The aim of this study was to (1) observe the extent to which hemodynamic and glucose measurements change in patients submitted to a dental procedure with and without a local anesthetic and a vasoconstrictor (LAVA; 2% mepivacaine with adrenaline 1∶100,000) and (2) correlate those parameters with the patients' anxiety levels.
METHOD:This was an unblinded, random, prospective, and observational study with paired groups. Patients were evaluated during two different consultations during which they either did or did not receive a local anesthetic/vasoconstrictor.
RESULTS:Thirty-seven patients ranging in age from 18 to 45 years (mean 30.4 ± 5.5 years) were evaluated. Hemodynamic parameters, including systolic blood pressure, diastolic blood pressure, heart rate, and glucose levels, did not change significantly in healthy patients, regardless of whether a LAVA was administered during the dental treatment.
CONCLUSION:The patients' anxiety statuses neither varied significantly nor showed any correlation with the studied hemodynamic parameters and glucose levels, regardless of whether local anesthetics were used.
Under most circumstances, it is impossible to provide effective dental care without the use of local anesthetics and vasoconstrictors (LAVA). Although these drug classes have a history of safety and efficacy, they have the potential to produce significant toxicity if used carelessly. Whereas local anesthetics produce peripheral vasodilatation, which contributes to hypotension, even small doses of vasoconstrictors can influence cardiovascular function, causing an increase in cardiac output and stroke volume as well as alterations in heart rate and arterial blood pressure.1-4
Anxiety may be defined as either a cognitive, emotional, and physical reaction to a dangerous situation or the anticipation of a threat.3 Pain and anxiety triggered by dental treatment can induce the secretion of endogenous catecholamines. When the situation is combined with LAVA use, it may increase its undesirable effects on the cardiovascular system.2,5-7 The physiological effects of such catecholamines can also include the stimulation of glycogenolysis with a consequent increase in the blood level of glucose;8 however, this issue is controversial.9,10
In clinical practice, dentists try to find the most comfortable and safe situations for patients. They often have to decide between using local anesthetics or proceeding with a simple procedure without them. In the latter circumstance, they must decide which is better for the patient physiologically and psychologically. The aim of this study was to (1) observe the extent to which hemodynamic and glucose measures change in patients submitted to a dental procedure with and without LAVA administration (2% mepivacaine with adrenaline 1∶100,000) and (2) correlate those parameters with patients' anxiety levels. Gaining an understanding of these changes may also allow dentists to identify situations of increased risk and prevent emergency situations in clinical practice.
PATIENTS AND METHODSThis is an unblinded prospective and observational study with paired groups. It was submitted and approved by the UNOESC/HUST Ethical Committee for Human Research (number 087/2007). All patients were randomly selected and invited to participate; however, this study was limited to healthy patients between the ages of 18 and 45 years with the ability to maintain eight hours of fasting. Data collection was performed in the first hours of the morning. The patients were evaluated during two different appointments for dental treatment with a time interval of at least 48 hours. For the first consultation, the patients (control group) did not receive any LAVA, whereas the patients (test group) in the second consultation received a LAVA (2% mepivacaine with adrenaline 1∶100,000; Cloridrato de Mepivacaína 2% com Epinefrina 1∶100,000, Mepiadre®, DFL, Brazil) for dental treatment at the maximum amount of 3.2 mL (two cartridges).
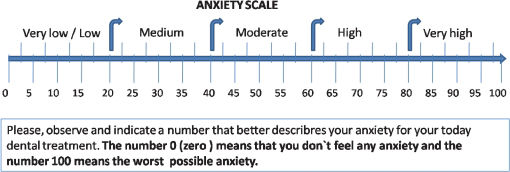
On both occasions and before the dental procedure, patients were asked about the fasting and then rested for 15 minutes. During this period, patients were asked to rate how anxious they felt about the upcoming procedure using a numerical scale ranging from 0 to 100 (see Fig. 1). Immediately before starting the planned dental procedures for both consultations, baseline measurements of glucose (GLU), systolic and diastolic arterial blood pressure (SyBP and DiBP), and heart rate (HR) were taken. A calibrated wrist digital sphygmomanometer (Powerpack®, MS-808, Powerpack) certified by INMETRO (National Institute of Metrology, Standardization and Industrial Quality, Brazil) was used. A glucometer was utilized for GLU measurements (mg/dL; OneTouch® Ultra®, Johnson & Johnson, Milpitas, California, USA). Fifteen minutes after the initiation of the procedure, new measurements of SyBP, DiBP, HR and GLU were performed. For the second consultation, the additional measurement was taken 15 minutes after the anesthesia procedure with LAVA. With the exception of GLU, a final measurement of the variables was conducted at the end of the day's procedure. Following the procedure, a snack and fruit juice were offered to the patients to compensate for the fasting period. The data were analyzed by BioEstat (version 5.0; Belém/Pará, Brazil), with the level of significance set at p<0.05.
RESULTSThirty-seven patients ranging in age from 18 to 45 years (mean 30.4 ± 5.5 years) were evaluated. Nineteen (51.4%) patients were male. For the first appointment without the LAVA, the following procedures were performed: dental restoration (27%), prosthesis (21.6%), dental prophylaxis (18.9%), endodontic treatment (16.2%), periodontal treatment (10.8%), and others (5.4%). For the second appointment with the use of LAVA, the following procedures were performed: dental restoration (67.6%), prosthesis (10.8%), periodontal treatment (8.1%), endodontic treatment (5.4%), and others (8.1%).
Patients' self-reported anxiety levels related to dental treatment ranged from 5 to 90 (mean 28.9 ±19.8) during the first appointment (control) and from 0 to 95 (mean 25.6 ±18.8) during the second (test). For the first and second appointments, patient anxiety level was not significantly correlation with GLU level, SyBP, DiBP, and HR in the established periods of data collection. In addition, self-reported anxiety level did not vary significantly between male and female patients or by age, which was dichotomized as less than and greater than 30 years (median) of age.
No significant changes were observed between appointments (control and test groups) for all measurements of GLU levels (see Table 1) and hemodynamic changes, including SyBP (see Table 2), DiBP (see Table 3), and HR (see Table 4).
Mean, standard deviation (SD), and results of statistical analyses of four glucose measurements taken during two different appointments for dental treatment with and without LAVA (2% mepivacaine with adrenaline 1∶100,000) (n = 37).
| Glucose measurements (mg/dL) | Mean | SD | Paired t-Test within appointments∗ | ANOVA∗ between all measurements | |
|---|---|---|---|---|---|
| First appointment (Dental procedure without anesthesia) | Baseline | 90.3 | 11.8 | p = .73 | p = .36 |
| Dental procedure with no anesthesia | 90.8 | 12.9 | |||
| Second appointment (Dental procedure with anesthesia) | Baseline | 92.9 | 10.4 | p = .21 | |
| Dental procedure with local anesthesia | 94.7 | 12.1 |
Mean, standard deviation (SD), and results of statistical analyses of six systolic arterial blood pressure measurements taken during two different appointments for dental treatment with and without LAVA (2% mepivacaine with adrenaline 1∶100,000) (n = 37).
| Systolic arterial blood pressure measurements | Mean | SD | ANOVA∗ within appointment | ANOVA∗ between all measurements | |
|---|---|---|---|---|---|
| First appointment (Dental procedure without anesthesia) | Baseline | 128.1 | 15.6 | ||
| During the procedure (15 minutes) | 124.3 | 14.1 | p = .54 | ||
| At the end of the procedure | 127.7 | 12.6 | p = .83 | ||
| Second appointment (Dental procedure with anesthesia) | Baseline | 126.1 | 15.8 | ||
| During the procedure (15 minutes after local anesthesia) | 125.3 | 11.8 | p = .86 | ||
| At the end of the procedure | 127.0 | 11.1 |
Mean, standard deviation (SD), and results of statistical analyses of six diastolic arterial blood pressure measurements taken during two different appointments for dental treatment with and without LAVA (2% mepivacaine with adrenaline 1∶100,000) (n = 37).
| Diastolic arterial blood pressure measurements | Mean | SD | ANOVA∗ within appointment | ANOVA∗ between all measurements | |
|---|---|---|---|---|---|
| First appointment (Dental procedure without anesthesia) | Baseline | 85.7 | 11.4 | ||
| During the procedure (15 minutes) | 80.2 | 13.5 | p = .10 | ||
| At the end of the procedure | 85.0 | 11.0 | p = .17 | ||
| Second appointment (Dental procedure with anesthesia) | Baseline | 82.2 | 11.3 | ||
| During the procedure (15 minutes after local anesthesia) | 79.8 | 12.0 | p = .62 | ||
| At the end of the procedure | 82.0 | 10.9 |
Mean, standard deviation (SD), and results of statistical analyses of six heart rate measurements taken during two different appointments for dental treatment with and without LAVA (2% mepivacaine with adrenaline 1∶100,000) (n = 37).
| Heart rate measurements | Mean | SD | ANOVA within appointment | ANOVA between all measurements | |
|---|---|---|---|---|---|
| First appointment (Dental procedure without anesthesia) | Baseline | 71,5 | 11.7 | ||
| During the procedure (15 minutes) | 69.8 | 11.3 | p = .80 | ||
| At the end of the procedure | 71.0 | 10.4 | p = .97 | ||
| Second appointment (Dental procedure with anesthesia) | Baseline | 71.7 | 12.0 | ||
| During the procedure (15 minutes after local anesthesia) | 70.5 | 12.6 | p = .77 | ||
| At the end of the procedure | 69.8 | 10.9 |
Most types of dental treatment can produce discomfort and pain at some level. Further, pain may influence or be influenced by anxiety levels related to dental treatment. The use of a LAVA (injection) can also produce extreme pain and fear, at least momentarily, in some patients.11,12 On the other hand, when a dentist judges that it is possible to go on with a procedure without the use of a LAVA, patients may also exhibit discomfort, anxiety, and pain. An ineffective form of pain control increases the risk of negative patient health outcomes due to increased levels of endogenous catecholamines, particularly norepinephrine, which may increase blood pressure and heart rate.2,6 The purpose of this study was to determine if there was a significant correlation between anxiety levels, hemodynamics, and glucose parameters in patients undergoing dental treatment, regardless of whether or not they received a LAVA. No such relationship was found.
Because patients experience adrenergic stimulation under both sets of circumstances (with and without a LAVA), it is unclear why their hemodynamic and glucose parameters did not change significantly. With regard to adrenaline (also called epinephrine) and adrenergic system stimulation, it might be that adrenaline has both beta 1 and beta 2 activity. Beta 1 stimulation tends to cause an increase in blood pressure, whereas beta 2 stimulation tends to decrease blood pressure; therefore, it often does not dynamically increase blood pressure due, in part, to beta 2 activity. A second possible explanation is that the hemodynamic alterations are usually short in plasma due to the short adrenaline half-life, which is approximately less than three minutes. In addition, when stimulated, the sympathetic nervous system primarily releases norepinephrine and secondarily releases epinephrine. The effects of both substances on blood pressure have been described as limited.2,13
Alemany-Martínez et al.14 monitored healthy patients during the surgical removal of lower third molars using 4% articaine with a vasoconstrictor (adrenaline 1∶100,000). They found that the hemodynamic measurements remained within normal parameters. In that study, all patients received less than 5.4 mL (3 cartridges) of the LAVA and, with the exception of the differences between the methods, these results are consistent with those of the present study, which also showed no modifications between baseline and procedure measurements of SyBP, DiBP, and HR. Further, there was no correlation found between hemodynamic parameters and anxiety in both studies.
Elad et al.5 examined the hemodynamic and electrocardiographic responses of cardiovascular patients to two different local anesthetic solutions with different vasoconstrictor concentrations (adrenaline 1∶200,000 versus adrenaline 1∶100,000) and found no differences between the hemodynamic indices of SyBP, DiBP, HR, and blood oxygen saturation at various time points and intervals between the two groups. Conrado et al.15 evaluated 54 patients with coronary disease who underwent dental extraction under local anesthesia either with or without a vasoconstrictor. They concluded that the use of anesthesia with 1∶100,000 epinephrine does not result in additional ischemic risks. Nevertheless, significant variations in arterial blood pressure and heart rate were observed in that study in both groups (with and without a vasoconstrictor). Liau et al.6 found that patients with severe anxiety and pain upon injection had a significant increase in HR during anesthetic administration; however, that increase lasted only 10 minutes. Similar to the results of the present study, Liau et al.6 did not report any statistical differences in SyBP and DiBP with one cartridge of 2% lidocaine with 1∶100,000 epinephrine.
Variations in glucose plasma levels during dental treatment have been the subject of study and controversy in the literature.9,10,16-18 Tily and Thomas 9 compared the effect of epinephrine (adrenaline) administration in the dental local anesthetic solution on blood glucose concentrations in healthy and diabetic dental patients after extraction. They observed no significant differences in pre- and post-operative blood glucose levels. Nakamura et al.10 investigated the changes in blood pressure, plasma catecholamines, glucose, and insulin concentrations in 11 normotensive patients during dental surgery and found that the administration of both local anesthetics and tooth extraction activates sympathoadrenal outflow, resulting in increases of the SyBP, HR, plasma epinephrine, and serum glucose concentrations. They concluded that the adrenaline concentration increased and reached its peak just after the administration of local anesthetics, yet the peak of epinephrine occurred within a time period similar to that of the increase of the serum glucose level, suggesting that there is a close relationship between the two variables. The increase in the glucose level may be small and transient for healthy patients due to compensatory and regulatory mechanisms of the body. Although an increase in the mean glucose levels was observed in this study, it did not reach statistical or even clinical significance.
CONCLUSIONHemodynamic parameters, including SyBP, DiBP, HR, and glucose levels, did not change significantly, regardless of whether 2% mepivacaine with adrenaline 1∶100,000 (two cartridges) was used in healthy patients undergoing dental treatment. The anxiety level of patients neither varied significantly nor showed any correlation with the investigated hemodynamic parameters and glucose levels, regardless of whether local anesthetics were used.