Anterior cruciate ligament ruptures are frequent, especially in sports. Surgical reconstruction with autologous grafts is widely employed in the international literature. Controversies remain with respect to technique variations as continuous research for improvement takes place. One of these variations is the anatomical double bundle technique, which is performed instead of the conventional single bundle technique. More recently, there has been a tendency towards positioning the two bundles through double bone tunnels in the femur and tibia (anatomical reconstruction).
OBJECTIVESTo compare, through biomechanical tests, the practice of anatomical double bundle anterior cruciate ligament reconstruction with a patellar graft to conventional single bundle reconstruction with the same amount of patellar graft in a paired experimental cadaver study.
METHODSNine pairs of male cadaver knees ranging in age from 44 to 63 years were randomized into two groups: group A (single bundle) and group B (anatomical reconstruction). Each knee was biomechanically tested under three conditions: intact anterior cruciate ligament, reconstructed anterior cruciate ligament, and injured anterior cruciate ligament. Maximum anterior dislocation, rigidity, and passive internal tibia rotation were recorded with knees submitted to a 100 N horizontal anterior dislocation force applied to the tibia with the knees at 30, 60 and 90 degrees of flexion.
RESULTSThere were no differences between the two techniques for any of the measurements by ANOVA tests.
CONCLUSIONThe technique of anatomical double bundle reconstruction of the anterior cruciate ligament with bone-patellar tendon-bone graft has a similar biomechanical behavior with regard to anterior tibial dislocation, rigidity, and passive internal tibial rotation.
Anterior Cruciate Ligament (ACL) ruptures are a frequent injury, especially in sports. Surgical reconstruction with autologous grafts is widely employed in the international literature. Controversies remain with respect to technique variations as continuous research for improvement takes place. One of these variations is the anatomical double bundle technique, which is performed in place of the conventional single bundle (antero-medial bundle) technique1–8. Recently, there has a tendency towards positioning of the two bundles through a double tunnel technique in the femur and the tibia9–13, the so called “anatomical technique.”
The effectiveness of the “Double Bundle” technique has been questioned by some authors14–16, who found similar outcomes when these were compared to conventional “Single Bundle” reconstruction. Harner17, in 2004, posed the question: “Double Bundle or Double Trouble?” Morbidity, biomechanical advantages, and the duration of surgery have been specifically questioned.
In light of this tendency, we propose our study, a direct comparison between the two techniques involving a biomechanical evaluation of the single bundle ACL technique versus anatomical double bundle reconstruction using cadaveric knees and patellar grafts (with no graft amount variation).
MATERIALS AND METHODSSpecimen PreparationEighteen fresh frozen human undamaged cadaveric knees (nine pairs), all from males ranging in age from 44 to 63 years, were used in this study. The femur was cut 20 cm, and the tibia 30 cm from the joint line. The iliotibial tract up to mid-tight, the popliteus musculotendinous unit, and the joint capsule were left intact. The fibula was secured to the tibia to simulate the restraint provided by the interosseous membrane. The knees were stored at −20°C, and were thawed for 24 hours at room temperature before testing. Prior to the procedures, they were submitted to a primary arthroscopic inspection to rule out any previous intra-articular lesions.
Biomechanical testsAnterior tibial displacement simulating the anterior drawer test with the knees at 30, 60 and 90 degrees flexion were the biomechanical tests performed. All knee specimens were tested under three conditions (“Intact,” “Reconstructed,” and “Injured,” in this order), and every test had three cycles, for which the third test’s data were recorded. The knees were first tested after an initial inspection by arthroscopy (“Intact Condition”). They were set up in a Kratos 5002 Universal Biomechanical Test Machine with a 100 kgf load cell connected to a computer system, where anterior displacement (millimeters) and stiffness (Newtons/milimiters) data were recorded, while concomitant internal tibia rotation (degrees) data was recorded by digital photography. A continuous velocity (20mm/min) was applied by a 100N load cell in the tests.
The tibia and femur were fixed to steel tubes with screws. Mounting was accomplished using grips for each bone that allowed their precise positions to be adjusted. The tibia was secured first, with its shaft ranging at 30, 60 and 90 degrees to the load cell axis. Tibia rotation, varus, valgus and translation were allowed by the system. There was a degree graduation mark on the tibial steel tube and a needle to register initial and final tibial rotation values (Figure 1). The unsecured femur was placed with its shaft aligned along the axis of the load cell and its weight supported by the lower grip (Figure 2). Before each test, the tibia was placed in a rotational position midway between its limits of internal and external rotation, and its rotational position in degrees was recorded.
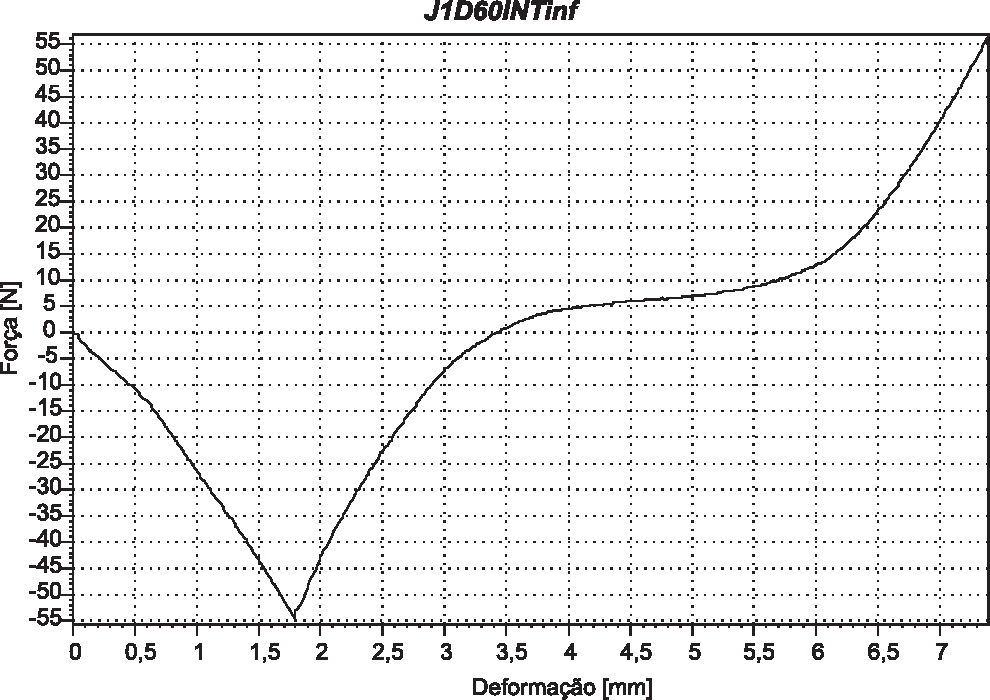
The “zero test point” was determined by a previous short cycle with a posterior drawer followed by an anterior drawer under 50 N load (Figure 3), and the inflexion point of this curve was registered as the “zero point.” All biomechanical tests in the protocol were begun with a short posterior drawer to ensure the presence of the predetermined “zero point” on the anterior drawer curves of the three cycles (Figure 4). The specimens were not disconnected from the original steel tube fixation at any time, including during surgeries, when the whole system was disconnected from the Kratos Machine grips.
LesionsThe ACL lesions were made through an arthroscopic procedure after the “intact” tests and before the “reconstructed” tests.
After the “reconstructed” tests, all bicortical screws were removed followed by the removal of the patellar grafts from the knees.
GroupsSpecimens were divided in two groups, with one knee from each pair. In group A, single bundle reconstruction was performed, and in group B, the opposite side knees were submitted to anatomic double bundle reconstruction (Figure 5).
Surgical technique1) Group A (single bundle):After the original ACL resection, the group A knees were submitted to ACL conventional single bundle reconstruction with a bone-tendon-bone patellar graft. The tibial tunnel parameters for the tibial guide location were 7 mm in front of the PCL (Posterior Cruciate Ligament) at the medial tibial spine basis. For the femoral tunnel, a 7 mm offset guide was positioned in the notch at 11 h in the right knees and 1 h in the left knees. The grafts’ bone plug dimensions were 2.5 cm in length, 10 mm wide and 10 mm deep. Tibial and femoral graft fixation was performed with two sutures (polyester No. 5) through the bone plugs attached to a transversal bicortical screw and washer.
2) Group B ( Anatomic Double Bundle):Anatomical double bundle reconstruction through double femoral and double tibial tunnels was performed using a patellar graft divided longitudinally into two parts with the same length, 5 mm thickness, and 5 mm depth (Figure 6).
The posterior lateral (PL) tibial tunnel location parameters were 7 mm in front of the PCL, behind the lateral tibial spine18, with the extra-articular location at the medial tibial anterior cortical diverging 70 degrees from the coronal plane. The anterior medial (AM) tunnel’s location was 7 mm in front of the posterior lateral guide wire, between the tibial spines, with 50 degrees angulation to the coronal plane. After each tunnel was ready, we confirmed its integrity by introducing an arthroscope into the tunnel.
For the femoral tunnels, we used a 5 mm offset femoral guide introduced through the tibial tunnel when possible. On two occasions, for the PL femoral tunnel, we had to introduce the femoral guide through the anteromedial portal. The PL tunnel was located on the notch at 9:30 hs on the right knees and 14:30 hs on the left knees. The second femoral tunnel (AM) was at 11 hs on right knees and 13 hs on the left knees (Figure 7).
The posterior lateral patellar graft was introduced first through the tunnels, followed by the AM graft. The PL graft was tensioned and fixed at 15 degrees and the AM graft at 90 degrees of knee flexion by two sutures (polyester No. 5) through each bone plug attached to transversal bicortical screws and washers, two on the femur, and two on the tibia.
StatisticsStatistical analysis was performed with Analysis of Variance (ANOVA) of groups with the third cycle data tests of dislocation (millimeters) and stiffness media (Newtons/millimeters).
Evaluation Condition test differences were determined by the Bonferroni test method.
The á value was 5%, and lower p values represented statistically significant differences.
RESULTSThe anterior drawer dislocation results are presented in millimeters and stiffness media in Newtons per millimeter for each evaluation condition: intact, injured, and repaired at 30, 60, and 90 degrees of knee flexion (Table 1). Statistical analysis showed no differences between groups A and B. The tibial passive internal rotation data are presented in degrees for the intact and repaired conditions at 30, 60, and 90 degrees of knee flexion (Table 2). Again, there were no statistical differences between groups A and B
Anterior drawer and stiffness.
| Data Registered | Dislocation (mm) | Stiffness (N/mm) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Flexion Angle | ||||||||||||
| 30° | 60° | 90° | 30° | 60° | 90° | |||||||
| Knee condition | A | B | A | B | A | B | A | B | A | B | A | B |
| Intact | 5.93 | 6.41 | 5.52 | 6.41 | 4.72 | 4.91 | 27.56 | 28.74 | 34.02 | 33.62 | 40.03 | 40.93 |
| Injured | 17.07 | 18.57 | 13.99 | 14.72 | 11.14 | 12.75 | 15.93 | 15.17 | 16.20 | 17.43 | 18.91 | 20.77 |
| Repaired | 10.90 | 11.20 | 8.46 | 9.13 | 6.60 | 7.65 | 16.24 | 16.08 | 19.03 | 18.32 | 22.90 | 23.71 |
| p | P=0.47 | p=0.59 | P=0.23 | P=0.93 | P=0.97 | P=0.45 | ||||||
Today’s technical improvement theme for ACL reconstruction certainly includes the double bundle proposal1–8,11–13. Recently, there has been a tendency towards the “anatomical double bundle reconstruction” technique with four bone tunnels, of which two are in the femur and two are in the tibia.5,11–13
The superiority of the double bundle technique in the literature is questionable as some authors have found similar results when comparing it with the single bundle technique15,16,19, while others have found better results with the double bundle method.13,14
In 1999, Edwards20 showed the influence of the amount of graft on double bundle ACL reconstruction results, and questioned the real advantage of this technique. It is possible that the better double bundle results found in some publications13,14 stem from this facet.
In light of these studies, we present a direct biomechanical comparison between single and anatomical double bundle ACL reconstructions with the same total amount of bone-patellar tendon-bone graft. One of the reasons for the patellar graft choice was the possibility of exact division into two equal parts. The other reason was to avoid overstraining of the bundles, a problem documented by Miura21 in 2006 for hamstrings grafts.
One difficulty of double bundle technique execution was the femoral guide location on the tibial tunnel. As such, it was alternatively introduced through the anteromedial portal in two specimens.
Our results showed no differences between the two techniques for any of the measurements. This does not necessarily mean that the two techniques are similar under clinical conditions, as testing was limited to a non-cyclical loading biomechanical comparison (limited by our conventional tensile tester) on cadaveric specimens, which evaluated only immediate biomechanical results under experimental conditions. However, we could compare the results with the “intact condition” parameters (not possible in patients), concluding that both techniques could not restore them completely but have the same capacity to improve the “lesioned condition” parameters.
CONCLUSIONSReconstructions of anterior cruciate ligaments with the anatomical double bundle technique and with the conventional single anterior medial bundle technique with the same amount of bone-patellar tendon-bone graft have similar initial biomechanical behaviors with regard to anterior tibial dislocation, rigidity and passive internal tibial rotation.