Hip fractures are associated with high levels of co-morbidity and mortality. Orthogeriatric units have been shown to be effective with respect to functional recovery and mortality reduction. The aim of this study is to document the natural history of early multidisciplinary intervention in elderly patients with hip fractures and to establish the prognostic factors of mortality and walking ability after discharge.
METHODS:This observational, retrospective study was performed in an orthogeriatric care unit on patients aged ≥70 years with a diagnosis of hip fracture between 2004 and 2008. This study included 1363 patients with a mean age of 82.7±6.4 years.
RESULTS:On admission to the unit, the average Barthel score of these patients was 77.2±27.8 points, and the average Charlson index score was 2.14±2.05. The mean length of stay was 8.9±4.26 days, and the readmission rate was 2.3%. The in-hospital mortality rate was 4.7%, and the mortality rates at one, six, and 12 months after discharge were 8.7%, 16.9%, and 25.9%, respectively. The Cox proportional hazards model estimated that male sex, Barthel scale, heart failure, and cognitive impairment were associated with an increased risk of death. With regard to functionality, 63.7% of the patients were able to walk at the time of discharge, whereas 77.4% and 80.1% were able to walk at one month and six months post-discharge, respectively. The factors associated with a worse functional recovery included cognitive impairment, performance status, age, stroke, Charlson score, and delirium during the hospital stay.
CONCLUSIONS:Early multidisciplinary intervention appears to be effective for the management of hip fracture. Age, male sex, baseline function, cognitive impairment and previous comorbidities are associated with a higher mortality rate and worse functional recovery.
Hip fracture is a health problem that commonly affects the elderly. This condition carries a high rate of morbidity and mortality (1–3), is associated with a marked loss of mobility and function (4–5), and generates substantial medical and social costs. Approximately 350,000 hip fractures occur every year in the US (6), of which more than 90% occur in subjects over 65 years of age 7. In Spain, the population older than 65 years of age has been projected to increase from 15.5% in the year 1980 to 28.6% in the year 2025 (8), which represents an increase of 84.5%, and one of the consequences of aging is the high and increasing number of patients admitted for hip fracture (9). In our setting, hip fractures show an incidence of 614 cases per 100,000 admissions among patients over 64 years of age (10).
The joint care model of geriatricians and traumatologists was developed in the United Kingdom in the late 1950s. In 1974, Devas (11) described the functioning of the so-called orthogeriatric units, which are aimed at the care of the elderly urgently admitted to a hospital setting for hip fracture. A significant percentage of patients seen at these units show co-morbidity, cognitive impairment or meet frailty criteria. These hospital units attempt to provide continuous care to prevent intrahospital complications and improve the functional recovery of these patients. Orthogeriatric units are currently grouped into different functional models based on the degree of involvement of geriatricians, traumatologists and rehabilitation physicians (12). These models generally manage to reduce the average hospital stay, complications, readmissions and mortality rates generated at orthogeriatric units. In addition, these procedures have been shown to save costs to the health system. However, the functional recovery outcomes of such models have been heterogeneous (13–14). Of the models published, programs offering early, intensive geriatric care have been shown to be more effective for improving functional recovery and reducing hospital stays and mortality rates (14–17).
The objectives of this study are to evaluate the results of early, intensive multidisciplinary care and establish the prognostic factors for walking ability and mortality in the long-term.
MATERIAL AND METHODSStudy DesignThis study was an observational, analytical, and retrospective study.
Scope and populationThe Hospital Universitario de la Ribera is a hospital that manages the population from the region of La Ribera (Region of Valencia, Spain), which has 256,090 inhabitants, of whom 13.5% are older than 69 years of age. In the surgical area, geriatricians see all patients over 69 years of age who are admitted for hip fracture, For other diagnoses in the areas of traumatology, general surgery, vascular surgery, neurosurgery, and urology, a risk screening is performed based on the pre-anesthetic assessment regarding elective procedures or the co-morbidities, performance status and clinical condition of the patient at the time of his/her admission to urgent care.
PatientsThis study included all patients over 69 years of age who were admitted with a diagnosis of hip fracture between 1 January 2004 and 31 December 2008. The exclusion criteria included the presence of pathological fractures or terminal diseases and a life expectancy of less than six months.
InterventionFollowing the diagnosis of hip fracture upon hospital admission, each patient was assigned to a traumatologist, a geriatrician and a nurse team for the duration of his/her hospital stay. The geriatrician and traumatologist evaluated the patient during the first 24 hours and daily thereafter. After the surgical procedure, the rehabilitation department examined the patient and initiated rehabilitation therapy within the first 48 hours after surgery.
For the first evaluation, the traumatologist evaluated the patient and decided on the suitability of the surgical treatment and the technique to be used, and the geriatrician used a comprehensive geriatric assessment (CGA) that included an assessment of functional, cognitive and social issues. Furthermore, co-morbidities and the clinical condition of each patient were evaluated at the time of admission to establish a pre-operative treatment plan. For patients with a diagnosis of previous cognitive impairment or those with delirium at the time of the survey, data were obtained from the main care giver. When considered necessary by the geriatrician, the social worker examined the social network of the patient and advised on measures that could strengthen it upon discharge.
The decision for patient discharge was agreed upon by the traumatologist, geriatrician and rehabilitation specialist. When considered necessary, rehabilitation was continued after hospital discharge at reference rehabilitation sites.
This designed model attempted to provide early, integral care with an emphasis on early geriatric assessment, surgical procedure selection and the initiation of rehabilitation therapy to recover patient mobility in the shortest possible time following surgery.
Data collection and variables testedThe data were obtained from the electronic clinical history using SIAS© software (Ribera Salud II UTE, Alzira, Comunidad Valenciana, Spain). Once accepted by the Ethics and Research Committee of the hospital and after obtaining the patient's consent, the hospital records and discharge reports for those patients with a diagnosis of hip fracture during the study period were evaluated. The follow-up data were obtained from the records of outpatient services, emergency rooms, and hospital admission after discharge. The subjects with no follow-up data within the twelve months following discharge were contacted by phone. Therefore, information on survival and walking ability was obtained from the patient, relatives or care givers. These data were collected by two co-investigators who did not know the study design or its objectives.
Admission variablesThe sociodemographic variables collected included sex, age, marital status, social status, and living environment (rural or urban). The functional variables included the Barthel scale (18) for activities of daily living, previous walking ability (rated as independent, assisted [cane or walker], dependent or no walking), and the presence and degree of previous cognitive impairment according to the Reisberg Global Deterioration Scale (GDS) (19). The medical variables included a history of fractures, heart failure (HF) as diagnosed using the Framingham criteria (20), previous cerebrovascular disease (CVD), previous renal failure (RF), co-morbidity assessment using the Charlson index score (21), and previous medication history including the number of drugs taken by the patient. The perioperative medical complications documented included urinary infection, pneumonia, constipation, vascular disease, diagnosis of acute confusion syndrome (ACS) during the hospital stay using the Confusion Assessment Method (CAM) (22), receipt of blood transfusion(s), admission to ICU (Intensive Care Unit), and the total number of complications arising during the hospital stay. Other data that were collected included mortality, hospital length of stay, discharge location (home, residence or hospital-based home care), pre-surgical waiting time, type of fracture (subcapital, basicervical, pertrochanteric or subtrochanteric), surgical treatment applied and post-operative surgical complications (surgical wound infection, prosthesis dislocation and resurgery).
Variables after dischargeThe ability of the patients to walk was evaluated at one and six months after discharge. The recovery of walking was defined as the ability to walk a distance of more than five meters with or without assistance. Mortality was recorded at one month, six months, and one year after discharge. The presence of new fractures, failures of osteosynthesis during the subsequent year, and hospital readmissions (defined as admission to the same ICD within 30 days following discharge) were also recorded.
Data processing and analysisThe values for each of the variables were entered into an Excel table, version 2003, and the statistical analysis was performed using SPSS for Windows version 15.0 (SPSS Inc., Chicago, IL).
The categorical variables were described as percentages, and quantitative variables were expressed as the value of the mean with the standard deviation and 95% confidence interval. The bivariate analyses used Student's t-tests (Fisher method) for the comparison of means, Pearson's chi-square test and Mantel-Haenszel's linear trend for proportions and Pearson's correlation for quantitative variables. A p-value of less than 0.05 was taken as the threshold for statistical significance.
A multiple logistic regression model was built to study walking ability at one and six months after discharge. Survival was estimated using the statistical Kaplan-Meier method, and survival differences between groups were estimated using the Mantel-Haenszel test. The variables related to one-year mortality were tested using a Cox proportional hazards model, which was defined according to the deaths observed during the 365 days following the incidence of hip fracture. First, the full model was considered with all variables significantly associated with one-year mortality in the bivariate analysis. In a second step, any variable not causing an important change (defined as the absence of an adjusted effect of more than 10%) or not improving the standard error of the estimation upon adjusting the model without this variable was removed from the model. Agreement between the investigators was used in cases where two or more subsets of variables were obtained with a similar degree of adjustment.
RESULTSA total of 1363 patients were included during the study period, and 75.7% of these patients were women. The mean age of the patients was 82.6±6.4 years. No significant differences were found concerning the living environment of the patients (rural or urban).
The mean score on the Barthel scale at admission was 77±27 points; of the total patients, 40.5% had a score >94 points, 46.6% had a score from 40 to 94 points, and 12.8% had a score ≤39 points. With respect to walking, 88.2% could walk independently or with technical assistance. The social variables indicated that 87.8% lived in the community, and 35.4% of the patients lived alone. The co-morbidity level of the evaluated population was high (Charlson score 2.1±2.1), and higher Charlson index scores were observed for men (2.4 vs. 1.8, p<0.000). The most common co-morbidities included hypertension (57%), cognitive impairment (30%), diabetes mellitus (25%), heart failure (19%), dyslipidemia (16%), previous stroke (14%), ischemic heart disease (9%), and heart failure (6%). Among all of the patients, 19% had suffered previous fractures. Male patients had a higher prevalence of ischemic heart disease (15.6% vs. 7.7%, p<0.001), stroke (19.9% vs. 11.8%, p<0.000), and renal failure (10.9% vs. 4.5%, p<0.001), whereas female patients had a higher prevalence of previous bone fracture (51.5% vs. 11.5%, p<0.0001). Prescriptions for calcium and vitamin D supplements were higher among women (7.8% vs. 3.9%, p<0.001), as were prescriptions for anti-resorption agents (4.1%, vs. 0.7%, p = 0.003). No differences were observed regarding the number of admissions by day of the week, month of the year, or quarter. Peri-trochanteric fracture was the most common type (52%) and was followed by subcapital (38%), subtrochanteric (8%), and basicervical fractures (2%). There were no differences between types of fracture according to the year of study or patient age or sex.
The average hospital stay was 8.9±4.3 days, and the hospital stay lasted more than 9 days in 32.7% of the patients. The mean surgical delay was 2.4±1.9 days and was longer than 48 hours for 37.5% of the patients. During their hospital stay, 18.4% of the patients experienced delirium. The mean number of the complications documented during the hospital stay was 1.3±0.6. After the surgical procedure, 40.2% of the patients required a blood transfusion. At the time of hospital discharge, 63.7% of the admitted patients had recovered their ability to walk. However, 65 patients (4.7%) died during their hospital stay. The causes of intra-hospital death included heart failure (27.7%), infectious disease (24.6%), vascular ischemic disease (21.5%), respiratory disease (15.4%), and other causes (digestive, renal; 10.8%). The re-admission rate was 2.3%.
MortalityIn the univariate analysis, age, male sex, the presence of cognitive impairment and post-surgical complications were significantly associated with a higher mortality rate during the hospital stay and at one month, six months and one year after hospital discharge (Table 1). At twelve months, single individuals had a higher mortality rate (33%) as compared to widowed (29.7%) or married patients (22.4%), p<0.02. At twelve months post-discharge, there was a significant difference in the mortality rate among patients with a longer length of hospital stay (9.6±5.1 vs. 8.8±3.8, p<0.02). Additionally, patients with an increased intake of prescription drugs prior to admission had a higher mortality one month (4.7±3.4 vs. 4.5±2.8, p<0.05), six months (4.8±3.6 vs. 4.4±2.8, p<0.05) and 12 months (4.8±3.5 vs. 4.2±2.7, p<0.001) after discharge. The mortality rate was also higher in patients with more complications at the time of hospital admission (1.6±0.9 vs. 1.1±0.4, p<0.05) or at one month (1.5±0.9 vs. 1.1±0.4, p<0.02), six months (1.5±0.8 vs. 1.1±0.4, p<0.02), and 12 months after discharge (1.4±0.7 vs. 1.1±0.4, p<0.03).
Univariate analysis comparing clinical variables and mortality.
| Variables | On discharge | One month | Six months | 12 months | ||||
|---|---|---|---|---|---|---|---|---|
| mortality | p-value | mortality | p-value | mortality | p-value | mortality | p-value | |
| Global | 65 (4.7%) | 118 (8.7%) | 231 (16.9%) | 353 (25.9%) | ||||
| Sex: Male Female | 7.6%3.9% | 0.006 | 13.8%6.2% | <0.001 | 29.3%15.0% | <0.001 | 39.6%23.1% | < 0.001 |
| Age | +5.3 | <0.001 | +4.0 | <0.001 | +3.3 | <0.001 | +3.4 | < 0.001 |
| Social status: Alone With partner With children Institutionalized | 4.5%3.4%6.2%6.0% | 0.319 | 6.9%6.3%9.6%10.2% | 0.231 | 15.0%14.8%22.8%26.8% | 0.001 | 22.2%20.3%34.7%42.1% | < 0.001 |
| Barthel Scale | -9.4 | 0.071 | -11.2 | 0.003 | -15.4 | <0.001 | -16.8 | < 0.001 |
| Previous walking: Autonomous Cane/crutch Walker Dependent Does not walk | 3.3%5.3%6.5%7.2%7.0% | 0.152 | 5.1%10.9%11.2%8.4%14.0% | 0.003 | 13.1%21.7%30.0%24.5%27.8% | <0.001 | 20.3%31.9%36.5%42.4%47.2% | <0.001 |
| Charlson index | +0.3 | 0.192 | +0.5 | 0.025 | +0.4 | 0.007 | +0.5 | < 0.001 |
| Previous heart failure: Present Absent | 8.5%3.9% | 0.002 | 13.3%6.7% | <0.001 | 22.1%17.6% | 0.097 | 37.4%25.0% | < 0.001 |
| Cognitive impairment:PresentAbsent | 7.3%4.0% | 0.013 | 11.7%6.8% | 0.004 | 25.1%15.5% | <0.001 | 41.1%21.2% | < 0.001 |
| Degree of cognitive impairment:MildModerateSevere | 5.5%8.0%10.4% | 0.325 | 8.3%13.3%15.2% | 0.181 | 17.9%25.5%36.0% | 0.005 | 31.3%45.4%53.4% | 0.001 |
| Complications: Present Absent | 16.8%2.9% | <0.001 | 25.0%5.4% | <0.001 | 40.7%14.9% | <0.001 | 53.3%22.9% | < 0.001 |
| Delirium: Present Absent | 3.0%2.0% | 0.359 | 7.9%4.9% | 0.069 | 22.2%14.5% | 0.004 | 34.0%22.3% | < 0.001 |
| Transfusion: Present Absent | 3.1%3.2% | 0.975 | 8.3%5.1% | 0.019 | 22.0%13.1% | <0.001 | 32.2%21.6% | < 0.001 |
Data expressed as % or difference between means.
During the hospital stay, the average mortality rate was 4.7% and was associated with a history of heart failure. One month after hospital discharge, the cumulative mortality rate was 8.7% and was higher in patients with a lower Barthel index score, worse previous walking ability, higher co-morbidity score (Charlson index), and a greater need for transfusion during the hospital stay. At six months after discharge, the cumulative mortality rate was 16.9% and was associated with social status (institutionalization), a lower Barthel index score, worse previous walking, higher co-morbidity score (Charlson index), higher degree of cognitive impairment, greater use of drugs, hospital complications, the presence of delirium during the hospital stay, and a greater need for transfusions. At twelve months after hospital discharge, the cumulative mortality rate was 25.9% and was associated with marital status (greater percentage of bachelors), social status (institutionalization), lower score on the Barthel scale, worse previous functionality, higher co-morbidity score (Charlson index), presence of heart failure, higher degree of cognitive impairment, greater use of drugs, surgical complications, delirium, and the need for transfusions.
During the one-year follow-up period, the probability of surviving a hip fracture was 73% and was significantly lower in males (60% vs. 77%; p<0.001).
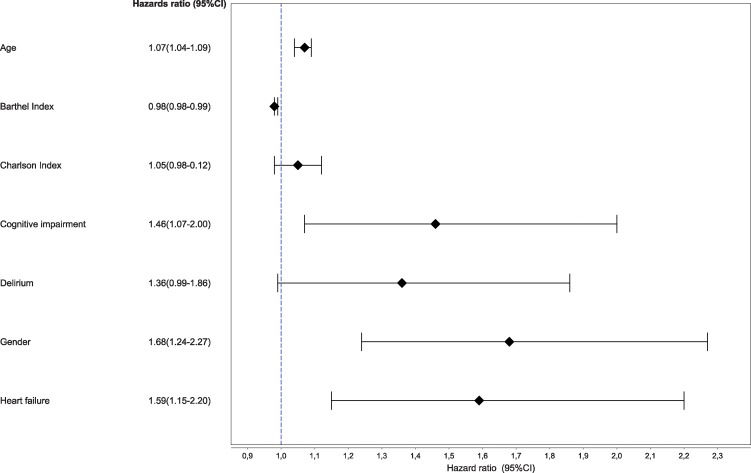
In a Cox proportional hazards model, the variables associated with a higher mortality rate after one year included the following: male sex (HR 1.683; 95% CI 1.245-2.275), age (HR 1.072; 95% CI 1.048-1.096), Barthel index score (HR 0.989; 95% CI 0.985-0.994), history of heart failure (HR 1.593; 95% CI 1.151-2.203), and the presence of cognitive impairment (HR 1.467; 95% CI 1.073-2.005) (Figure 1).
WalkingAt the time of hospital discharge, 63% of the patients were able to walk. The percentage of patients surviving at one month and walking was 77.4% and increased to 80.2% at six months. Of the 462 patients (36.3%) who were not walking at the time of discharge, 59.2% were able to walk at six months after discharge.
The data from the univariate analysis are shown in Table 2. The factors negatively associated with walking at both time points tested included functional (a low previous score on the Barthel scale, the ability to walk while dependent on another person and the absence of walking), cognitive (the degree of cognitive impairment and the presence of delirium during hospital stay), and social (institutionalized patients) variables.
Univariate analysis for variables associated with walking.
| On discharge | At six months | |||
|---|---|---|---|---|
| Variable | Percentage walking | Significance | Percentage walking | Significance |
| Sex: Male Female | 57.1%64.9% | 0.012 | 80.2%82.2% | 0.542 |
| Living with: Alone Partner Children Institutionalized | 68.4%70.6%60.7%37.7% | <0.000 | 82.0%84.4%79.1%61.6% | <0.000 |
| Previous walking: Autonomous Cane Walker Dependent Does not walk | 72.4%59.9%53.1%37.4%15.7% | <0.000 | 85.5%86.2%70.5%52.7%30.0% | <0.000 |
| Previous stroke: Present Absent | 60.8%63.2% | 0.555 | 73.1%81.6% | 0.029 |
| Previous HT: Present Absent | 65.6%59.4% | 0.023 | 82.3%77.8% | 0.090 |
| Previous cognitive impairment: Present Absent | 47.8%69.8% | < 0.000 | 64.4%85.8% | <0.000 |
| Degree of cognitive impairment: Mild Moderate Severe | 60.7%43.2%24.4% | <0.000 | 74.1%59.3%47.5% | 0.005 |
| Delirium: Present Absent | 46.3%66.8% | <0.000 | 65.5%83.4% | <0.000 |
| Previous Barthel score: Walking Not walking | 84.367.0 | <0.000 | 85.664.9 | <0.000 |
| Age: Walking Not walking | 81.883.5 | <0.000 | 81.482.1 | 0.184 |
| Charlson index: Walking Not walking | 2.12.3 | 0.075 | 2.12.4 | 0.087 |
Legend: ST: stroke; HT: hypertension, ICU: Intensive Care Unit.
For the univariate analysis at the time of hospital discharge, the factors negatively associated with walking ability included demographic factors (male sex), co-morbidity factors (hypertension and previous diagnosis of bone fracture: -56.4% in patients unable to walk vs. 35.9% in walking patients, p<0.03), complications (52.8% vs. 35.5%, p<0.001), and the need for an allogenic blood transfusion during the hospital stay (55.3% vs. 21.8%, p<0.001).
At six months after discharge, the only variable negatively associated with walking ability that did not show significance at the previous cutoff point was a previous diagnosis of stroke.
Admission rates to the ICU were significantly different between patients unable to walk (41.7%) and those who could walk (19.1%) (p<0.05). There were no significant differences regarding age, sex, Charlson index score, the need for a blood transfusion or the prescription of anti-resorption agents or calcium and vitamin D supplements at the time of discharge between subjects who were able to walk after six months and those who were not. The values of the variables tested are shown in Table 2.
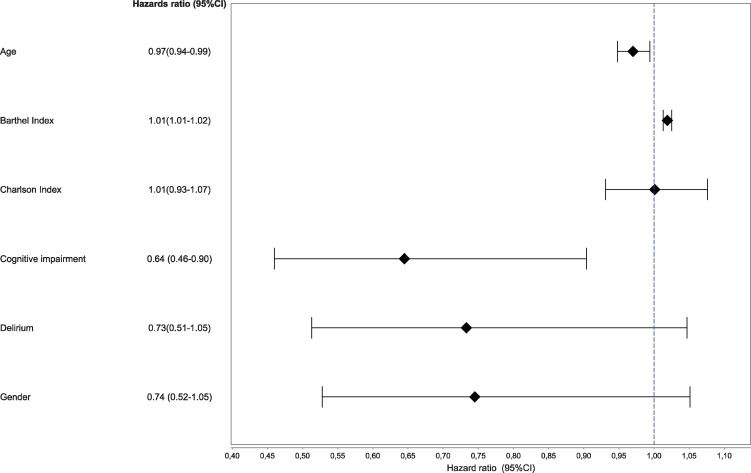
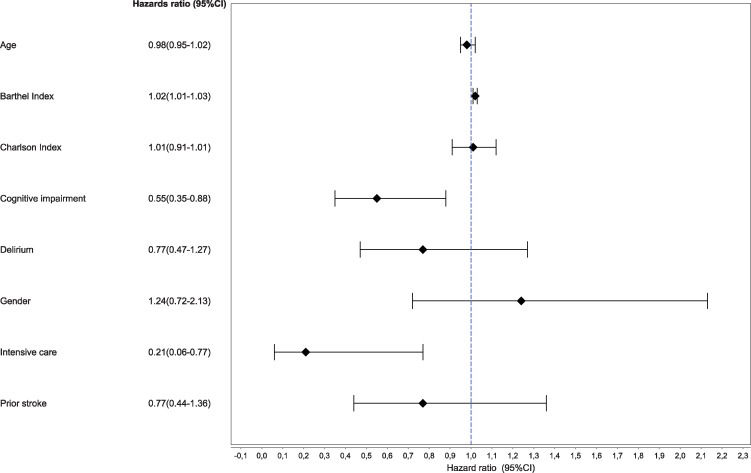
In the logistic regression analysis (Figures 2 and 3), walking ability at the time of discharge was associated with age (OR 0.97; 95% CI 0.94-0.99), Barthel scale (OR 1.019; 95% CI 1.013-1.025) and cognitive impairment (OR 0.64; 95% CI 0.46-0.9). At six months, walking ability was associated with a history of cognitive impairment (OR 0.557; 95% CI 0.351-0.884), admission to the ICU (OR 0.209; 95% CI 0.057-0.772) and the Barthel scale score (OR 1.024; 95% CI 1.016-1.032) but was independent of sex, age, previous stroke, Carlson index score, and the presence of delirium.
This study implemented a strategy of early multidisciplinary management and herein reported results concerning the functional recovery and mortality of patients with hip fracture. In these patients, mortality was mainly associated with age, male sex, previous functionality, heart failure, the Charlson index score, delirium, and cognitive impairment. The recovery of the ability to walk after the fracture was related to age, function, presence of cognitive impairment, and delirium. Our findings confirm certain previously published results, stress the importance of geriatric care for obtaining improved healthcare outcomes, and extend the knowledge of the risk factors associated with poor vitality and function.
The main limitation of this study was its retrospective case analysis design. Therefore, upon comparing the conclusions provided with those of other studies on the same subject, the differences in the design and organization of the various orthogeriatric units should be considered. The decision to evaluate walking ability at six months after hospital discharge was due to the similar results obtained at this time and at 12 months after follow-up. The losses after one year of follow-up constituted 3.1% of the cases, and these mainly involved patients from different hospital areas who happened to suffer a hip fracture while in the region of our hospital.
Joint medical care provided by geriatric and traumatology departments was first described in the year 1974 by Devas (11). Since this time, the scientific literature has not yet elucidated the optimal model of orthogeriatric care from the various orthogeriatric models described (12). In fact, one recent Australian review (23) highlighted the difficulties associated with drawing conclusions about the efficacy of a given model and suggested that an adequate geriatric monitoring process would generate only minor effects on the functional recovery, average stay, complications, and mortality rates of the patients involved.
Our study confirmed previous findings from other reports concerning the prevalence of various characteristics in patients with hip fractures. In fact, the current study described an average hospital stay similar to that published in another clinical trial evaluating the efficacy of this model (17). Additionally, the average hospital stay of the patients in our study was shorter than that published by other studies (24,25) and shorter than that from the data provided by the Spanish Ministry of Health (26) for public health hospitals over the period from 2004-2007 (19.6 days). The average cost of one day of stay at our hospital is estimated to be €167.5. Therefore, assuming a hospital stay in a range between 10.27 (27) and 19.6 days (26), a reduction of 356-2894 stays/year and a savings of €59,630-€484,758.4 per year can be obtained ($80.500-$654.453). These savings are similar to the annual $170,244 in savings estimated in another study (17). Some of these results may have been due to the short surgical waiting times and continued care, which did not present differences between patients admitted during the week and those during the weekend. In contrast, Anderson et al. (28) described a higher mortality rate among patients who were admitted during the months of July and August. This finding, which may be related to the holiday periods, was not reproduced in our study, and we believe this supports the efficacy of the medical care provided with our model.
Given the inherent comorbidities of these patients, we consider the rate of intrahospital complications obtained in our study to be low and consistent with patients receiving daily geriatric care. The beneficial effects of such care have been described by Incalzi et al. (15). Furthermore, the incidence of delirium found in our study was similar to the 16% obtained in a Brazilian study (29) that also used CAM as a screening tool.
The intrahospital mortality rate obtained in our study was slightly higher than that obtained in some previous studies (14,30) but was similar or even lower than those rates demonstrated in other studies (1,24,31). Finally, with regard to the quality of the medical care provided to patients with hip fracture, we believe that the low readmission rate in the current study, which was lower than those reported in previous studies (27,30,32), confirms the efficacy of our model.
The mortality rates of 16.9% and 25.9% at six and 12 months after hospital discharge, respectively, are consistent with results published in previous studies and reviews (7,33,36). However, as highlighted in some of these reviews (36,37), these values are independent from the presence or absence of geriatric departments in the hospitals studied.
One relevant point related to the medical care of these patients is the identification of variables associated with higher rates of mortality. In our sample, the variables associated with a higher risk of mortality were related to patient demographics (sex and age), function (Barthel scale score) and co-morbidities (cognitive impairment and heart failure).
In our series, as in other studies (2,34,38), male sex was associated with a higher risk of mortality, despite the average male age being younger than the average female age. Given the greater degree of co-morbidity seen in men, further research will be required to establish whether accurate control of these co-morbidities would improve the prognosis of these patients.
Heart failure was associated with increased early and late mortality, and heart failure has been shown to be the most common clinical condition in patients with hip fracture (2,34), regardless of patient sex (39). This increased mortality rate likely has a multifactorial origin, but according to heart failure clinical guidelines, early intervention (35) can improve the survival rates of these patients.
The presence of cognitive impairment was also associated with a higher mortality rate. As in our series, two other studies (41,42) have shown that cognitive impairment represents an independent factor for predicting mortality. However, in our study, we found a relationship between the presence of delirium during the hospital stay and mortality that almost reached statistical significance. These results are consistent with those of Julieb⊘ et al. (43), who did not find differences prior to adjusting for the presence of delirium and dementia. Furlaneto and Garcez-Leme (29,42) also did not find significant differences between delirium and mortality. Thus, the strict use of protocols for the prevention of delirium and the implementation of cognitive therapies could reduce the potential lethality associated with cognitive impairment.
In our study, each 10-point reduction in the Barthel scale score generated a mortality increase of 10%, which is a finding that has also been described by others (35). Thus, achieving a functional recovery approaching the pre-fracture baseline level may be associated with longer survival.
Age is a potent non-modifiable factor that can predict mortality, as described in numerous studies (34,41,44). This variable is typically related to the presence of chronic diseases. Because the Charlson index score predicted greater mortality in the multivariate analysis in our study, we believe that adequate control of chronic diseases in elderly patients could improve their prognosis and quality of life.
The risk of mortality associated with surgical delay has shown conflicting results in previous studies (34,40,44). In our series, surgical delay was not associated with higher mortality, which was likely due to the fact that the delay was short for the patients in our study. Additionally, in our study, blood transfusion was associated with increased mortality, which is consistent with a previous study (45). This finding is likely explained in part by the association between the need for transfusion and greater frailty and instability.
The percentage of patients able to walk after hospital discharge was high. The prognostic factors related to the recovery of walking ability included functional variables (Barthel scale), demographic variables (age), the presence of co-morbidity (delirium and cognitive impairment), and the occurrence of complications (post-surgical transfusion).
The Barthel scale score was the most potent factor related to the recovery of the ability to walk in our study. This result is consistent with that published by Burgos et al. (46), who studied six scales in 232 patients to correlate mortality and functional recovery and found that none of these scales were related to mortality and that only the Barthel index and the RISK-VAS were able to predict walking ability at 90 days. In addition to improving mortality rates, we believe that comprehensive rehabilitation not specifically focused on walking would improve the global function of patients after hospital discharge.
The second factor that was correlated with a worse ability to walk at six months after hospital discharge was age. Semel et al. (47) observed a greater functional recovery in younger patients, as the loss of function associated with age generally causes a worse functional condition. However, these functional losses can be recovered with more intensive therapies.
The presence of cognitive impairment and delirium was also related to a lower likelihood of walking. These findings are consistent with other published findings (48–49) and raise awareness for the importance of measures to prevent delirium and cognitive therapies, which would likely improve the functional recovery and mortality of patients at one year after hospital discharge.
In conclusion, early multidisciplinary care models are effective for the management of patients with hip fractures. However, establishing the factors that lead to increased mortality and worse functional recovery despite the efficacy of the model should help to improve the survival and quality of life of our patients.
AUTHOR CONTRIBUTIONSTarazona-Santabalbina, FJ and Belenguer-Varea, A conceived and designed the study and were responsible for the data collection, analysis, and interpretation and the preparation of the manuscript. Rovira-Daudi, E was responsible for the data analysis and interpretation and the preparation of the manuscript. Salcedo-Mahiques, E was responsible for the study design and data recruitment and collection. Cuesta-Peredó D was responsible for gathering data regarding the recruitment, mortality and hospital admissions of the patients. Doménech-Pascual, JR, Salvador-Pérez, MI and Avellana-Zaragoza, JA were responsible for the data recruitment and collection.
The authors would like to thank Concepción Bermell-González, MD for her collaboration in data collection and Elena Burdeos-Palau, from the Quality Management Department, for managing the SIAS software for access to the clinical histories of the recruited patients.
No potential conflict of interest was reported.