Mechanical ventilation with positive end expiratory pressure (PEEP) improves oxygenation and treats acute pulmonary failure. However, increased intrathoracic pressure may cause regional blood flow alterations that may contribute to mesenteric ischemia and gastrointestinal failure. We investigated the effects of different PEEP levels on mesenteric leukocyte-endothelial interactions.
METHODS:Forty-four male Wistar rats were initially anesthetized (Pentobarbital I.P. 50mg/kg) and randomly assigned to one of the following groups: 1) NAIVE (only anesthesia; n=9), 2) PEEP 0 (PEEP of 0 cmH2O, n=13), 3) PEEP 5 (PEEP of 5 cmH2O, n=12), and 4) PEEP 10 (PEEP of 10 cmH2O, n=13). Positive end expiratory pressure groups were tracheostomized and mechanically ventilated with a tidal volume of 10 mL/kg, respiratory rate of 70 rpm, and inspired oxygen fraction of 1. Animals were maintained under isoflurane anesthesia. After two hours, laparotomy was performed, and leukocyte-endothelial interactions were evaluated by intravital microscopy.
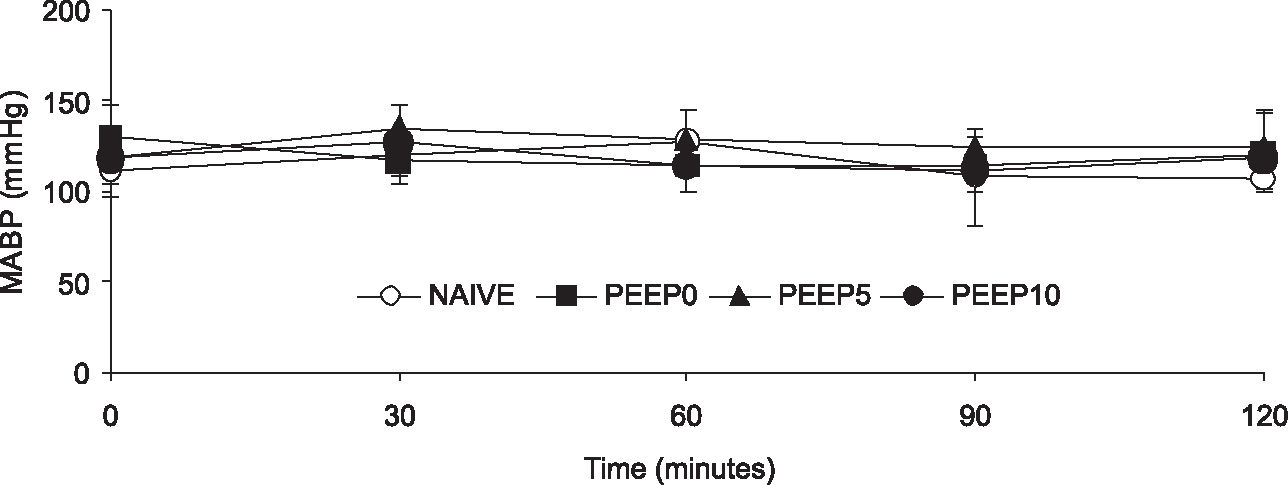
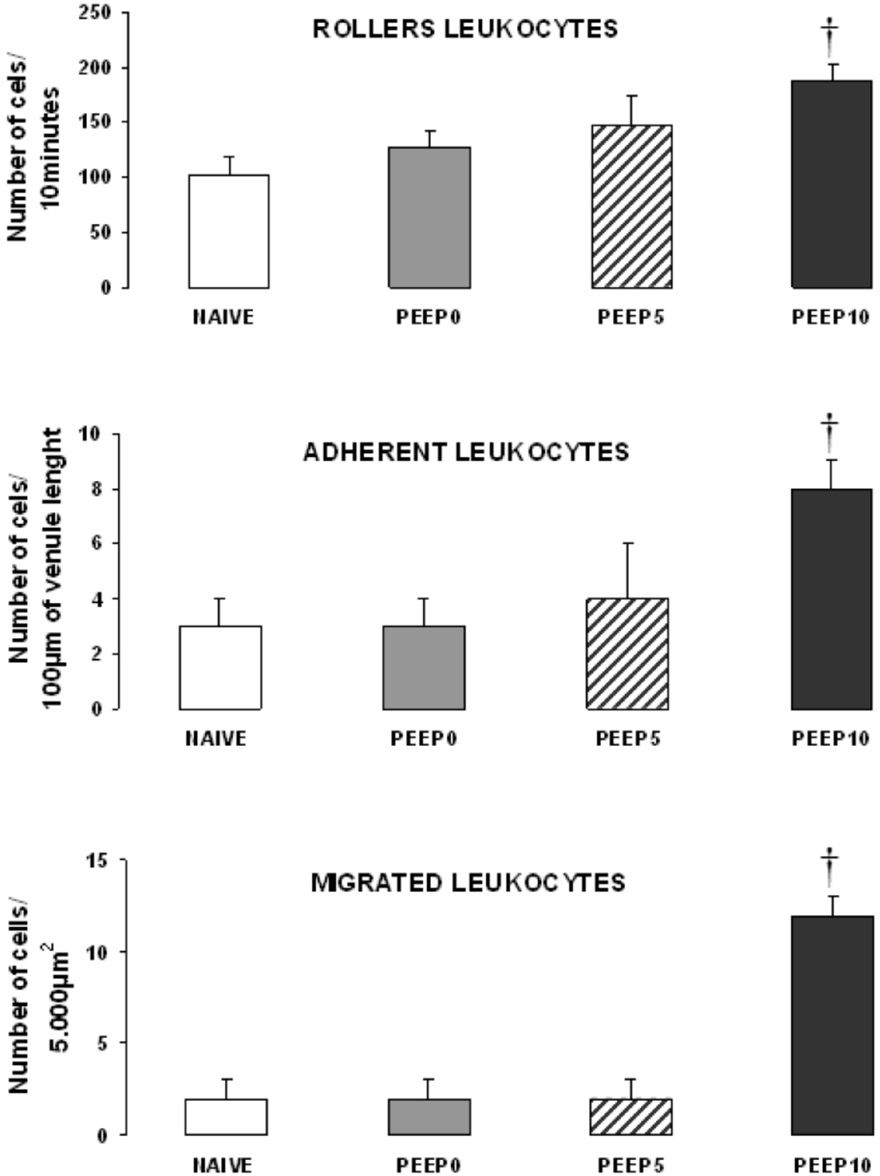
RESULTS:No significant changes were observed in mean arterial blood pressure among groups during the study. Tracheal peak pressure was smaller in PEEP 5 compared with PEEP 0 and PEEP 10 groups (11, 15, and 16 cmH2O, respectively; p<0.05). After two hours of MV, there were no differences among NAIVE, PEEP 0 and PEEP 5 groups in the number of rollers (118±9,127±14 and 147±26 cells/10minutes, respectively), adherent leukocytes (3±1,3±1 and 4±2 cells/100μm venule length, respectively), and migrated leukocytes (2±1,2±1 and 2±1 cells/5,000μm2, respectively) at the mesentery. However, the PEEP 10 group exhibited an increase in the number of rolling, adherent and migrated leukocytes (188±15 cells / 10 min, 8±1 cells / 100 μm and 12±1 cells / 5,000 μm2, respectively; p<0.05).
CONCLUSIONS:High intrathoracic pressure was harmful to mesenteric microcirculation in the experimental model of rats with normal lungs and stable systemic blood pressure, a finding that may have relevance for complications related to mechanical ventilation.
Mechanical ventilation (MV) and positive end expiratory pressure (PEEP) have been widely used to improve oxygenation and treat acute respiratory failure. However, the increased intrathoracic pressure can affect nearly every system of the body due to homeostatic interactions involving the lungs and other organs.1 These complex, dynamic interactions may contribute to several complications. Distribution of stress during cyclic tidal ventilation has been associated with macrophage, neutrophil and endothelial cell activation,2,3 inflammatory mediator release,4 vascular permeability alterations,5 increased adhesion molecule expression,6 and leukocyte sequestration3 in the lungs. It is also associated with a number of morbid conditions such as for instance diabetes mellitus.7
Characteristics of the splanchnic vasculature8 make the gastrointestinal tract vulnerable to adverse effects related to MV and PEEP, with a particularly pronounced risk of organ dysfunction.9–13 Hypoperfusion appears to play a pivotal role in the pathogenesis of gastrointestinal complications in mechanically ventilated patients, the most prevalent of which are mucosal damage, hypomotility, diarrhea, mesenteric ischemia, gastrointestinal failure and sepsis.11,12 Increased intrathoracic pressure also induces diaphragmatic descent, which may play a role in increased intra-abdominal pressure during critical illness, leading to splanchnic ischemia and organ dysfunction.14–16
Several studies have focused on changes that occur at the microcirculatory level, showing that disturbances in the microcirculation may be markers of disease severity and potential predictors of the outcome of critically ill patients.17–19 In the experimental setting, intravital microscopy is a unique technique to directly observe the in vivo leukocyte-endothelial interactions. This approach has been used to investigate the mesenteric microcirculation in models of hemorrhagic shock, reperfusion and sepsis.20–22 Recently, there has been a growing interest in the effects of MV and PEEP on microcirculation. Lim and Wagner23 showed that the combination of MV and PEEP of 8 cmH2O causes a significant increase in neutrophil adhesion and leukocyte recruitment in the trachea in rats. However, little is known regarding the effects of MV and PEEP on mesenteric microcirculation. The aim of the current experimental study was to investigate the effects of different PEEP levels on leukocyte-endothelial interactions at the mesentery.
MATERIALS AND METHODSThe protocol was approved by the Institutional Animal Care and Use Committee of the Heart Institute (InCor), Faculdade de Medicina da Universidade de São Paulo. The experiments were performed according to National Institutes of Health Guidelines for the use of experimental animals.
Forty-four adult male Wistar rats (200–300 g, University of Sao Paulo Medical School Laboratory Animals, Sao Paulo, Brazil) were housed in our facility for three to five days before the experiment. They were given unrestricted access to food and water. On the day of the experiment, the animals were anesthetized with pentobarbital sodium (50 mg/kg, I.P.). The right carotid artery was cannulated with a PE50 tube, and systemic arterial blood pressure was recorded on a polygraph (Polygraph MK-III-S Model, Narco Bio-Systems, TX, USA). Thereafter, animals were randomly assigned to the following experimental groups: 1) NAIVE: only anesthesia, 2) PEEP0: MV with PEEP=0 cmH2O, 3) PEEP5: MV with PEEP=5 cmH2O or 4) PEEP10: MV with PEEP=10 cmH2O.
Tracheostomy and Mechanical Ventilation. Animals were tracheostomized with polyethylene catheter PE45 tubes, and they were mechanically ventilated with a tidal volume of 10 mL/kg (Harvard Ventilator, 683 Model, Harvard Rodent Apparatus, South Natick, USA) at a respiratory rate of 70 rpm and with an inspired oxygen fraction of one. Anesthesia was maintained with inhaled isoflurane (4%) during two hours of MV.
Tracheal Peak Pressure, Blood Gas Analysis and Hematocrit. Tracheal peak pressure measurements were performed at 0 (baseline), 30, 60, 90 and 120 minutes, with a 142PC05D differential pressure transducer (Honeywell, Freeport, IL, USA) connected to a side tap in the tracheal cannula.24 Blood samples were collected from the right carotid artery for blood gas analysis and hematocrit determination. Arterial blood gases were tested by a gas analyzer (Radiometer ABL 555, Radiometer Medical, Kopenhagen, Denmark) at baseline (before MV) and after two hours of MV in all animals. Hematocrit was measured by microcapillary tube centrifugation only at baseline.
Intravital Microscopy at the Mesentery. We performed mesenteric surgical preparation as previously described.20,21 In brief, after two hours of MV, we performed a laparotomy with a midline abdominal incision, and we exposed the distal ileum and its accompanying mesentery for in vivo microscopic examination of the mesenteric microcirculation. The animals were placed in the right lateral decubitus position on a specially designed, warmed (37°C) stage with a transparent platform, on which the tissue to be transilluminated was placed. The tissue was kept moist with regular applications of warm (37°C) Krebs solution and covered with an impermeable membrane (Saran Wrap, Dow Chemical Co, UK) to prevent dehydration. Care was taken during handling to prevent physical damage. Mesenteric microcirculation was assessed after ten minutes of stabilization. We performed intravital microscopy in three to five microvessels after two hours of MV in each animal. Post-capillary venules with diameters ranging from 12 to 20 μm were randomly selected. A CCD color camera (TK-C1380U, JVC Co, Tokyo, Japan) was incorporated into a triocular microscope (Axioplan 2, Carl Zeiss Co, München-Hallbergmoos, Germany) to facilitate observation of the enlarged image (1960x) on a computer monitor (SyncMaster 753DFX, Samsung, Manaus, Brazil). Analyses of leukocyte-endothelial interactions were performed online, by using digital image software (KS300, Carl Zeiss Co, München-Hallbergmoos, Germany). In addition, images were stored, enabling off-line time-delayed analysis.
Rolling Leukocytes. Rolling leukocytes were defined as white blood cells that moved at a velocity significantly slower than that of erythrocytes in a given microvessel.25 The number of rolling leukocytes was expressed in terms of the mean number of cells passing a designated line perpendicular to the venular axis every ten minutes. A given section of the vascular bed was tested only once. Three to five microvessels were tested in a single animal. Results are presented as the number of rolling leukocytes/ten minutes.
Adherent Leukocytes. A leukocyte was considered to be adherent to the venular endothelium if it remained stationary for >30 seconds.26 Adherent cells were counted during a ten-minute period in a 100 μm segment of the vessel. Three to five microvessels were selected from a single animal, and a given section of the vascular bed was tested only once. Results are presented as the number of adherent leukocytes / 100 μm venule length.
Migrated Leukocytes. The number of leukocytes accumulating at the connective tissue, adjacent to the chosen post-capillary venule, was determined over a standard area of 5,000 μm.2,20,21 Three to five different fields were evaluated for each microvessel. Three to five microvessels were selected in a single animal. Results are expressed in terms of the number of migrated leukocytes/5,000 μm2.
Lung Histomorphometric Analysis. Animals were anesthetized (pentobarbital sodium, 50 mg/kg I.P.) and exsanguinated by cutting the abdominal aorta. Lungs were gently inflated (10 mL/kg), removed and fixed with 10% formaldehyde solution in sodium phosphate buffer 0.2 mol/L (pH 7.2) for 24 hours, before being dehydrated in ethanol and embedded in paraffin. Three sections (5 μm) cut from the apex to the base of the right and left lungs were stained with hematoxylin-eosin (HE). Histological examinations were performed by two assistants. Briefly, by using a 100-point grid with a known area (104 μm2 at 1000x) attached to the ocular lens of the microscope, 12–20 fields in each section (three to five sections per animal) were randomly chosen, and 1) edema volume index (volume fraction of edema/total perivascular tissue) and 2) polymorphonuclear cell density (cells / 104 μm2) were quantified within the perivascular tissue, while 3) polymorphonuclear cell density (cells / 104 μm2) was quantified within the alveolar area. The edema volume index was assessed using the number of points in the grid colocalized with edematous tissue divided by the total number of points colocalized with the perivascular space (volume fraction). Polymorphonuclear cells were counted within either alveolar or perivascular areas. Tissue area in each field was calculated according to the number of points associated with alveolar or perivascular tissue, as a proportion of the total grid area. The density of inflammatory cells was determined from the number of positive cells in each field divided by the tissue area (cells / 104 μm2).
Statistical Analysis. Data are presented as means ± standard deviations (SD). Statistical intergroup comparisons of leukocyte-endothelial interactions, lung histomorphometry, and hematocrit were performed using one-way ANOVA. Statistical comparisons of mean arterial blood pressure, tracheal pressure, and blood gas analyses among groups were performed using two-way ANOVA. Differences among groups were tested by the Tukey multiple comparisons test. A P value less than 0.05 was considered significant.
RESULTSBody weight, hematocrit, mean arterial blood pressure, respiratory parameters, and blood gas analysis. Animals presented similar values of hematocrit (46±1). There were no differences in mean arterial blood pressures across groups during the two-hour study period (Figure 1). Values of arterial blood gas were similar across groups at baseline: pH (7.35), PaO2 (88 ± 15 mmHg), and PaCO2 (44 ± 6 mmHg). However, as expected, after two hours of MV, animals presented increased PaO2 (>300 mmHg, p<0.05) and decreased PaCO2 (38 ± 2 mmHg, p<0.05), with no changes in pH (7.40). Tracheal peak pressure was smaller in the PEEP5 group compared with the PEEP0 and PEEP10 groups (Table 1, p<0.05).
Mean values and standard deviations of tracheal peak pressure at the baseline, and after one and two hours of mechanical ventilation (*, p<0.05 vs. baseline; †, p<0.05 vs. other groups at the same time points)
| Groups | Baseline | 1-hour MV | 2-hours MV |
|---|---|---|---|
| PEEP0 | 9 ± 1 | 15 ± 3* | 16 ± 2* |
| PEEP5 | 9 ± 0 | 11 ± 1† | 12 ± 1† |
| PEEP10 | 10 ± 1 | 16 ± 1* | 16 ± 1* |
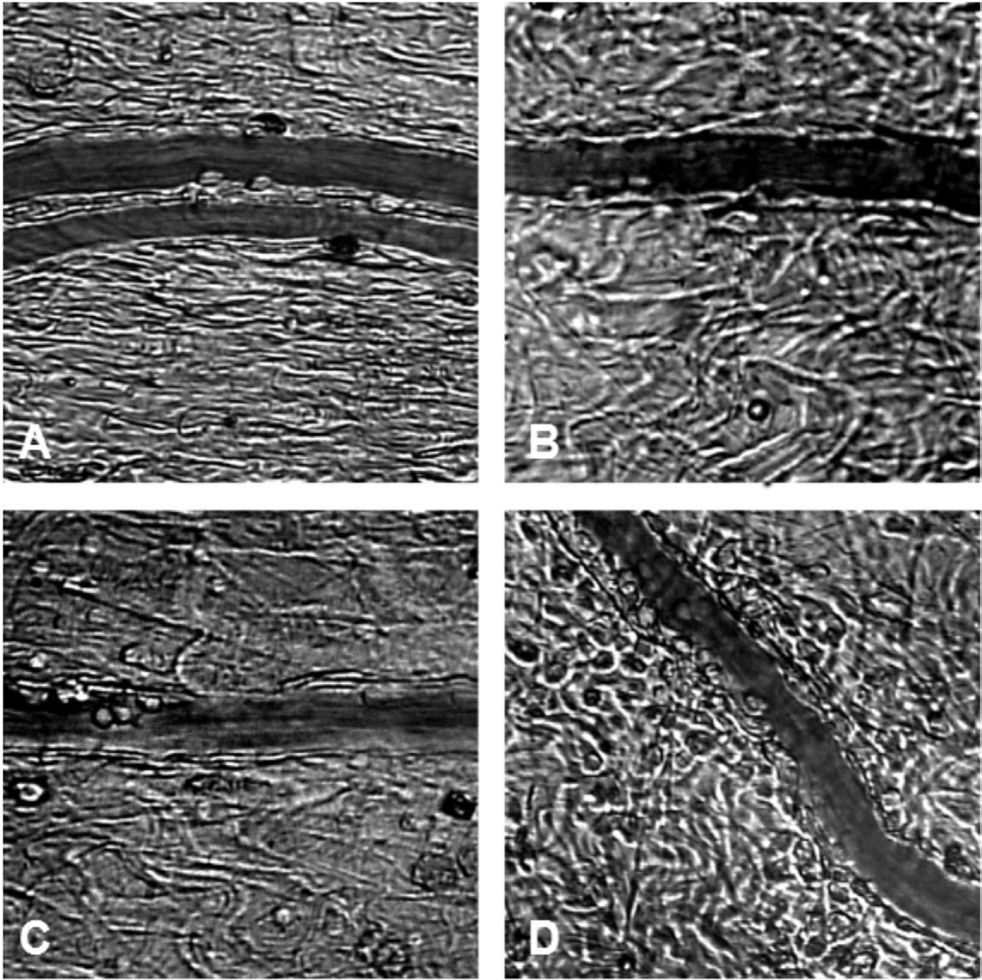
Mesenteric Leukocyte-Endothelial Interactions. Microvessel (Figure 2) diameter was similar in NAIVE, PEEP0, PEEP5 and PEEP10 groups (13.7±2.8, 11.8 ± 3.0, 13.8 ± 1.6, and 13.8 ± 2.6 μm, respectively; p>0.05). Few adherent and migrated leukocytes were noted within the mesentery microcirculation in animals breathing ambient air (Figure 3). There were no differences among NAIVE, PEEP0 and PEEP5 groups in the number of rolling, adherent and migrated leukocytes. However, the PEEP10 group presented an increased number of rolling, adherent and migrated leukocytes compared to the other groups (p<0.01).
Rolling (number of cells/10 minutes), adherent (number of cells/100 μm venule length) and migrated leukocytes (number of cells/5,000 μm2) in post-capillary venules at the mesentery (mean values ± SD) in NAIVE (n=3), PEEP0 (n=6), PEEP5 (n=6) and PEEP10 (n=7) groups. †, p<0.01 PEEP10 vs. other groups
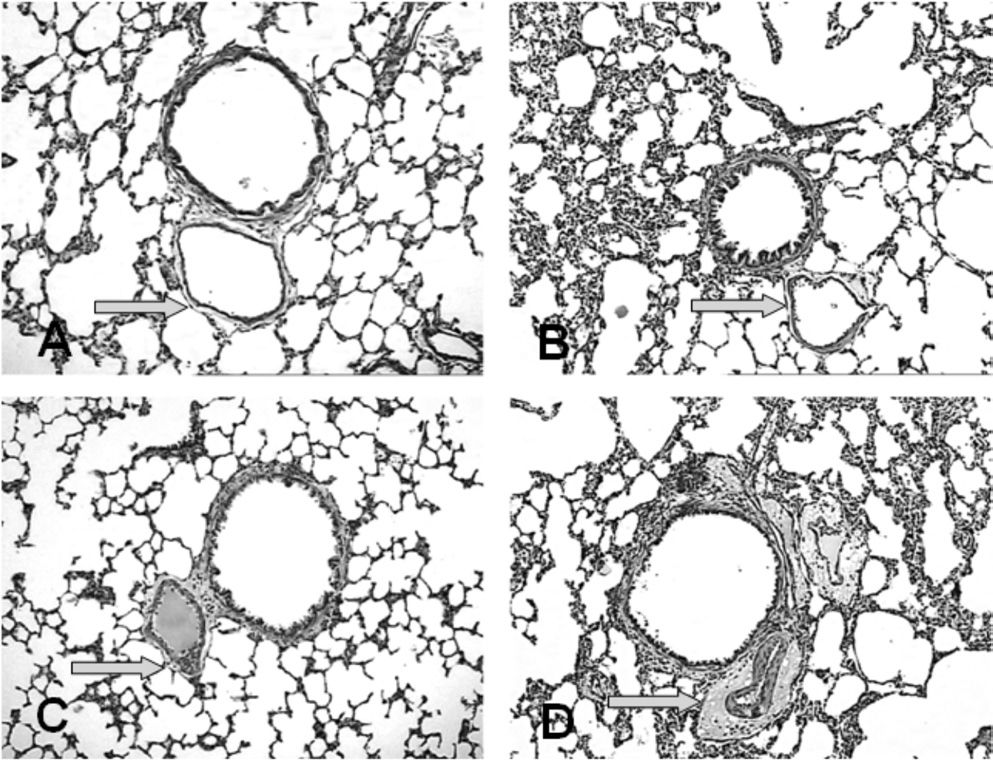
Lung Neutrophil Infiltration and Edema by Histomorphometry. Lung tissue analysis revealed no intra-alveolar hemorrhage or hyaline membranes in all groups (Figure 4). However, PEEP groups presented increased polymorphonuclear cell density in the parenchyma and in the perivascular tissue compared with the NAIVE group (p<0.05, Table 2). In addition, a larger volume of perivascular edema was found in all mechanically ventilated animals compared with the NAIVE group (p<0.05).
Mean values and standard deviations of neutrophil infiltration and fluid accumulation within pulmonary microvessels and parenchyma after two hours of mechanical ventilation (*, p<0.05 vs. NAIVE; †, vs. others groups)
| Groups | n | Lung Parenchyma | Lung Perivascular Tissue | |
|---|---|---|---|---|
| Neutrophils/104 μm2 | Edema Index | Neutrophils/104 μm2 | ||
| NAIVE | 3 | 1.22 ± 1.19 | 0.03 ± 0.02 | 0.72 ± 0.05 |
| PEEP0 | 4 | 9.67 ± 3.78* | 0.24 ± 0.03* | 1.90 ± 0.75* |
| PEEP5 | 3 | 11.49 ± 3.36* | 0.23 ± 0.04* | 0.72 ± 0. 47 |
| PEEP10 | 3 | 9.47 ± 1.95* | 0.54 ± 0.04*† | 1.28 ± 0.17* |
The model described in the current in vivo study proved to be suitable for assessing initial injury to the mesenteric microcirculation during MV and PEEP. The use of PEEP parameters of 0 and 5 cmH2O did not cause sufficient changes in leukocyte-endothelial interactions in the mesentery. However, a PEEP of 10 cmH2O caused significant microcirculatory changes in the mesentery, which was evidenced by increased leukocyte rolling and adhesion in the microvasculature, as well as migration to the perivascular tissue. All mechanically ventilated animals presented leukocyte and fluid accumulation within both the pulmonary microvessels and the parenchyma.
Leukocyte-endothelial interactions are mediated by a variety of glycoproteins expressed on the surface of leukocytes and endothelial cells. The accumulation of leukocytes in inflamed tissues was found to be preceded by leukocyte rolling and adhesion to the vascular endothelium.27,28 Leukocytes roll along the walls of post-capillary venules, as mediated by the selectin family of adhesion molecules.27 Leukocytes become firmly adherent to the vascular wall on account of the interaction between ICAM-1 on endothelial cells with 2 integrins on leukocytes.21 After activation, neutrophils generate and release toxic oxygen metabolites, numerous proteases, and phospholipase products, all of which may result in vasomotor changes, endothelial injury, and loss of vascular integrity.29
In rats with intact lungs, Lim and Wagner23 have studied the effects of PEEP on tracheal microcirculation, showing deleterious effects of the airway distension cause by the use of PEEP. In their study, MV was performed with a tidal volume of 6 mL/kg and a respiratory rate of 80 rpm. Furthermore, by using PEEP of 8 cmH2O, the authors reported a 30-minute transitory decrease in mean arterial blood pressure, associated with decreased rolling leukocyte velocity and an increased number of rolling and adherent leukocytes in the tracheal vasculature. They concluded that PEEP of 8 cmH2O is a critical level for tracheal microcirculation.
Our experimental study focused on mesenteric leukocyte-endothelial interactions because the gastrointestinal tract may be under increased risk of organ dysfunction11,22 during MV and PEEP. In critically ill patients, gastrointestinal dysfunction has been associated with increased morbidity and mortality.11,12 We demonstrated that the combination of a moderate tidal volume (10 mL/kg) and high PEEP (10 cmH2O) affected mesenteric vascular endothelium, which resulted in increased leukocyte-endothelial interactions. We speculate that these events may have been induced by gastrointestinal compression, which may have resulted in splanchnic hypoperfusion and an imbalance between oxygen supply and demand.14–16,30–34 Sequential events of hypoperfusion followed by reperfusion triggered by ventilatory strategies may be associated with acute nonocclusive mesenteric ischemia in the critical care setting.35
We also observed leukocyte and fluid accumulation within pulmonary microvessels and parenchyma in all mechanically ventilated animals. Eosinophils were absent. We speculate that the histologic lung alterations observed in all mechanically ventilated rats may be a consequence of tracheal intubation, exposure to hyperoxia, and alveolar overdistension during mechanical tidal cycling, all of which may be associated with vascular damage and increased polymorphonuclear cell accumulation in lungs.2–6,36,37
This study has limitations. Animals submitted to MV and PEEP were ventilated with a 100% inspired oxygen fraction, although subsequent hyperoxia may have influenced lung results. However, this protocol was used to avoid any possibility of hypoxia. In fact, hypoxia has been associated with rapid increases in vascular permeability and in leukocyte adherence and migration into the extravascular space of the mesenteric microcirculation in rats.38 Secondly, one may argue that in clinical practice, high PEEP levels have been widely used only in patients with acute lung injury, in which the cardiovascular effects of increased intrathoracic pressure are potentially reduced.39 However, patients with normal lungs may require MV during deep sedation or anesthesia in the surgical, emergency, and intensive care units. Ventilatory strategies using a moderate tidal volume of 10 mL/kg and PEEP levels from zero up to 10 cmH2O have been used with surgical patients.9,40 Thirdly, PEEP in the setting of relatively normal lungs and without fluid administration is very likely to reduce cardiac output - we did not measure cardiac output or mesenteric blood flow. However, fluid administration or inotropic agents may have affected microcirculation. Besides, we identified significant alterations in mesenteric leukocyte-endothelial interactions despite the unchanged mean arterial blood pressure among groups. Finally, although we did not demonstrate the mechanism involved in this inflammatory response at the mesentery that caused increased intrathoracic pressure, it is reasonable to hypothesize that the combination of a number of mechanical forces, such as alveoli overdistention, lung stretch, and compressive stress on the gastrointestinal organs may have resulted in mesenteric hypoperfusion and inflammation.
In conclusion, the current animal study shows that the association of moderate tidal volume and high PEEP may be harmful to mesenteric microcirculation in the setting of normal lungs and stable systemic blood pressure. This finding may have relevance in understanding the development of complications related to MV.
The authors would like to thank Dr. Carmem Valente Barbas, Dr. Daniel de Backer and Dr. Luciano Gattinoni for outstanding discussion in the poster session of International Symposium on Intensive Care and Emergency Medicine for Latin America, and Julia Fukushima for cooperation in the statistical analysis. Photomicrographs were taken by the Museum of Pathology, Faculdade de Medicina da Universidade de São Paulo. The platform for intravital microscopic study of the rat mesentery was developed by Dr. Naomi Kondo Nakagawa, Simão Bacht, and Dr. Idágene Cestari, and built by the Bioengeering Division of the Heart Institute (InCor), Faculdade de Medicina da Universidade de São Paulo. This work was supported by grant of PRONEX and FAPESP (proc. 07/51605-9).