Mammography has been established as the gold standard for the detection of breast cancer, and imaging techniques such as ultrasonography, magnetic resonance imaging, scintigraphy and positron emission tomography may be useful to improve its sensitivity and specificity. The objective of this study with breast scintigraphy was to evaluate the uptake of 99mTc-thymine in mammary lesions.
METHODSA total of 45 patients were included in this study. Thirty-three patients (73%) were subjected to surgery or percutaneous biopsy, providing histopathological data. The other 12 patients who remained under surveillance received clinical examinations and biannual mammography with a normal follow-up of at least three years, the data from which were used for comparison with the scintimammography results.
RESULTSThe majority of patients (64.4%) had clinically impalpable lesions with a mammogram diagnosis of microcalcifications, impalpable nodules, or focal asymmetry. Of the studied lesions, 87% were smaller or equal to 20 mm in diameter, and 22% had malignant histopathological findings. Scintigraphy with 99mTc-thymine had a sensitivity of 70%, a specificity of 85.7%, positive and negative predictive values of 58.3% and 90.9%, respectively, and an accuracy of 82.2%.
CONCLUSIONSThe results of this study are consistent with those previously reported by other authors. The good specificity and high negative predictive value of this technique and the absence of uptake in the heart indicate that it may be a promising complementary method in clinical practice and that it may contribute to reducing unnecessary benign biopsies.
Breast cancer is a major public health problem, the incidence and mortality of which are continuously increasing. Breast cancer represents the most common malignancy in women, affecting more than one million individuals every year worldwide (1,2).
An early diagnosis of breast cancer may result in a better prognosis. Thus, regular screenings are recommended by health systems around the world. Mammography has been established as the gold standard method for the detection of breast cancer (3-5). The efficacy of cancer screening using mammography has been demonstrated in both randomized trials and observational studies (3-5). Mammographic screening reduces the mortality from breast cancer in women between 40 and 69 years of age by 20 to 35% (4,6). However, not all malignancies are detected using this screening method. Major factors that lead to false-negative findings using mammography include breast density, implants, severe dysplastic disease, and significant architectural distortion following breast surgery or radiation therapy (7-10).
Approximately 90 to 95% of women with abnormal mammogram findings do not have breast cancer. The relative inefficiency reflected by this statistic highlights the necessity of new diagnostic methods that can improve the sensitivity and specificity of mammography (10,11). The development of improved non-invasive diagnostic methods for the screening of breast lesions is needed, which would reduce the requirement for invasive procedures such as breast biopsy for a precise diagnosis (10,11). Conventional biopsies, in addition to the potential for the involvement of hospitalization, anesthesia, and clinical complications, are unnecessary in 80% of cases and may induce changes in the breast parenchyma that hinder subsequent mammographic readings (4,10). In addition, procedures such as percutaneous or surgical biopsy can cause anxiety, inconvenience, and discomfort to the patient and can add medical costs to both the patient and the health care system (10-12).
In the last decade, progress in pharmacology combined with evolving technology has enabled the establishment of scintimammography as a non-invasive technique for the localization and staging of malignant tumors of the breast using molecules such as Sestamibi and Tetrofosmin labeled with technetium-99m (99mTc) (13-15). Other molecules such as 99mTc(V) dimercaptosuccinic acid (DMSA) and 99mTc-labeled alkyl triphenyl phosphonium (99mTc-Mito10-MAG3) are also being studied to improve detection (16,17). The quality of scintimammography is not compromised by breast density, which limits the effectiveness of mammography particularly in young women. Breast scintigraphy has a major indication for select groups of patients with dense breasts; patients using hormone therapy; patients suspected of having recurrent disease resulting in architectural distortions secondary to previous surgery; patients undergoing chemotherapy or radiotherapy or who have breast implants; and patients at high risk for breast cancer (15,18-21). Scintimammography is also useful for the study of breast cancer multicentricity (13,15).
A recent meta-analysis of 42 studies that used ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), scintimammography, and positron emission tomography (PET) determined that MRI seemed to be a more useful complement to existing surveillance methods to assess patients with suspected recurrent and/or metastatic breast cancer (17). Although MRI can be applied in these patient populations, its usage is limited by higher costs and a higher rate of false-positive results compared with mammography (4).
In previous reports, we presented the use of 99mTc-thymine in the evaluation of nodules and the thickening of breast tissue. The pattern of 99mTc-thymine uptake could differentiate malignant lesions of the breast from benign lesions and breast densities in which there is uptake of the radiopharmaceutical (22). We also compared the uptake of 99mTc-thymine and 99mTc-sestamibi in malignant breast lesions and found that 99mTc-thymine exhibited higher sensitivity, specificity, accuracy, and positive predictive values compared to 99mTc-sestamibi (19).
Here, we evaluated the use of 99mTc-thymine for the study of malignant microcalcifications and initial palpable and impalpable malignant lesions of the breast.
METHODS AND MATERIALSStudy subjects consisted of 45 patients of the gynecology and mastology services of two public hospitals. Inclusion criteria were: (I) patients who detected changes in their breast self-examination, (II) patients with microcalcifications detected using mammography consisting of asymmetry or focal nodules smaller or equal to 25 mm in diameter, and (III) patients with BI-RADS® categories 3, 4, or 5. We excluded patients based on the following criteria: (I) breast lesions greater than 25 mm in diameter, (II) prior chemo or hormone therapy, (III) breast surgery or prior homolateral radiotherapy, and (IV) pregnancy or lactation.
The BI-RADS system includes categories that are used to standardize interpretation of mammograms among radiologists (23). BI-RADS assessment categories can be summarized as: Category 0 - need additional imaging evaluation; Category 1 - negative; Category 2 - benign finding; Category 3 - probably benign finding - follow-up in a short time frame is suggested; Category 4 - suspicious abnormality, biopsy considered; Category 5 - highly suggestive of malignancy, appropriate action needed; Category 6 - known biopsy - proven malignancy.
The average age of the patients studied was 49.9 years and ranged from 26 to 80 years. All patients were informed about the procedure and, after acceptance for inclusion in the study, signed a written informed consent. The research protocol was approved by the research ethics committee of the institution.
To evaluate breast lesions, 370 MBq (10 mCi) of 99mTc-thymine was injected intravenously into the forearm, contralateral to the breast with the lesion. Patients were placed in a prone position on a foam mattress, and the studied breast was positioned to make it accessible. The other breast remained compressed to the mattress. The homolateral arm of the affected breast was placed above the patient's head in a position as comfortable as possible. The surface of the collimator (a device of the gamma camera that is capable of collimating radiation to produce the patient's images) touched the side of the body with the studied breast.
Counts were acquired in a 15% window centered at 140 keV. The acquisition of images was initiated 15 minutes after the administration of 99mTc-thymine, and each acquisition lasted for 10 minutes. Both breasts were evaluated. The first lateral image obtained was of the breast without lesions, followed by the breast with the suspected tumor. Following image acquisition, the patient was placed in the supine position with the hands behind the head.
Planar images were analyzed separately by two nuclear medicine physicians and, when the opinions were discordant, the results were determined by consensus. Using a qualitative analysis of images, scintigraphy was considered positive when there was a high uptake of the radiopharmaceutical in a segment of the breast. Scintigraphy was considered negative in cases where there was a homogeneous distribution of the radiopharmaceutical in both breasts.
The data were evaluated by the analysis of the sensitivity, specificity, positive and negative predictive values, and measures of accuracy (confidence interval of 95%; 95% CI) for scintigraphy in relation to the standard for histology (positive and negative).
The histopathological samples were obtained from study patients with breast mammography results with BI-RADS® classifications of category 4 or 5, which included 33 patients. Twelve patients with BI-RADS® classification of category 3 had been recommended for monitoring with biannual mammography. We used the follow-up period of three years and the radiological gold standard for comparison with the outcome of breast scintigraphy in these patients.
The degree of agreement was evaluated using the Kappa coefficient. The criterion for determination of significance was 5%.
RESULTSThirty-three of the 45 patients studied (73%) were subjected to surgery or percutaneous biopsy, providing histopathological data. The patients (n = 12) that remained under surveillance received clinical examinations and biannual mammography with a normal follow-up of at least three years, the data from which were used for comparison with the scintimammography results.
A majority of patients (29/45; 64.4%) had clinically impalpable lesions with a mammogram diagnosis of microcalcifications, impalpable nodules, or focal asymmetry. Sixteen patients (35.6%) had palpable lesions. Clustered microcalcifications, which were or were not associated with a nodule, were present in 24/45 patients (53%). Among the studied lesions, 87% were smaller or equal to 20 mm in diameter (41/47). Two patients had two lesions.
Ten (22%) of the 45 patients studied had malignant histopathological findings (11 lesions - eight cases of infiltrating ductal carcinoma, one case of in situ ductal carcinoma and invasive lobular carcinoma, and one case of cribriform type intraductal carcinoma. All patients with confirmed breast cancer were between 42 and 75 years old.
In comparison with breast mammography, 7/10 of the cancer cases were correctly identified by breast scintigraphy with 99mTc-thymine. In three patients (3/10), breast scintigraphy showed false-negative results (a palpable nodule with normal mammogram, an irregular nodule suspected for malignancy, and clustered microcalcifications on mammography).
Thirty patients with negative breast scintigraphy results had histopathology and/or radiological follow-up for three years. Four patients who had positive breast scintigraphy had benign histopathological biopsies. The false-positive results were: two cystic nodules, one fibroadenoma, and an atypical hyperplasia. In one patient (BI-RADS® 3) with a positive breast scintigraphy, histopathological examination was not performed by decision of the mastology service, which followed the patient for three years. Table 1 shows the patients' characteristics, Table 2 lists the measures of accuracy of the patients studied, and Table 3 shows the patients sorted by BI-RADS.
Patient characteristics.
| Patient | Age | Location | Side | Micro-calcifications | BI-RADS® | Lesion size on mammography (mm) | Scintigraphy | Biopsy | Histopathology |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 80 | UOQ | R | Yes | 4 | NEG | NEG | Fibrocystic disease | |
| 2 | 58 | Retroareolar | R | 4 | POS | POS | IDC (15 mm) | ||
| 3 | 52 | UOQ | L | Yes | 4 | NEG | NEG | Fibrocystic disease | |
| 4 | 42 | LIQ | L | Yes | 5 | 9.2 | POS | POS | In situ ductal carcinoma and invasive lobular carcinoma (20 mm) |
| 5 | 52 | UOQ | L | 3 | 25 | NEG | Follow-up | - | |
| 6 | 50 | UOQ | L | Yes | 4 | POS | NEG | Fibrocystic disease | |
| 7 | 55 | UIQ | L | Yes | 4 | NEG | NEG | Usual ductal hyperplasia | |
| 8 | 46 | LIQ | L | Yes | 3 | 18 and 7 | NEG | Follow-up | - |
| 9 | 43 | UOQ | L | 4 | 18 | POS | POS | IDC (18×13 mm) | |
| 10 | 67 | Retroareolar | L | Yes | 3 | NEG | Follow-up | - | |
| 11 | 50 | Asymmetry on UOQ, UIQ | R | 3 | NEG | Follow-up | - | ||
| 12 | 54 | UIQ and UOQ | R | 4 | 17 | NEG | NEG | Fibrocystic disease | |
| 13 | 61 | UOQ | R | 3 | 12 | NEG | Follow-up | - | |
| 14 | 68 | UOQ | L | 4 | 15 | NEG | NEG | Fibrocystic disease | |
| 15 | 56 | UIQ | L | 4 | 25 | NEG | NEG | - | |
| 16 | 30 | Retroareolar | L | 3 | 25 | NEG | Follow-up | - | |
| 17 | 61 | UOQ | L | Yes | 4 | NEG | NEG | Fibrocystic disease | |
| 18 | 56 | UOQ | L | Yes | 3 | NEG | Follow-up | - | |
| 19 | 55 | Asymmetry on LIQ and UIQ | L | 3 | NEG | Follow-up | - | ||
| 20 | 65 | UOQ | R | Yes | 4 | NEG | Follow-up | - | |
| 21*) | 36 | LIQ | R+L | Yes (L) | 4 | 20 (R) | POS (R) | NEG | Fibroadenoma |
| 22 | 67 | LOQ | L | Yes | 4 | NEG | NEG | Fibrocystic disease | |
| 23 | 58 | UOQ | R | 4 | 13 | NEG | NEG | Fibrocystic disease | |
| 24 | 39 | UIQ | R | 4 | 15 | POS | NEG | AEH | |
| 25 | 75 | UOQ | L | 5 | POS | POS | IDC (10 mm) | ||
| 26 | 70 | LIQ | L | Yes | 4 | NEG | NEG | - | |
| 27 | 45 | LIQ | R | Yes | 4 | NEG | NEG | - | |
| 28 | 68 | UOQ | L | 5 | 25 | NEG | POS | IDC (25 mm) | |
| 29 | 54 | UOQ | L | Yes | 4 | NEG | Follow-up | - | |
| 30 | 61 | UOQ | L | Yes | 4 | NEG | NEG | - | |
| 31 | 55 | UOQ | R | Yes | 4 | NEG | POS | IDC (10 mm) | |
| 32 | 61 | Subareolar | L | Yes | 4 | POS | POS | Cribriform IDC (20 mm) | |
| 33 | 26 | UOQ | R | 4 | 20 | NEG | NEG | Fibroadenoma | |
| 34 | 67 | Retroareolar | R | Yes | 4 | NEG | NEG | Fibrocystic disease, adenosis | |
| 35 | 63 | Asymmetry, LIQ | L | 4 | NEG | NEG | - | ||
| 36 | 62 | UOQ and LOQ | L | Yes | 4 | NEG | NEG | Fibrocystic disease, adenosis, usual ductal hyperplasia | |
| 37 | 50 | UOQ | L | Yes | 4 | POS | NEG | Fibrocystic disease, adenosis | |
| 38 | 58 | UOQ | L | Yes | 4 | NEG | NEG | Adenosis, usual ductal hyperplasia | |
| 39 | 58 | Asymmetry | R | 4 | POS | POS | IDC (20 mm) | ||
| 40 | 44 | Asymmetry | L | 4 | NEG | POS | IDC (25 mm) | ||
| 41 | 48 | UOQ | L | 4 | POS | POS | IDC (23 mm) | ||
| 42 | 49 | UOQ | R | 4 | 20 | NEG | NEG | Fibrocystic disease | |
| 43 | 48 | UIQ and LIQ | R | Yes | 4 | NEG | NEG | ||
| 44 | 36 | UIQ and LIQ | L | Yes | 4 | NEG | Follow-up | - | |
| 45 | 50 | LIQ | L | 4 | 8 | POS | Follow-up | - |
Abbreviations: UOQ, upper outer quadrant; UIQ, upper inner quadrant; LOQ, lower outer quadrant; LIQ, lower inner quadrant; AEH, atypical epithelial hyperplasia; IDC, invasive ductal carcinoma; NEG, negative; POS, positive; R, right; L, left.
Measures of accuracy of scintigraphy using 99mTc-thymine for the diagnosis of breast cancer.
| Measures | % | LL 95% | UL 95% |
|---|---|---|---|
| Sensitivity | 70.0 | 41.6 | 98.4 |
| Specificity | 85.7 | 74.1 | 97.3 |
| Positive Predictive Value | 58.3 | 30.4 | 86.2 |
| Negative Predictive Value | 90.9 | 81.1 | 100 |
| Accuracy | 82.2 | 71.1 | 93.4 |
LL 95%: Lower limit of 95%; UL: Upper limit of 95%.
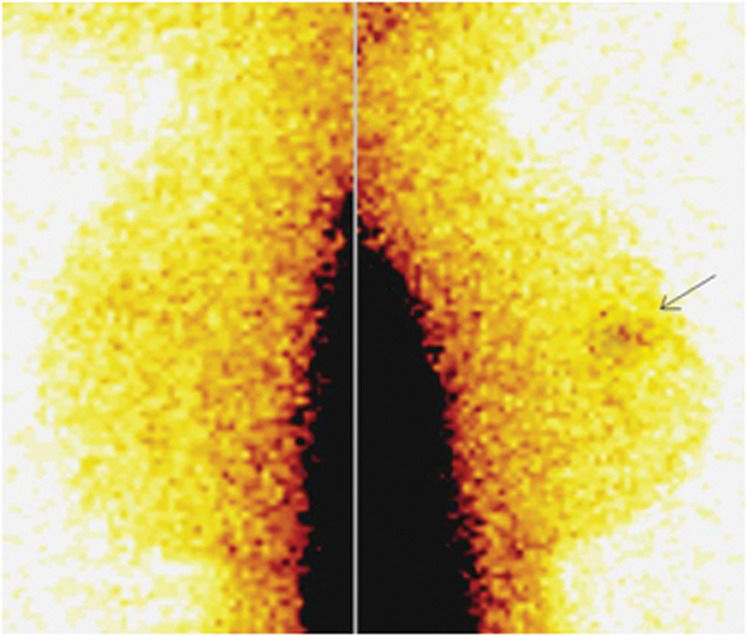
We observed a significant concordance (Kappa = 0.520, standard error = 0.147, p = 0.0002) between the diagnosis by scintigraphy and the pattern of histology, but it was of a moderate degree. Figure 1 illustrates a normal distribution of 99mTc-thymine scintigraphy in the anterior view with a high liver uptake. We can observe that there is no heart uptake. Figure 2 is an example of a negative scintigraphy image obtained with 99mTc-thymine. A homogenous distribution of the radiopharmaceutical can be observed in both breasts. Figure 3 shows an example of a positive scintigraphy image obtained with 99mTc-thymine in which an increased uptake of the radiopharmaceutical is observed in the region of the right breast nodule.
A 58-year-old patient with a nodule (15 mm) in the right breast and a mammographic BI-RADS® 4 (a nodule in the right upper quadrant + microcalcifications). Breast scintigraphy with 99mTc-thymine shows uptake in right breast. Histopathological findings showed an infiltrating ductal carcinoma.
Although the efficacy of mammography has been demonstrated, perfect sensitivity or specificity is not achieved in women undergoing screening. As such, the issue of adverse consequences for women who do or do not have breast cancer has been a source of growing attention (15,24,25).
If breast cancer screening is to be successful, the majority of cancers among screened women must be detected when tumors are small and before the occurrence of distant or nodal metastases. To achieve this, a combination of imaging modalities may be superior to any single screening technique (9). 99mTc-sestamibi and 99mTc-tetrofosmin were first described as myocardial perfusion tracers due to their property of accumulating in cells with higher mitochondrial activity and demonstrating perfused myocardium in contrast with ischemic and fibrotic regions. Afterwards, they were applied to detect tumors based on the principle that tumors such as breast cancer generally have higher mitochondrial activity than the surrounding cells. Despite promising initial results, breast scintigraphy with 99mTc-sestamibi is not yet included in the routine diagnosis of breast cancer. The sensitivity of the method was reported to range from 84 to 96% in initial studies, and the specificity ranged from 86 to 100% (13,26,27). However, in more recent publications, particularly in multicenter studies in which a large number of palpable and impalpable lesions were studied, sensitivity and specificity were both reduced (28-30).
Tiling et al. (31) reported that tumor size appears to be crucial in limiting the capacity of scintigraphy to detect breast cancer, and a number of studies have also identified a correlation between the sensitivity of breast scintigraphy and the diameter of the tumor (29,31).
In a modified meta-analysis of the use of 99mTc-sestamibi for the diagnosis of initial breast cancer in 2,727 lesions, Khalkhali and Itti (32) stated that the overall sensitivity and specificity of breast scintigraphy were 83.3% and 81.3%, respectively. The overall sensitivity reported included palpable and impalpable lesions, which likely explains the difference in reported results in this and other reviews (32). In a multicenter study to assess the effectiveness of breast scintigraphy with 99mTc-sestamibi in 1243 women with 33% palpable lesions, Sampalis et al. (33) concluded that breast scintigraphy was highly effective and potentially useful as a complement to mammography for the early detection of breast cancer. These authors reported a sensitivity and specificity of 93% and 87%, respectively, with a negative predictive value of 98% and a positive predictive value of 58% (33).
We previously described a technique for the labeling of thymine, a thymidine precursor, with 99mTc. (19,22). Here, we obtained a sensitivity of 70%, a specificity of 85.7%, an accuracy of 82.2%, and positive and negative predictive values of 58.3% and 90.9%, respectively. It is noteworthy that the total number of patients was 45, which were divided into two groups following BI-RADS® 3 classification: one (n = 33) with histopathological results and the other (n = 12) without biopsy. The false-positive results in most of the other studies using 99mTc-sestamibi resulted from the presence of fibroadenoma, atypical hyperplasia, fibrocystic disease, and inflammatory disease (26,31,34,35). In our study, the four false-positive results also consisted of fibrocystic breast changes (two cases), fibroadenoma (one case), and one case of atypical hyperplasia. Patients with atypical hyperplasia have been shown to have an increased relative risk for breast cancer and a higher incidence of positive breast scintigraphy (36). The results of 99mTc-sestamibi scintigraphy are least useful in cases of breast microcalcifications and in situ carcinoma, as reported by Gommans et al. (37). Moreover, unlike 99mTc-thymine, the myocardial uptake of the 99mTc-sestamibi is relatively high, which leads to greater background activity due to the proximity to breast tissues. Despite this, intravenously administered 99mTc-thymine has the potential advantage of being used in radioguided surgeries to detect impalpable breast lesions without conventional Radioguided Occult Lesion Localization (ROLL) and Sentinel Node and Occult Lesion Localization (SNOLL) techniques.
In nearly all reports of breast scintigraphy, 99mTc-sestamibi or 99mTc-tetrofosmin was used. The 99mTc-thymine results in this study are consistent with those reported by other authors (30,38), even though the majority of patients in this study had impalpable lesions.
To be an acceptable complementary method to mammography, breast scintigraphy must provide high specificity. We obtained a high level of specificity and a high negative predictive value in this breast scintigraphy study. These make this test attractive because of the potential to reduce unnecessary biopsies. Other studies have reported a better sensitivity but a lower specificity than those reported in this study (39). Although the early detection of breast cancer needs to be improved with the development of equipment that can discover smaller lesions, the employment of 99mTc-thymine seems to be more advantageous than other radiopharmaceuticals because it is a precursor to a DNA nitrogenous base that plays an important role in tumoral growth. Some of the main characteristics of the metabolism of tumor cells are the increase of glycolysis and mitochondrial activity, the synthesis of nucleic acids, and the production of proteins previous to mitosis. Unlike methods that simply demonstrate an increase in mitochondrial activity, which may occur in tissues that are not under cell division, 99mTc-thymine has the potential to demonstrate the synthesis of nucleic acids related to tumor growth. This effect increases the sensitivity and specificity of tumor detection.
Recently, Sun et al. (40) imaged DNA synthesis with PET using 18F- 1-(2‘-deoxy-2‘-fluoro-beta-D-arabinofuranosyl) thymine (FMAU), a pyrimidine analogue that is phosphorylated by thymidine kinase and incorporated into DNA. Their results demonstrated that 18F-FMAU was selectively retained in the DNA of proliferating cells and was resistant to degradation (40). We have similarly shown that 99mTc-thymine is incorporated into cellular DNA (22). Unlike PET and PET-CT, which require expensive equipment with limited availability worldwide, conventional gamma cameras are able to perform SPECT imaging and are much more readily available. Therefore, the use of 99mTc-thymine as a radiopharmaceutical for SPECT imaging has the potential for broader use.
It is important to note that our study has limitations; for instance, our study included a great number (87%) of lesions smaller or equal to 20 mm and few patients with malignant lesions. These factors could explain the lower sensitivity that we report for scintigraphy. Further studies are needed to provide a greater understanding of the application of this technique in these two groups. Nonetheless, the high level of specificity and the high negative predictive value of this technique indicate that the use of breast scintigraphy with 99mTc-thymine may be a promising complementary method, particularly in selected patients. It may be a useful adjunct method in high-risk patients such as those with prior breast cancer, a very strong family history of breast cancer, lobular cancer in situ, or Paget disease. Scintimammography may also be helpful for the study of borderline lesions of BI-RADS categories 3 and 4 or patients under evaluation for recurrence and adjuvant chemotherapy. Therefore, scintimammography may be a valuable tool in clinical practice that can reduce the number of unnecessary benign biopsies.
AUTHOR CONTRIBUTIONSRibeiro MP contributed to the screening of the patients, design and writing of the paper. Souza SA, Fonseca LM, and Gutfilen B contributed to the execution of scintigraphy, discussion of the results, design and writing of the paper. Lopes FP contributed to the discussion of the results, design and writing of the paper. Castro PH contributed to the design and writing of the paper.
This study was supported by grants from Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
No potential conflict of interest was reported.