Declines in cognition and mobility are frequently observed in the elderly, and it has been suggested that the appearance of gait disorders in older individuals may constitute a marker of cognitive decline that precedes significant findings in functional performance screening tests. This study sought to evaluate the relationship between functional capacities and gait and balance in an elderly community monitored by the Preventive and Integrated Care Unit of the Hospital Adventista Silvestre in Rio de Janeiro, RJ, Brazil.
METHODS:Elderly individuals (193 females and 90 males) were submitted to a broad geriatric evaluation, which included the following tests: 1) a performance-oriented mobility assessment (POMA) to evaluate gait; 2) a mini-mental state examination (MMSE); 3) the use of Katz and Lawton scales to assess functional capacity; 4) the application of the geriatric depression scale (GDS); and 5) a mini-nutritional assessment (MNA) scale.
RESULTS:Reductions in MMSE, Katz and Lawton scores were associated with reductions in POMA scores, and we also observed that significant reductions in POMA scores were present in persons for whom the MMSE and Katz scores did not clearly indicate cognitive dysfunction. We also demonstrated that a decline in the scores obtained with the GDS and MNA scales was associated with a decline in the POMA scores.
CONCLUSIONS:Considering that significant alterations in the POMA scores were observed prior to the identification of significant alterations in cognitive capacity using either the MMSE or the Katz systems, a prospective study seems warranted to assess the predictive capacity of POMA scores regarding the associated decline in functional capacity.
The percentage of elderly people in the general population has steadily increased throughout the last century (1). At the start of the 20th century, this increase occurred mainly in countries that today are considered socio-economically developed. As a result, most of these countries currently have a considerable proportion of their population above the age of 65 (1). More recently, this increase has been associated with an increase in the socio-economic status of developing countries (2). For instance, it is expected that Brazil will have a geriatric population of more than 14% of the general population by 2025, with approximately 33.4 million elderly people (3). Moreover, this aging population trend will undoubtedly continue, as most of the world's population lives in countries with low to moderate socio-economic status. Therefore, delivering proper care to this increasingly older population is and will continue to be a serious challenge, and the development of strategies to preserve the functional capacity of the geriatric population is therefore of paramount importance. Early identification of cognitive decline may constitute one such strategy, although to date, no effective and long-lasting methods for averting senility have been devised (4). However, early medical, behavioral and social intervention does improve clinical outcomes, which indirectly justifies the need for better screening methods (4). Improvements in clinical outcomes may offer the opportunity for a better quality of life, both for the elderly population and their caregivers (relatives and/or hired professionals).
The loss of functional capacity is closely linked to dementia, which is defined as a persistent and progressive loss of cognitive function in two or more domains (attention, memory, language, visuospatial skills and executive function) that interferes with the ability to perform the basic and instrumental activities of daily living (5). The main causes of dementia are related to Alzheimer's (55%–77%) and vascular diseases (15%–25%) (6). Dementia can have a deleterious impact on other aspects of health in the elderly; for instance, mood disorders and malnutrition are more frequent in dementia patients than in cognitively unimpaired individuals (7). In older individuals, falls are not only considerably more frequent than in younger people but also constitute a major health problem with a significant psychological impact and a higher risk of serious injury (7,8). Accidents are the fifth most common cause of death in the elderly, of which falls are responsible for 2/3 of all deaths (9). Approximately 1/3 of the elderly population 65 years of age or older living in non-residential care facilities will suffer at least one fall per year, and this number doubles for those over 80 years of age (8). Gait and balance disorders associated with normal and pathological aging increase the frequency of falls and dependency (10). In fact, such disorders are found in 20-40% of elderly individuals aged 65-84 years and in 40-50% of those aged 85 or older (11).
Motor control disorders may share relevant pathophysiological aspects with cognitive disorders (11), which may be due to the fact that human motor control is intimately associated with the functioning of the CNS (12). This association warrants further investigation into how a reduction in the functional capacity of the elderly, whether the result of normal or pathological aging, would reflect a reduction in motor control and as a consequence, an increased risk of falling.
It is often difficult to differentiate normal aging (senescence), which is characterized by natural physiological alterations, from pathological aging (senility), which is associated with illnesses that can affect quality and length of life (13). The need to differentiate senescence from senility has led to the creation of guidelines for clinical decisions, such as diagnoses, treatment and follow-up, which differ considerably between young patients and the elderly (14). Motor control related to gait and balance is highly dependent on the integrity of the CNS, and gait and balance disorders may be significantly associated with declining functional capacity in the elderly. Therefore, in the present study, we compared the results obtained with the use of the performance-oriented assessment of mobility problems (POMA) test in elderly patients to several parameters used for the assessment of functional capacity in elderly subjects. The objective of the current study was to examine the potential association between gait and balance disorders and functional alterations of senescence and senility.
MATERIALS AND METHODSThe initial sample consisted of 353 elderly patients who were routinely followed up at the Preventive and Integrated Care Unit (UIP) of the Hospital Adventista Silvestre (HAS) in Rio de Janeiro, Brazil. The study was approved by the Ethics Committee of HAS (protocol number: 20307/2007), and all procedures were carried out in accordance with the Declaration of Helsinki. Prior to participation in the study, all patients signed an informed consent form (ICF). The inclusion criteria were as follows: 1) patients followed at the UIP; 2) agreement to participate in the study and completion of the ICF; 3) patients between 65 and 95 years of age; 4) ability to participate in the tests used in the study; and 5) scores ≥22 on the mini-mental state examination (MMSE) test. The exclusion criterion consisted of the presence of any illness that could represent a risk to the subject's health during the functional assessments, especially those associated with walking and standing upright. In particular, subjects reporting dizziness or altered vestibular function at the time of the initial physical examination or immediately prior to the functional assessment were not tested with the performance-oriented assessment of mobility problems in elderly patients (POMA) and therefore were not included in the final sample.
All participants were subjected to a comprehensive geriatric assessment, which consisted of two home visits. During the first visit, the patient's history was recorded, a physical examination was performed, and the patient signed the ICF. During the second visit one week later, the functional assessment was performed using POMA. This instrument, which is specifically used to evaluate gait and balance problems in the elderly, was originally developed by Mary E. Tinetti in 1986 (15). The patient assessment was divided into two parts; the first part contained nine items related to balance, and the second part was composed of seven items related to gait. The scores ranged between 0 and 28, and lower scores indicated greater deficiencies. Scores below 26 were suggestive of deficiency, and scores less than 19 indicated a fivefold increase in the risk of falling. The functional assessment of the patients was also performed using the mini-mental state examination (MMSE) (16), which is an instrument commonly used as a screening test in the assessment of cognitive deficiencies. The potential scores ranged between 0 and 30, and a score less than 26 indicated the possibility of dementia. Moreover, the Katz scale (17) was used to evaluate the capacity of the elderly to undertake basic activities in daily life. This scale measured scores between 0 and 6; scores of 5 or 6 indicated independence in these activities, whereas scores of 3 or 4 indicated partial dependency and scores less than 3 indicated dependency. In addition, the Lawton scale (18) was used to measure the capacity of the elderly to undertake the instrumental activities of daily living. These scores ranged from 9 to 27, and lower scores indicated greater dependency. The geriatric depression scale (GDS) (19) was used to measure depression in the elderly. These scores range from 0 to 15; scores from 0 to 5 were considered normal, whereas scores from 6 to 10 suggested a slight disruption in mood, and any result above 11 indicated significant alteration. Last, the mini-nutritional assessment scale (MNA) (20) was used to evaluate nutritional alterations in the elderly. These scores ranged from 0 to 14, and a result of less than 12 indicated potential nutritional deficiencies.
For the statistical analyses, Kolmogorov-Smirnov one-sample (K-S) tests were initially used to assess the normality of the distributions. Kruskal-Wallis H (K-W) tests and Mann-Whitney U (M-W) tests were used to assess differences between the groups. Kendall tau-b (τ) tests were used to assess the degree of association between two variables, and chi-squared (χ2) tests were used to compare proportions between the groups. Significance was assigned at the level of p<0.05.
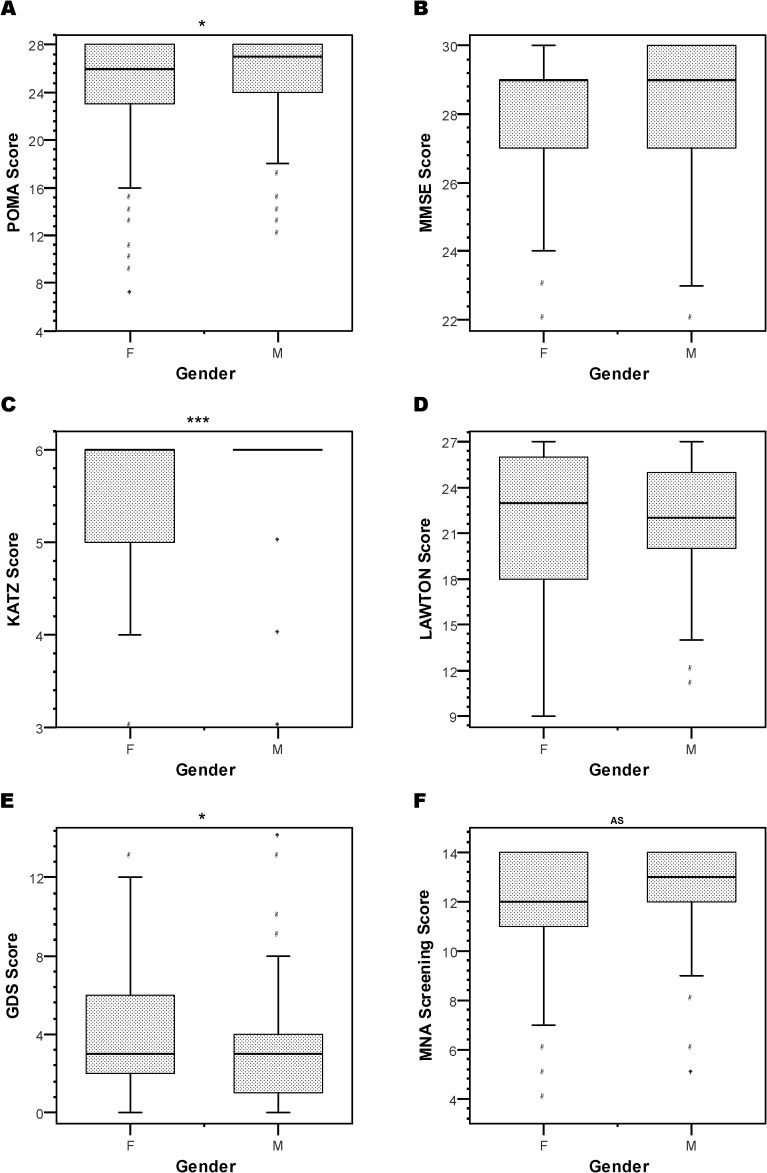
RESULTSThe final patient sample consisted of 90 (31.8%) men and 193 (68.2%) women with the following age distribution: 16 men and 54 women between 65 and 74 years of age; 50 men and 102 women between 75 and 84 years of age; and 24 men and 37 women between 85 and 95 years of age. No significant differences were observed between the men (79.6±0.6 years) and women (78.9±0.5 years) regarding mean age (t = 0.87, p>0.10) or the percentage of individuals with more than eight years of schooling (χ2 = 1.0, gl = 1, p>0.05; H = 88.8%, M = 84.2%). In addition, no significant differences were found between the men and women concerning the results obtained with the MMSE, Lawton and MNA scales (M-W: p>0.05 in all comparisons) (Figure 1). However, male patients demonstrated better scores than female patients regarding the POMA (M-W: Z = 2.1, p = 0.038), KATZ (M-W: Z = 4.4, p<0.001) and GDS (M-W: Z = 2.2, p = 0.029) scales (Figure 1).
Graphs depicting the effects of gender on the POMA (A), MMSE (B), Katz (C), Lawton (D), GDS (E) and MNA (F) scores. Note that women performed more poorly than men, as measured using the POMA, Katz and GDS assessment instruments. F: females; M: males; AS: 0.10>p≥0.05; * p<0.05; *** p<0.001.
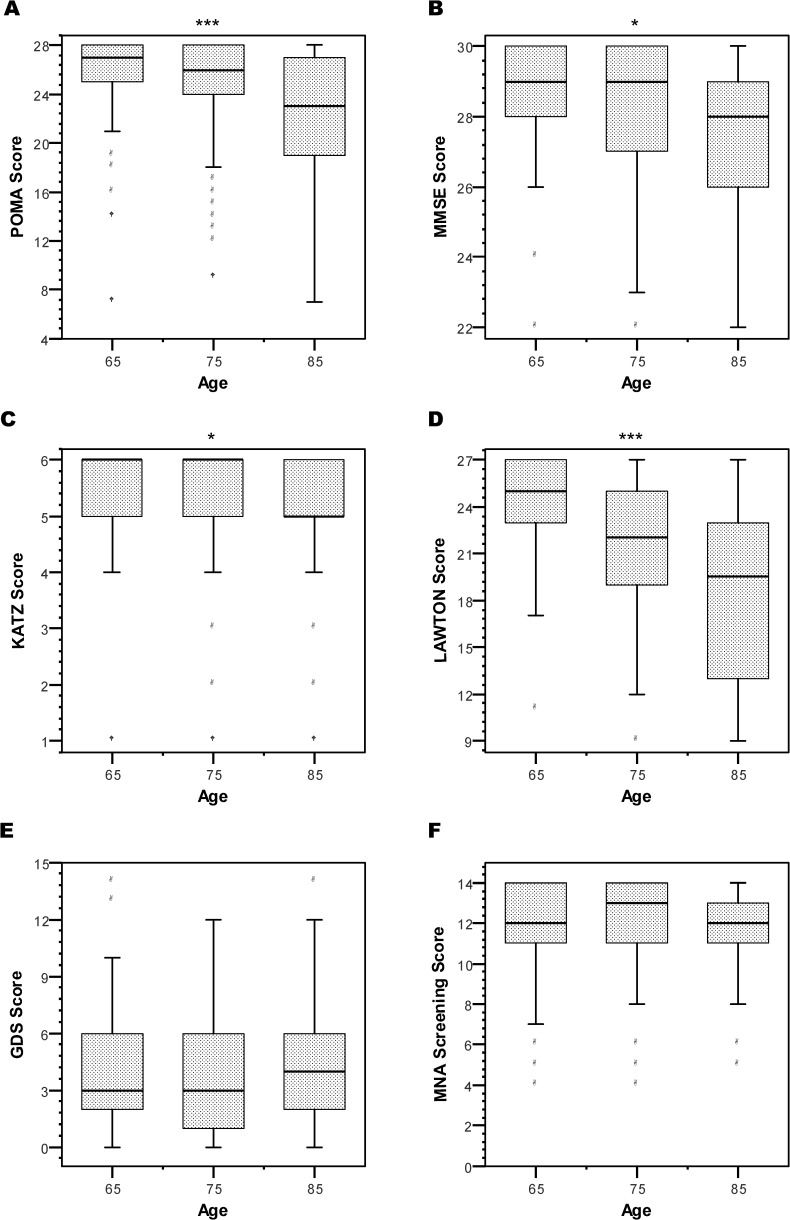
Analyses of the Kendall's correlation coefficients indicated significant associations between age and the scores obtained with the POMA (τ = -0.19, p<0.001), MMSE (τ = -0.13, p = 0.004), KATZ (τ = -0.13, p = 0.008), LAWTON (τ = -0.28, p<0.001) and MNA (τ = -0.09, p = 0.038). However, these coefficients were very low, and age was not considered to be a factor in the subsequent analyses. As shown in Figure 2, significant reductions in the scores were identified with increased age for the following variables: POMA (K-W: χ2 = 19.4, gl = 2, p<0.001), MMSE (K-W: χ2 = 9.0, gl = 2, p = 0.011), KATZ (K-W: χ2 = 9.0, gl = 2, p = 0.011) and LAWTON (K-W: χ2 = 22.1, gl = 2, p<0.001). In addition, the pairwise comparisons and the stratification of individuals according to age and functional capacity according to the various assessment instruments are shown in Table 1.
Graphs depicting the effects of age on the POMA (A), MMSE (B), Katz (C), Lawton (D), GDS (E) and MNA (F) scores. Note that performance declined as a function of increasing age when the POMA, MMSE, Katz and Lawton assessment instruments are used. 65: from 65 to 74 years old; 75: 75 to 84 years old; 85: from 85 to 95 years old; * p<0.05; *** p<0.001.
Age effects on functional scores.
| Assessment | K-S | Pairwise | M-W | Age | % of subjects | χ2 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| instruments | comparisons | Group | per score range | |||||||
| POMA | *** | 65 vs. 75 | # | 7-19 | 20-25 | 26-28 | ||||
| 65 vs. 85 | *** | 65-74 | 9% | 11% | 80% | *** | ||||
| 75 vs. 85 | *** | 75-84 | 9% | 20% | 72% | |||||
| >84 | 25% | 30% | 46% | |||||||
| MMSE | * | 65 vs. 75 | * | 22-25 | 26-30 | |||||
| 65 vs. 85 | ** | 65-74 | 3% | 97% | * | |||||
| 75 vs. 85 | 75-84 | 12% | 88% | |||||||
| >84 | 16% | 84% | ||||||||
| KATZ | * | 65 vs. 75 | 0-2 | 3-4 | 5-6 | |||||
| 65 vs. 85 | ** | 65-74 | 1% | 1% | 97% | ** | ||||
| 75 vs. 85 | * | 75-84 | 3% | 6% | 91% | |||||
| >84 | 13% | 7% | 80% | |||||||
| LAWTON | *** | 65 vs. 75 | ** | |||||||
| 65 vs. 85 | *** | |||||||||
| 75 vs. 85 | ** | |||||||||
| EDG | ns | 11-15 | 6-10 | 0-5 | ||||||
| 65-74 | 4% | 28% | 68% | ns | ||||||
| 75-84 | 3% | 23% | 74% | |||||||
| >84 | 3% | 27% | 70% | |||||||
| MAN | ns | 0-11 | 12-14 | |||||||
| 65-74 | 31% | 69% | ns | |||||||
| 75-84 | 27% | 73% | ||||||||
| >84 | 36% | 64% | ||||||||
K-S: Kruskal-Wallis test; M-W: Mann-Whitney test; χ2: Chi-Squared test; ns: non-significant; # 0.10>p≥0.05; * p<0.05; ** p<0.01; *** p<0.001.
The analysis of the correlation coefficients obtained for the various assessment instruments used in the functional evaluation of the elderly indicated that the POMA scores presented significant correlations with the scores obtained using all other instruments. Particularly, the POMA-KATZ correlation (τ = 0.38, p<0.001) and the POMA-LAWTON correlation (τ = 0.44, p<0.001) were significantly larger than the others. In general, these correlations indicated that declines in the results obtained with the POMA were associated with declines in the results obtained with the other instruments (Figure 3).
As shown in Figure 4A, the percentage of elderly individuals with a normal POMA score (≥26) as well as a normal MMSE score (≥26) was significantly greater (χ2 = 12.3, p = 0.002) than the percentage of elderly individuals with a normal MMSE score and a POMA score ≤19. When the analysis was performed considering only the normal MMSE scores (between 26 and 30), the percentage of elderly persons with a result indicating an abnormality increased significantly (χ2 = 17.4, p = 0.026) as the MMSE score decreased (Figure 5A).
The percentage of elderly individuals with a normal POMA score as well as a normal KATZ score (≥5) was significantly larger (χ2 = 91.4, p<0.001) than the percentage of elderly persons with a normal KATZ score and a POMA score ≤19 (Figure 4B). When the analysis was performed only among individuals with normal KATZ scores (5 and 6), the percentage of elderly individuals with abnormal POMA scores was not significantly affected by decreases in the KATZ score (Figure 5B) (χ2 = 4.7, p = 0.097).
Figure 4C shows that the percentage of elderly persons with normal POMA scores and normal GDS scores (≤5) was significantly greater (χ2 = 18.0, p = 0.001) than the percentage of elderly persons with normal GDS scores and POMA scores ≤19. As shown in Figure 5C, when the analysis was performed only among individuals with normal GDS results (between 0 and 5), the percentage of elderly individuals with abnormal POMA scores increased significantly (χ2 = 9, p = 0.049) as the GDS scores increased.
Finally, as shown in Figure 4D, the percentage of elderly persons with a normal POMA score as well as a normal MNA score (≥12) was significantly greater (χ2 = 18.9, p<0.001) than the percentage of elderly persons with a normal MNA score and a POMA score ≤19. When the analysis was performed only among individuals with normal MNA scores (between 12 and 14), the percentage of elderly persons with an abnormal POMA score significantly increased (Figure 5D) (χ2 = 14.5, p = 0.006) as the MNA scores decreased.
DISCUSSIONMethodological aspectsOne of the prominent characteristics of our sample was the inclusion of more women than men. Interestingly, the proportion of men per age group increased as the total age increased, and the higher overall number of females in our sample may reflect the fact that women tend to live longer than men (21). However, given the increase in the proportion of males with increasing age in our sample, the most likely explanation for the observed differences is behavioral. Females are accustomed to being routinely examined by physicians (such as gynecologists), and women have been shown to pay more attention to their health than men (21). As a result, women would be expected to be more actively engaged in the activities of the Preventive and Integrated Care Unit than men, especially at younger ages. In contrast, men typically become more interested in the advantages of preventive activities later in life when health problems become more prevalent; as a result, the proportion of men in our patient sample would be expected to increase with increasing age.
Our sample had a high socioeconomic and educational level (data not shown), as more than 80% of our sample completed high school. Although studies using Brazilian subjects have suggested a MMSE cutoff score of 24 (22), we used a score of 26 as a cutoff point, as this value is frequently used in the USA and Europe. We also excluded elderly patients with a MMSE score of less than 22 due to the reduced number of subjects with such scores in our initial sample and because these scores would have compromised the quantitative analyses.
Gender and age effectsIn the present study, we did not observe significant gender effects regarding the scores obtained with the MMSE, Lawton and MNA instruments. Previously, educational level was shown to be a factor in the definition of cutoff scores for instruments such as the MMSE (16,20). Elderly Brazilian men tend to have higher levels of education than women, and this trend is often accentuated in lower income classes, which comprise most of the Brazilian population (23). As previously indicated, however, our sample was comprised of individuals with higher educational and socioeconomic levels, which may explain the absence of gender differences. On the other hand, gender effects were observed in regards to the results of the POMA, Katz and GDS instruments, and these findings are in agreement with the current literature. For instance, the higher POMA scores among men in our sample likely reflected the fact that men of all ages engage in more physical exercise, have higher muscle mass and suffer fewer falls than women (24). Moreover, the lower average Katz scores observed among women were likely due to the increased prevalence of urinary incontinence (a significant component of the Katz score) that has been reported for elderly women (17). Finally, the higher GDS scores observed for women likely reflect the fact that females are more prone to depression than males, as the European prevalence of depression in the elderly is 14.1% for women and 8.6% for men, according to the EURODEP (25).
Regarding age effects, our results indicate that the scores derived from the POMA, MMSE, Katz and Lawton instruments show a decline with increased age, which is also in agreement with the literature. Several studies have shown that aging is associated with a progressive reduction in functional capacity that eventually leads to death (26). Interestingly, the GDS and MNA scores were not significantly affected by aging. Although there is currently no clear explanation for these last two findings, it is possible that the higher socioeconomic level of our sample explains, at least in part, the absence of age effects regarding these instruments. Generally, our subjects were closely monitored by their families and physicians, which suggests that depressive states, particularly moderate to severe ones, would likely have been identified and treated, and the same reasoning could be applied regarding undernourishment. In addition, there are well-established treatment protocols for depression and undernourishment (27,28), and both health problems can usually be corrected. Conversely, there are currently no treatments that can fully reverse the cognitive decline associated with senility (5). In this sense, the number of elderly individuals with cognitive deficits (which directly affects the POMA, MMSE, Katz and Lawton scores) tends to accumulate with age. However, the same trend is not necessarily true regarding the number of individuals with depression and/or undernourishment, which affects the GDS and MNA score, respectively.
POMA in the context of a comprehensive geriatric assessmentAging leads to the loss of functional reserves for dealing with situations that demand additional resources, such as those involving cognition, motor performance, immune response and endocrine function (13). Under normal conditions, these reserves are not used, and a reduction or even the absence of these reserves should not have a relevant impact on an individual's daily life. However, reductions in these functional reserves indicate an increase in fragility, given that these resources will not be available in situations of increased demand (29). As a result of the absence of significant effects on routine tasks, it is difficult to identify the loss of functional reserves. This is unfortunate because an identifiable loss of reserves could constitute advanced warning for impending health problems that could be better dealt with during early stages, especially in the elderly population (29). Therefore, the development and use of assessment instruments to identify subtle changes in the functional capacity of elderly patients is of great importance. Walking involves complex and continuous strategic planning by the central nervous system and involves aspects pertaining to the individual as well as the environment (30). Walking competently and safely is a task that demands adequate sensory-motor function, an efficient interaction between executive control (integration and decision making) and cognition (navigation, visual-spatial perception and attention) and an affective dimension (mood, preoccupation and risk-taking) (30). Given the demands that walking poses on the nervous system, it is likely that patients with cognitive impairments also present problems in their ability to walk. In fact, one initial sign of neurologic disorder is when individuals with cognitive impairments have difficulties in maintaining a conversation while walking (“stop walking while talking”) (31). This sign has also been used as a predictor of future falls, which further demonstrates the relationship between cognition and gait (31). Furthermore, executive frontal function is particularly important in maintaining a stable gait, and executive dysfunction may actually explain falls from idiopathic causes in elderly subjects (32). Moreover, there is a significant correlation between executive function, working memory and gait velocity in the elderly, particularly those with mild cognitive impairment (33). These associations suggest that cognitive and motor functions share a neural substrate, and this hypothesis has been corroborated by neuroimaging studies showing that tasks demanding these functions lead to increases in the activity of brain areas such as the prefrontal and parietal cortices, the cingulate gyrus and premotor areas (34).
In addition, our results corroborate these previously documented observations. By comparing the results obtained with the POMA to those obtained with the MMSE, Katz and Lawton scales, our results strongly suggest that a decline in functional capacity related to gait and balance is associated with a decline in cognitive capacity. In particular, it was observed that significant reductions in the POMA scores were present even for MMSE and Katz scores that would not be considered significantly altered. The POMA could thus serve as an early indicator of a cognitive decline that is unable to be detected by the most commonly employed screening instruments, particularly in populations with higher levels of education. Despite this promising and relevant possibility, a longitudinal prospective study is warranted to unequivocally demonstrate under what circumstances the use of the POMA instrument is valid as an indicator of cognitive integrity in the elderly. For example, patients suffering from severe arthritis or those who have significant lesions in the spinal cord or peripheral nerves may have normal cognitive capacity in addition to a significantly altered POMA score.
In the present study, we evaluated two potential confounding factors regarding the use of the POMA score as an additional source of information on cognitive integrity in the elderly. Affective disorders are commonly associated with gait impairment in patients belonging to this age group. Depression, anxiety and, in particular, a fear of falling are common among elderly individuals with an insecure gait and a previous history of falling (12). Furthermore, our results show that declines in the GDS scores are associated with reduced POMA scores. Depression is frequently observed in cases of dementia, as 25% of dementia patients present clear symptoms of depression, and dementia is an independent risk factor for early institutionalization (35). Moreover, it is relatively common for dementia to be initially identified as depression (36). Considering the relationship between cognitive function and the POMA and GDS scores, we cannot disregard the possibility that depressive state, as identified using the GDS, may serve as a marker of cognitive impairment, which in turn may have been the true cause for the decline in the POMA results. Both severe and mild depression can alter the functional capacity of the elderly and aggravate associated chronic illnesses (36). Patients with mild depressive disorders present an elevated risk of developing disabilities, which may lead to more severe depression (37). Furthermore, elderly subjects with normal cognition and mild to moderate depressive symptoms present a twofold increase in the risk of presenting mild cognitive decline over a period of six years, and this change is independent of associated vascular illness, which suggests that depressive symptoms could be considered a risk factor for the onset of cognitive impairment (38).
Our results for the mini-nutritional assessment scale (MNA) were also associated with changes in POMA scores. Understandably, the loss of functional reserves brought about by aging becomes even more evident in the presence of an inadequate diet (28,29). In addition to the direct effects on muscular action, malnutrition interferes directly with the activity of the nervous system (12). Therefore, malnutrition in the elderly may affect both gait and balance as a result of both muscle weakness and the inability of the brain to deal with the associated sensory-motor and cognitive demands. Furthermore, nutritional status becomes particularly critical in patients with cognitive impairments, given that these individuals become progressively more dependent on others to perform the basic activities of daily life, such as feeding oneself (28). Two of the six items in the MNA assessment are not related to the somatic or nutritional characteristics of the individual but are instead related to their capacity for maintaining independence and intact cognition (20). Therefore, future studies must differentiate the direct effects of nutritional status on the POMA scores from the effects of the cognitive impairments that are relevant to the MNA assessment score and that could negatively affect both POMA and an individual's nutritional status.
It remains unclear what the effect of normal aging (senescence) is on gait and whether all normal aging elderly individuals experience gait disorders. Although it was once assumed that difficulties related to gait would be unavoidable with the passing of time, in has been demonstrated in recent years that more than 20% of very old individuals (older than 88 years of age) present a normal gait, which suggests that gait impairments are not a consequence of normal aging (senescence) (39). This assumption is further supported by the fact that individuals with senile gait have an increased risk of developing dementia and a lower survival rate when compared to elderly people who walk normally (40). We therefore have reason to believe that gait impairments may represent early manifestations of subclinical diseases affecting the central nervous system in elderly patients.
Gait and balance are intimately associated with the functioning of the nervous system. Although gait and balance are directly linked to the motor nervous system, disorders that affect components of the nervous system involved with cognition can also have negative repercussions on motor control. In fact, we observed that a reduction in the MMSE, Katz and Lawton scores (the three scales of functional evaluation in the elderly that involve cognitive aspects) was associated with a decline in the POMA scores. In particular, we demonstrated that significant reductions in POMA scores could be identified prior to the detection of cognitive impairment using the MMSE and Katz scores, and we also found that increased susceptibility to depression and malnutrition were associated with reduced POMA scores. Given these observations, the performance-oriented assessment of mobility problems in elderly patients (POMA) should be used in conjunction with other instruments that assess the functional status of the elderly, not only as a measure of motor performance, but also as a potential marker of cognitive status. In fact, the presence of alterations in POMA scores may be considered an early indication of cognitive decline.
AUTHOR CONTRIBUTIONSBoth authors contributed equally to the study.
The authors would like to thank Mirtes Ester Ferreira, Nilza Veiga Ferreira, Tereza Cristina Martins, Luciana Mescolin, Marta Gomes, Esther Bando, Dr. Rogério Gusmão and all the patients who participated in this study.
No potential conflict of interest was reported.