To evaluate the diagnostic accuracy of magnetic resonance imaging of the knee in identifying traumatic intraarticular knee lesions..
METHODS300 patients with a clinical diagnosis of traumatic intraarticular knee lesions underwent prearthoscopic magnetic resonance imaging. The sensitivity, specificity, positive predictive value, negative predictive value, likelihood ratio for a positive test, likelihood ratio for a negative test, and accuracy of magnetic resonance imaging were calculated relative to the findings during arthroscopy in the studied structures of the knee (medial meniscus, lateral meniscus, anterior cruciate ligament, posterior cruciate ligament, and articular cartilage).
RESULTSMagnetic resonance imaging produced the following results regarding detection of lesions: medial meniscus: sensitivity 97.5%, specificity 92.9%, positive predictive value 93.9%, positive negative value 97%, likelihood positive ratio 13.7, likelihood negative ratio 0.02, and accuracy 95.3%; lateral meniscus: sensitivity 91.9%, specificity 93.6%, positive predictive value 92.7%, positive negative value 92.9%, likelihood positive ratio 14.3, likelihood negative ratio 0.08, and accuracy 93.6%; anterior cruciate ligament: sensitivity 99.0%, specificity 95.9%, positive predictive value 91.9%, positive negative value 99.5%, likelihood positive ratio 21.5, likelihood negative ratio 0.01, and accuracy 96.6%; posterior cruciate ligament: sensitivity 100%, specificity 99%, positive predictive value 80.0%, positive negative value 100%, likelihood positive ratio 100, likelihood negative ratio 0.01, and accuracy 99.6%; articular cartilage: sensitivity 76.1%, specificity 94.9%, positive predictive value 94.7%, positive negative value 76.9%, likelihood positive ratio 14.9, likelihood negative ratio 0.25, and accuracy 84.6%.
CONCLUSIONMagnetic resonance imaging is a satisfactory diagnostic tool for evaluating meniscal and ligamentous lesions of the knee, but it is unable to clearly identify articular cartilage lesions.
Avaliar a validade da ressonância magnética do joelho no diagnóstico das lesões intra-articulares traumáticas do joelho.
MÉTODOPopulação de 300 pacientes, com quadro clínico sugestivo de lesões intra-articulares traumáticas do joelho, que tiveram seus laudos de ressonância magnética comparados com os resultados obtidos nas artroscopias realizadas posteriormente. Foram calculados a sensibilidade, especificidade, valor preditivo positivo, valor preditivo negativo, razão de verossimilhança positiva, razão de verossimilhança negativa e acurácia da ressonância magnética do joelho para o diagnóstico de lesões em cada estrutura intra-articular estudada do joelho (menisco medial, menisco lateral, ligamento cruzado anterior, ligamento cruzado posterior e cartilagem articular).
RESULTADOSEm relação às lesões do menisco medial, a sensibilidade da ressonância magnética foi de 97.5%, a especificidade de 92.9% o valor preditivo positivo de 93.9%, o valor preditivo negativo de 97%, a razão de verossimilhança positiva de 13.7, a razão de verossimilhança negativa de 0.02 e a acurácia de 95.3%. Para o menisco lateral, a sensibilidade da ressonância magnética foi de 91.9%, a especificidade de 93.6%, o valor preditivo positivo de 92.7%, o valor preditivo negativo de 92.9%, a razão de verossimilhança positiva de 14.3, a razão de verossimilhança negativa de 0.08 e a acurácia de 93.6%. Para o ligamento cruzado anterior, a sensibilidade da ressonância magnética foi de 99.0%, a especificidade de 95.4%, o valor preditivo positivo de 91.9%, o valor preditivo negativo de 99.5%, a razão de verossimilhança positiva de 21.5, a razão de verossimilhança negativa de 0.01 e a acurácia de 96.6%. Para o ligamento cruzado posterior, a sensibilidade da ressonância magnética foi de 100%, a especificidade de 99%, o valor preditivo positivo de 80%, o valor preditivo negativo de 100%, a razão de verossimilhança positiva de 100, a razão de verossimilhança negativa de 0.01 e a acurácia de 99.6%. Para as lesões condrais a sensibilidade da ressonância magnética foi de 76.1%, a especificidade de 94.9%, o valor preditivo positivo de 94.7%, o valor preditivo negativo de 76.9%, a razão de verossimilhança positiva de 14.9, a razão de verossimilhança negativa de 0.25 e a acurácia de 84.6%.
CONCLUSÃOA ressonância magnética apresenta alta acurácia para identificar as lesões meniscais e ligamentares do joelho, mas é insatisfatória para diagnosticar as lesões da cartilagem articular.
Due to its anatomical configuration and because of its being the biggest joint of the human body, the knee is frequently subjected to direct trauma that can result in injuries of variable gravity.1–5.
Intraarticular knee lesions are associated with significant morbidity and frequently need surgical treatment and extensive rest. Although they are common, their correct diagnosis still is a challenge.6–8
Clinical tests may be confusing, and delay in diagnosis can result in social and economic problems and sometimes in a worse prognosis.8–10 Therefore, complementary diagnostic tools are often necessary,11–14 mainly when suspicion of multiple lesions exists.15,16
Arthroscopy is considered as “the gold standard” for diagnosis of traumatic intraarticular knee lesions, having an accuracy as high as 95% to 98%.17–20 However, arthroscopy is an invasive and expensive tool that requires hospitalization and regional or general anesthesia, thus presenting all the potential complications of an open surgical procedure.21–27
During the last decade, magnetic resonance imaging has been confirmed as the ideal approach for primary diagnosis of traumatic intraarticular knee lesions.28–31 It is noninvasive, fast, can be done on an outpatient basis, and is free of complications. Despite this, magnetic resonance imaging is a new technology, 32 which means that clinical experience is still lacking. Additionally, there are doubts about the accuracy of magnetic resonance imaging and the clinical advantages of this test, since it is still an expensive procedure.33–36
With the purpose of investigating the accuracy of magnetic resonance imaging in patients with clinical signs of traumatic intraarticular knee lesions, we compared its findings with those obtained from the subsequent arthroscopies.
METHODSDesign: Diagnostic test evaluation.
Setting: Department of Orthopedics and Traumatology, University of Londrina, Londrina, Brazil.
Participants: A population of 300 consecutive patients with clinical signs of traumatic intraarticular knee lesions examined from August 1998 through March 2002 who underwent prearthoscopic magnetic resonance imaging where included in the study. Patients with previous knee injuries and knee surgery where excluded.
Procedures:
Magnetic Resonance:
All the exams were performed in the same diagnostic imaging center with blinded interpretation by 3 radiology specialists in magnetic resonance imaging. A Phillips device model NT5 with magnetic-field strength of 0.5 TESLA was used, along with a special knee bobbin. The magnetic resonance imaging sequences were TSE-T2; coronal SET1, TSE-T2, SPIR, and TSE-T2 oblique; and coronal and sagittal GRE-T2 (special sequences for the meniscus).
Arthroscopy:
The arthroscopies were all done in a hospital environment, with complete preoperative care, with most them being outpatient surgery. A Stryker 3 CCD video camera was used with a 4 mm Karl-Storz arthroscope with a 30-degree angle. Standard arthroscopic portals were used: the superomedial portal for fluid outflow, the inferolateral portal for the arthroscope, and the inferomedial portal for instrumentation. During arthroscopy, a systematic examination of the knee was performed with a complete evaluation of the joint. All arthroscopies where done by the same surgeon and filmed on appropriate tapes.
Data Analysis:
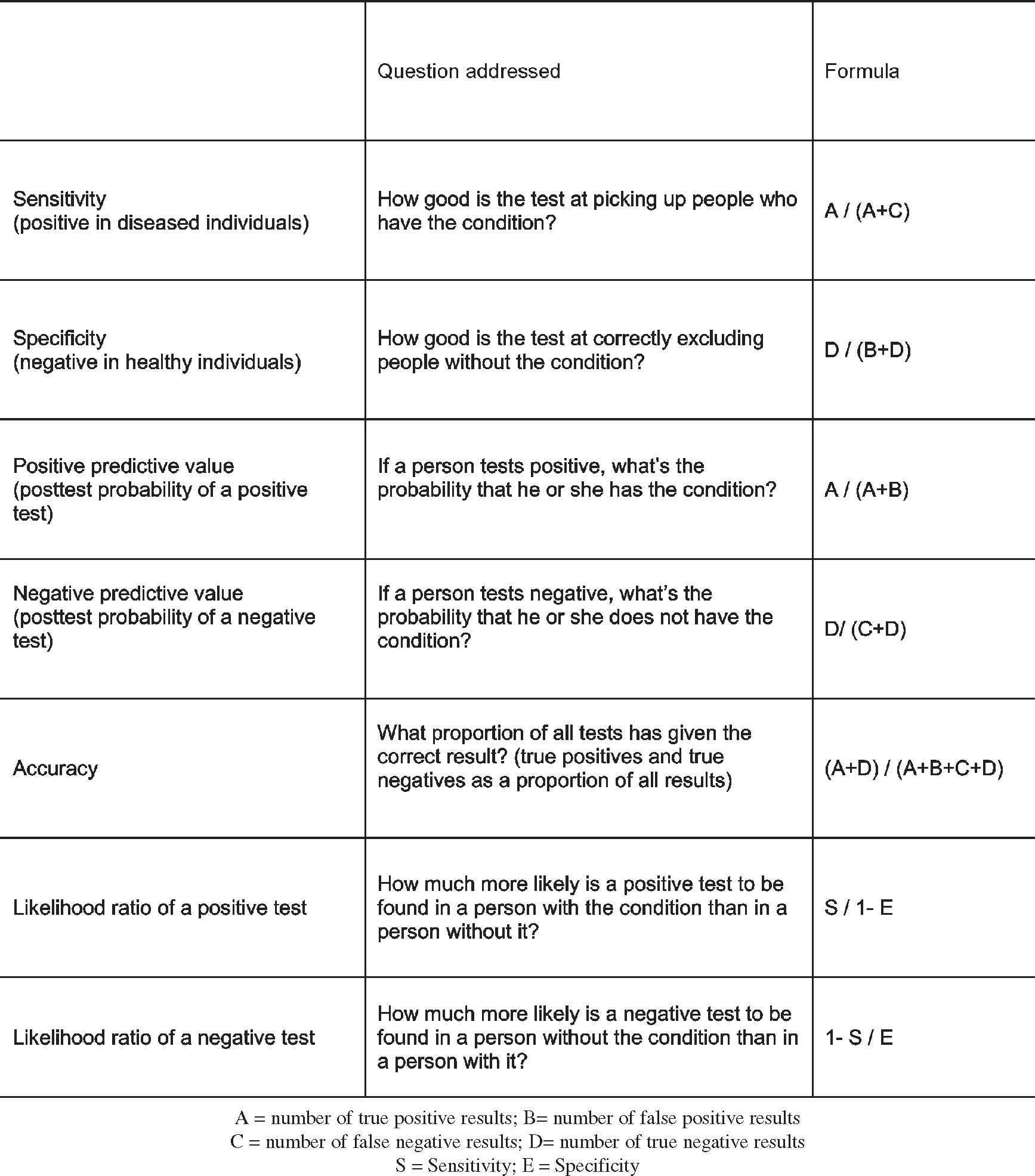
The intraarticular structures included in the study were the medial meniscus, the lateral meniscus, the anterior and posterior cruciate ligaments, and the articular cartilage. All these structures were evaluated to identify lesions, and the results of the magnetic resonance imaging were compared with the arthroscopies (considered the gold standard for diagnosis). The following were calculated as defined in Figure 1 using Epi Info 6, V 6.04 software: sensitivity, specificity, accuracy, positive predictive value, negative predictive value, likelihood ratio for a positive test, likelihood ratio for a negative test, and the 95% confidence intervals.
RESULTSResults for all the measured parameters are presented in Table 1. It can be seen that MRI has very high levels of sensitivity, specificity, positive predictive value, positivenegative value and accuracy for meniscal and ligamentous lesions. Likelihood of positive and negative ratio was also excellent. For articular cartilage lesions, results were not nearly as precise.
Results of the data analysis: sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood rate, negative likelihood rate, and accuracy of magnetic resonance imaging to evaluate lesions of the medial meniscus, lateral, meniscus, anterior cruciate ligament, posterior cruciate ligament, and articular cartilage
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | Positive Likelihood rate | Negative Likelihood rate | |
|---|---|---|---|---|---|---|---|
| Medial meniscus | 97.5% | 92.9% | 93.9% | 97.0% | 95.3% | 13.7 | 0.02 |
| Lateral meniscus | 91.9% | 93.6% | 92.7% | 92.9% | 93.6% | 14.3 | 0.08 |
| Anterior cruciate ligament | 99.0% | 95.4% | 91.9% | 99.5% | 96.6% | 21.5 | 0.01 |
| Posterior cruciate ligament | 100% | 99.7% | 80.0% | 100% | 99.6% | 100 | 0.01 |
| Articular cartilage | 76.1% | 94.9% | 94.7% | 76.9% | 84.6% | 14.9 | 0.25 |
While clinical data remain the most important tool for identifying intraarticular knee lesions, sometimes it is insufficient to elucidate the final diagnosis.
Until the last decade, diagnostic arthroscopy was the only possible way to clarify a doubtful diagnosis. Unfortunately, it is an invasive and expensive procedure, and its overuse has produced unnecessary complications, such as infection, neurovascular lesions, damaged intraarticular materials, amongst others.
With the evolution of the materials and surgical techniques, arthroscopy has become more of a surgical method than a diagnostic tool, and magnetic resonance is fast becoming the favorite diagnostic method for many of surgeons52–54.
The results of the present study demonstrate that knee meniscal and cruciate ligament lesions can be accurately diagnosed by magnetic resonance and support the findings of other studies.37–40 The high sensitivity and negative predictive value of the magnetic resonance allow excluding a diagnostic arthroscopy in patients with a doubtful clinical exam, 41–44 saving costs and reducing patient risk.45–48
Willians49 performed a study in which magnetic resonance imaging scans were performed on 69 patients waiting for knee arthroscopy. All patients had a clinical diagnosis of traumatic intraarticular knee lesion. Of the patients scanned, magnetic resonance imaging ruled out lesions in 24 patients, who were removed from the waiting list. After 9 months, only 1 of them had been re-listed for therapeutic arthroscopy because of continued symptoms.
Since magnetic resonance imaging results in a fast and accurate diagnosis, it allows the surgeon time to plan the surgical procedure prior to surgery for treatment, whereas diagnostic arthroscopy necessitates immediate treatment, without previous study.
Although knee magnetic resonance is still considered an expensive tool, with costs ranging from US $250 to US $500, the total cost of arthroscopy is far greater, ranging from US $1500 to US $3000. Weinstabl et al, 48 studying the cost-benefit of knee magnetic resonance, evaluated 201patients with clinical signs of knee meniscal lesions who later had undergone arthroscopy. They report that 30% of the diagnoses were false-positives, and that 30% fewer arthroscopies would have resulted in an economy of US $723,600 dollars. The total cost of knee magnetic resonance was US $160,800, and magnetic resonance offered a comparative accuracy of 96% against 78% for clinical examination.
Bui-Mansfield et al46 performed a study to ascertain whether there would be a significant economy if magnetic resonance to complement the clinical examination was done in all cases for which a diagnostic arthroscopy was indicated, using a value of US $1000 dollars for each magnetic resonance procedure. Of 50 diagnostic arthroscopies, 42% had been unnecessary (false-positive results). They observed that if the results of the magnetic resonance had been taken into account before the performance of the arthroscopy, there would have been an economy of US $680 dollars for each case.
Our study demonstrates that magnetic resonance does not appear to have a satisfactory accuracy for diagnosing knee articular cartilage lesions, since it was associated with a great number of false negative results (low sensitivity). It has been proposed that enhancement of the magnetic resonance imaging accuracy with articular cartilage lesions is obtained by the introduction of a special contrast in the knee.50 This procedure is called arthro-resonance (or arthro-MRI), and recent studies have demonstrated this innovation to have good accuracy.51
CONCLUSIONMagnetic resonance imaging has high accuracy to for diagnosing knee meniscal and cruciate ligament lesions, but does not have satisfactory accuracy in detecting articular cartilage lesions.