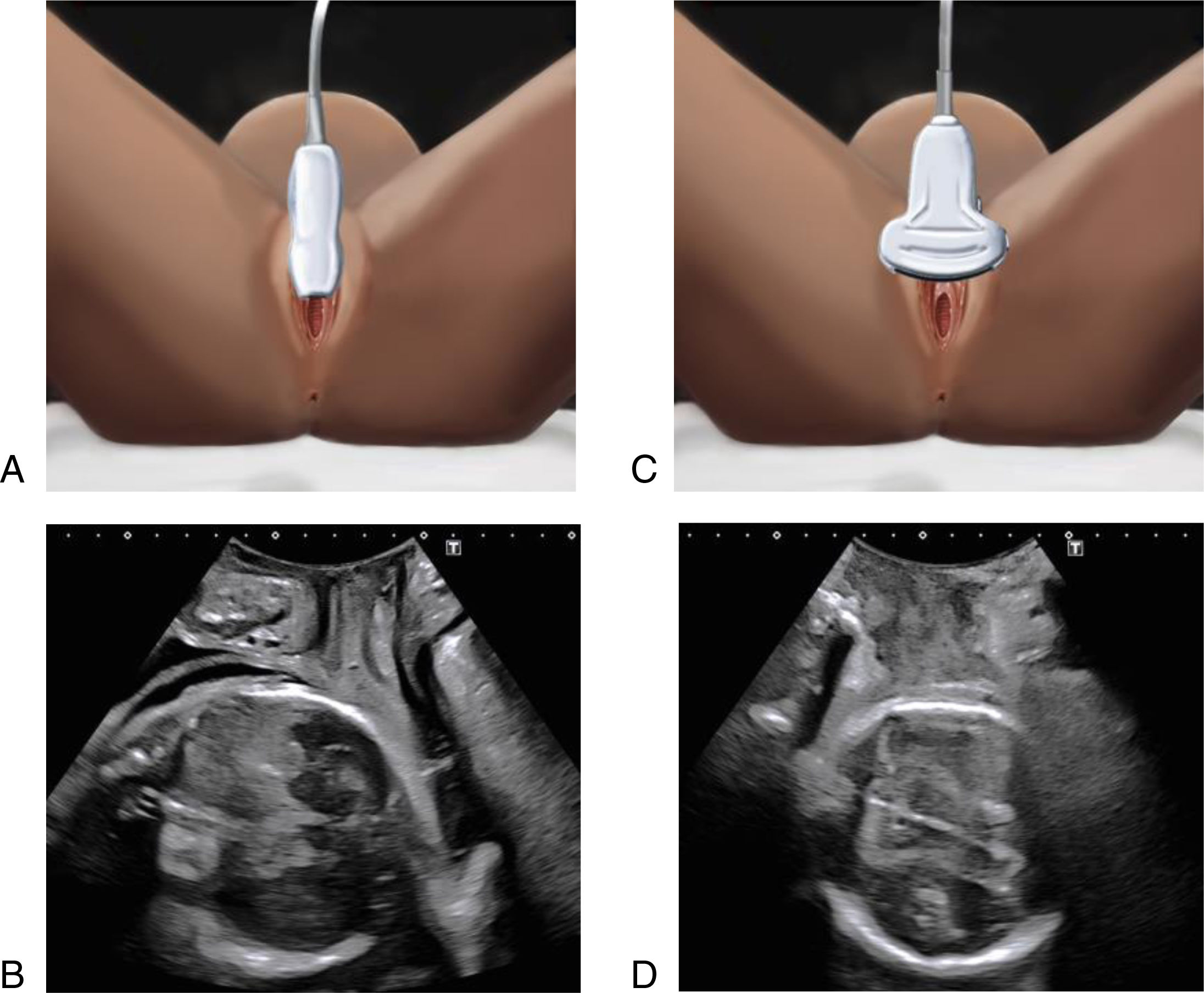
Transperineal assessmentThe transperineal approach is based on placing the probe on the perineum between the labia vulvae, protected by a sheath. By consensus, usually the dorsocaudal plane is placed on the right and the cranioventral plane on the left of the screen. A longitudinal or transverse plane may be obtained depending on the placement of the probe. Many measurements between the pelvic structures and the head have been described, but we will only mention those that have the greatest impact.
In the longitudinal or mid-sagittal plane (Fig. 4), starting from the position described above, we gently move the transducer upwards to obtain an image of the long axis of the pubic symphysis and the outline of the foetal skull. This imaginary line, which relates the pubic symphysis to the contour of the foetal head, can provide various measurements of the progress of labour and the position of the head (foetal head station).
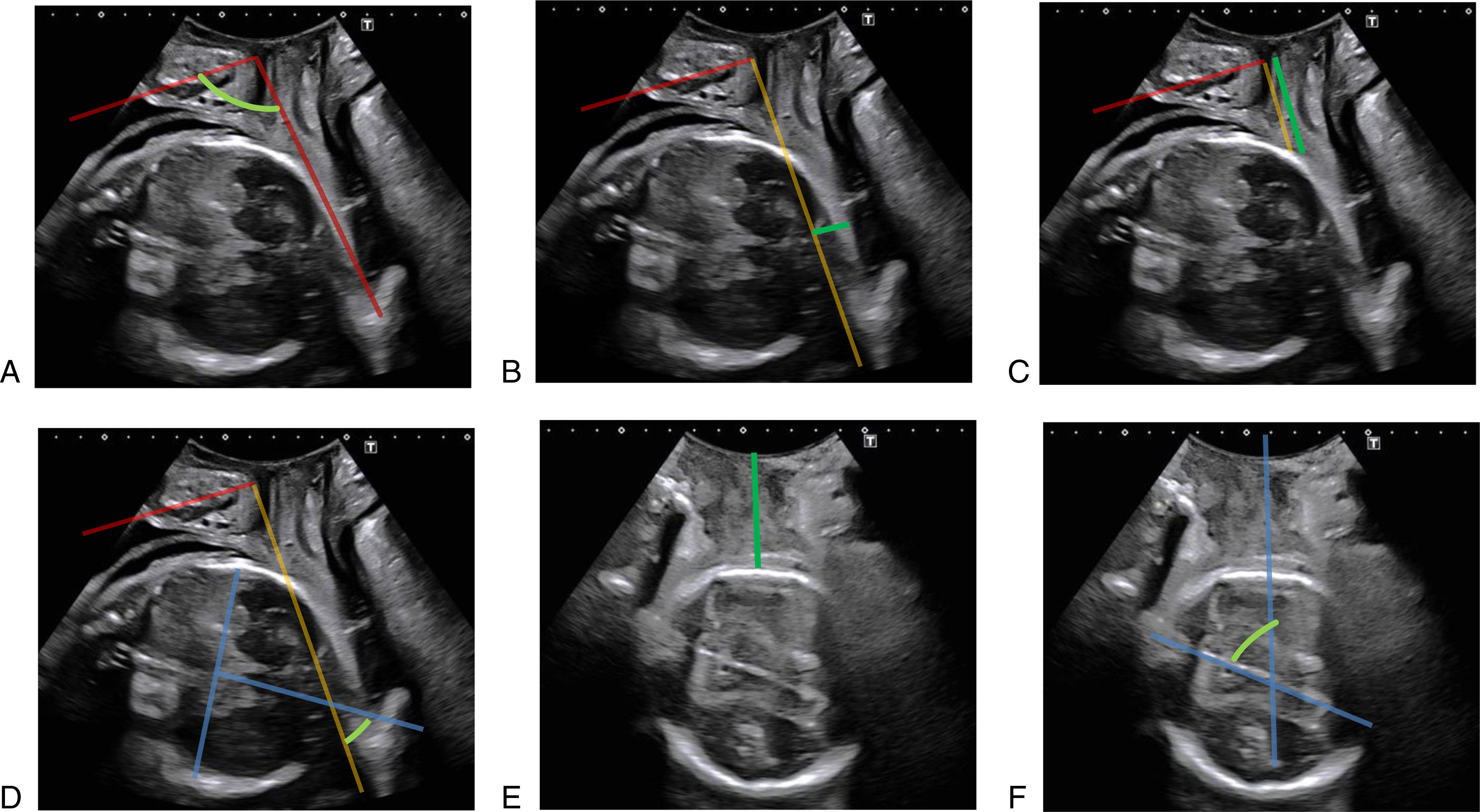
The most commonly used measurement is the angle of progression (AoP), which has been shown to be reproducible and easy to learn.11 It is measured by drawing a line along the long axis of the pubic symphysis and another line from the lowest edge of the pubic symphysis tangentially to the contour of the foetal head at its lowest point, and calculating the angle between them (Fig. 5). The greater the AoP, the greater the descent of the foetal head.
Main ultrasound measurements in transperineal ultrasound approach. (A) Angle of progression; (B) distance of progression, (C) head–symphysis-distance; (D) head direction; (E) head–perineum distance; (F) midline angle. In red: long axis of the pubic symphysis; in orange, infrapubic line; in green the main measurements.
Furthermore, the progression distance12 draws a line perpendicular to the aforementioned long axis of the pubic symphysis, called the infrapubic line, to which we relate the foetal head by measuring the distance in millimetres from this line to the most advanced part of the presentation, making the perpendicular measurement (Fig. 5), which may be cranial or distal to it. In addition, the head–symphysis distance12 is simple and reproducible, measuring the shortest distance from the infero-external edge of the pubic symphysis to the foetal head, following the infrapubic line described above (the shorter the distance, the more favourable the progression) (Fig. 5).
The direction of the head is more complex to assess.12 It relates the infrapubic line to a second line perpendicular to the biparietal diameter (Fig. 5). If the angle between the two lines is equal to or greater than 30°, it is described as “upward” (and is associated with a favourable outcome), between 0 and 30° as indifferent, and equal to or less than 0° as “downward” (and is associated with a higher risk of caesarean section).
In the transverse or coronal plane (Fig. 4), also with the transperineal probe, a 90° rotation is made from the longitudinal plane in order to evaluate the outline of the foetal head. The measurement of the head–perineum distance12 assesses the smallest distance in millimetres from the external perineal surface (corresponding to the area where the transducer is placed, without pressure) to the foetal head (Fig. 6).
This measure correlates with the foetal head station; the greater the distance, the smaller the station, with a measurement of 35mm associated with head engagement (station 0).13 The midline angle assesses the degree of rotation of the foetal head,14 but requires identification of the encephalic midline, as it is the angle drawn between this line and the antero-posterior axis of the maternal pelvis (Fig. 6). Angles less than 45° are associated with rotation of the head towards the OA or OP, so it is important to correlate this with position.
Practical application of intrapartum ultrasound: assessment of fetal head malposition and malpresentationThe incidence of malposition and malpresentation is not well defined, but it is a cause of difficulty in the progress of labour and is associated with increased operative deliveries and foetal and maternal morbidity, so it is important to identify it correctly. In addition, there are sometimes multiple coexisting factors associated with malpresentation that can complicate diagnosis and outcomes.
The use of intrapartum ultrasound to objectively diagnose asynclitism could predict the slow progress of labour, assess the risk of instrumental delivery and reduce the incidence of maternal and foetal morbidity and mortality.15,16 Labour dystocia has been observed in 40% of deliveries, and early recognition of foetal head malposition and malrotation is of paramount importance, especially in dystocia. The clinical diagnosis of asynclitism is made by vaginal palpation and is often erroneous due to its subjective nature and the presence of caput succedaneum, which makes palpation of the sutures more challenging.16,17 Evidence suggests that intrapartum ultrasound may help to improve the accuracy of vaginal palpation in dystocia, thereby improving maternal and foetal outcomes.16
In terms of malposition, 16.5% of occiput posterior (OP) and 5.5% of occiput transverse (OT) malpositions have been reported in primigravidae in the second stage of labour.18 Intrapartum ultrasound diagnosis by suprapubic transabdominal assessment confirms OP position, with foetal orbits upwards, and OT, with assessment of the midline of the brain and occiput. In addition, transperineal assessment in the coronal section shows the degree of rotation of the foetal head, confirming OT, with an angle close to 90°. The accuracy of this technique for diagnosing position has a high level of evidence,19 whereas digital palpation has been associated with a high rate of diagnostic error. Furthermore, persistent position in the OP and OT with advanced expulsion is more difficult to diagnose because of the frequent association with caput succedaneum.
In cephalic presentation, the abnormal position of the foetus at birth or malpresentation due to altered flexion of the foetal head varies according to the degree of flexion of the synciput, forehead and face. It is a well-known cause of dystocia, but clinical diagnosis is difficult and imprecise, so its prevalence is poorly reported.
For ultrasound diagnosis, in foetuses in OA and OT positions, the relationship between the spine and occiput is assessed longitudinally transabdominally with OSA (Fig. 3). Measurements of less than 125° have been associated with deflexion, prolonged labour and a higher incidence of caesarean section.18 In the OP position, flexion is assessed by longitudinal transabdominal evaluation of the relationship between the foetal chest and chin, using the chin–chest angle (Fig. 3). The transperineal approach is also useful, using a sagittal section to examine the structures visualised below the pubic symphysis, checking that the orbits are at the same level as the pubis (greater deflection, frontal presentation). The OP position is strongly associated with deflexion in a prolonged second stage of labour in primiparous20 and is more associated with caesarean section than in those positions without deflexion.
Another abnormal presentation is asynclitism, as the midline of the sagittal suture of the foetal head deviates from the midline of the plane of entry into the pelvis minor, which may be anterior (towards the sacrum) or more commonly posterior (towards the symphysis). Mild asynclitism is common and does not worsen prognosis of labour, but moderate or severe asynclitism is associated with increased operative delivery.20 The evaluation of foetal positioning using transabdominal transverse plane in OA foetuses distinguishes the occiput and the cerebral midline (hyperechoic), which corresponds to the sagittal suture and is asymmetrical in relation to the parietal bones. In the OP position, we use the easily identifiable orbits as a reference point to describe the squint sign,21 where we observe a single orbit below the pubic symphysis in these cases. In the OT position, we use the cerebral midline with identification of the thalami, which may be displaced towards the sacrum in anterior asynclitism (sunset of thalamus and cerebellum sign) and towards the pubis in posterior asynclitism. Lateral asynclitism has also been described, between the foetal head and body, in which the foetal head has a lateral orientation of 90° to the spinal axis, assessed by longitudinal transabdominal imaging, with the image of the four cardiac chambers at the same level as the foetal profile.22
‘Four chamber view’ and ‘strabismus sign without nose’ were classified as marked/severe asynclitism. ‘Midline deviation’ and ‘strabismus sign with nose’ were classified as moderate asynclitism.12
Usefulness of intrapartum ultrasound for instrumentationIt has already been noted that digital vaginal examination has a high error rate in determining the position of the foetal head. Prior to operative vaginal delivery, it is necessary to have a precise knowledge of the position of the head, as the correct use of forceps requires both blades to be placed parallel to the sagittal suture. In addition, the vacuum cup must be placed at the “flexion point”, at the level of the sagittal suture, 3cm from the posterior fontanel and 6cm from the anterior fontanel. Positioning too far anteriorly favours deflection and too far laterally favours asynclitism. Inadequate positioning favours foetal injury and increases the number of failed instrumentations.1–3
Another essential parameter is knowledge of the position of the foetus in the birth canal, as operative vaginal delivery is only advised in the mid or low plane when the foetal head is already engaged (Hodge's plane III or De Lee's station 0). The diagnostic error rate of digital vaginal examination in determining the foetal head station is 35%, with a high level of evidence.5 Intrapartum ultrasound has emerged as a tool to help us make this diagnosis, as safety in surgery is a priority.
Because of its accurate diagnosis of head position, intrapartum ultrasound has been used prior to forceps and vacuum extraction, improving the success rate of the operative delivery compared with cases in which it is not used.23–25
Additionally, in cephalic presentation, a correlation has been shown between the position of the foetus in the different pelvic planes and the angle of progression,11 with station 0 corresponding to an angle of 116°. This position has also been associated with a perineal-head distance of 35mm.12 These two aforementioned parameters are the most useful to confirm that the foetal head is indeed in a safe plane for instrumental delivery.
Its use in predicting successful vaginal delivery has also been studied. The angle of progression has been associated with a difficult operative delivery when it is <138° at rest (with a sensitivity of 85.7% and a specificity of almost 100%, 24) or <153° when performed with maternal pushing (which allows assessment of head descent).26,27
When the AoP is combined with the head circumference measurement, it is possible to predict a difficult or complicated instrumental delivery.28 An excessively narrow AoP (<105°) at rest has been associated with a high rate of operative delivery failure and the need for emergency intrapartum caesarean section. Similar findings for the identification of a difficult labour are observed with a head–perineum distance wider than 40mm.29
All these data from previous studies point to the great usefulness of intrapartum ultrasound, particularly for assessing head position. Nonetheless, its use has not yet been shown to reduce foetal or maternal morbidity and mortality, so there are still no recommendations for its routine use in labour by major clinical guidelines. The indications in the evidence should lead us to consider the need for its introduction to improve our practice in the management of vaginal birth.
ConclusionsIntrapartum ultrasound is a safe and easy to learn technique that provides objective and reliable information. It also allows us to assess the position of the foetal head using transabdominal ultrasound and the height of the foetal presentation using transperineal ultrasound. Intrapartum ultrasound allows us to predict a complicated delivery and deliver the foetus more safely. However, there are no results to show that this technique is superior to digital vaginal examination, and it should be used in addition to, not as a replacement for, digital vaginal examination.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis article is not funded.
Patient consentThe clinical management protocols of the Valme Hospital in Seville have been followed in this work and the consent of the patients for its publication has been obtained.
Conflict of interestThis article does not present any conflict of interest.