To evaluate the concordance between the Gleason scores of prostate biopsies and radical prostatectomy specimens, thereby highlighting the importance of the prostate-specific antigen (PSA) level as a predictive factor of concordance.
METHODSWe retrospectively analyzed 253 radical prostatectomy cases performed between 2006 and 2011. The patients were divided into 4 groups for the data analysis and dichotomized according to the preoperative PSA, <10 ng/mL and ≥10 ng/mL. A p-score <0.05 was considered significant.
RESULTSThe average patient age was 63.3±7.8 years. The median PSA level was 9.3±4.9 ng/mL. The overall concordance between the Gleason scores was 52%. Patients presented preoperative PSA levels <10 ng/mL in 153 of 235 cases (65%) and ≥10 ng/mL in 82 of 235 cases (35%). The Gleason scores were identical in 86 of 153 cases (56%) in the <10 ng/mL group and 36 of 82 (44%) cases in the ≥10 ng/mL group (p = 0.017). The biopsy underestimated the Gleason score in 45 (30%) patients in the <10 ng/mL group and 38 (46%) patients in the ≥10 ng/mL (p = 0.243). Specifically, the patients with Gleason 3 + 3 scores according to the biopsies demonstrated global concordance in 56 of 110 cases (51%). In this group, the patients with preoperative PSA levels <10 ng/dL had higher concordance than those with preoperative PSA levels ≥10 ng/dL (61% x 23%, p = 0.023), which resulted in 77% upgrading after surgery in those patients with PSA levels ≥10 ng/dl.
CONCLUSIONThe Gleason scores of needle prostate biopsies and those of the surgical specimens were concordant in approximately half of the global sample. The preoperative PSA level was a strong predictor of discrepancy and might improve the identification of those patients who tended to be upgraded after surgery, particularly in patients with Gleason scores of 3 + 3 in the prostate biopsy and preoperative PSA levels ≥10 ng/mL.
Despite the variability in incidence, prostate cancer (PC) remains one of the most prevalent cancers worldwide, and in many countries, it is the leading cause of cancer death among men. In 2012, the estimate of PC deaths in the European Union was 69,960, corresponding to 10.74 deaths per 100,000 men (1). In the United States, the 2012 estimate was 241,740 new PC cases and 28,170 deaths (2). In 2012 in Brazil, there was an estimated 60,180 new PC cases, representing an estimated risk of 62 new cases per 100,000 men (3).
In 1966, based on the histological architecture of the tumor, Donald F. Gleason developed a grading system for PC (4). Many changes have occurred since then (5). The currently accepted classification for the Gleason score (GS) was conceived in 2005, the consensus known as “The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma,” aimed to standardize the score. The result of this consensus was the exclusion of Gleason's pattern 1 in diagnosing prostate carcinoma, the near extinction of pattern 2 and some modifications in the diagnostic standard of patterns 3, 4 and 5 (6).
The Gleason score and prostate-specific antigen (PSA) level are the most important prognostic factors in prostate cancer. Several studies have reported great discrepancy between needle biopsies and radical prostatectomy (RP) specimens. The concordance of the Gleason score depends on certain clinical factors, such as the PSA dosage, number of cores at prostate needle biopsy and experience level of the pathologist. The biopsy Gleason score is a key factor in deciding the appropriate treatment, including selecting patients for RP, external beam radiotherapy (with or without neo and adjuvant androgen suppressive therapy), brachytherapy, expectant management and active surveillance. However, the definitive Gleason score can only be obtained after RP. The RP-based Gleason score appears to be a stronger predictor of PSA-based failure after RP than the biopsy-based Gleason score (7). The discrepancy between the biopsy and RP Gleason scores might result in inappropriate treatment recommendations.
Using population-based data from the pathology reports collected from a southern Brazilian hospital, the purpose of the present study was to examine the concordance between the reported biopsy-based and RP-based Gleason scores and to identify the pretreatment factors, mainly the PSA levels, that could predict an upgrade from a Gleason score of 6 in the biopsy to ≥7 in the RP specimen.
PATIENTS AND METHODSThe patients treated with radical retropubic prostatectomy between 2006 and 2011 were reviewed. Data from 253 patients were analyzed. All prostate biopsies had at least 12 needle cores.
The following exclusion criteria were applied: previous transurethral resection of the prostate (TURP) or open prostatectomy, using 5 alpha-reductase inhibitors (finasteride and dutasteride), adjuvant hormonal treatment, prolonged urethral catheterization, urinary tract infection, symptomatic chronic prostatitis and urinary bladder calculi. Patients with a biopsy Gleason score containing pattern 1 or 2 were also excluded. Based on these criteria, 18 patients were excluded from further analysis: 4 reported with Gleason pattern 2, 7 had previous TURP, 4 had urinary retention using prolonged urethral catheterization, 1 had a urinary tract infection, one was using finasteride and 1 had a preoperative treatment with goserelin.
We compared the Gleason score in the last preoperative cancer-positive needle biopsy with the Gleason score obtained from the surgical specimen. The patients were divided into 4 groups based on the biopsy Gleason score: 3 + 3, 3 +4, 4 + 3 and ≥8. To obtain an accurate prostate weight, the RP specimen description was used.
As some prostate biopsies were evaluated by different pathologists from outside institutions, additional analyses were included to identify any differences in the concordance rates between the biopsies analyzed by outside general pathologists and the staff uropathologist. The effect of PSA on the data analysis was evaluated considering a cutoff value of 10 ng/mL.
In all the analyses, a p-score <0.05 was considered significant. All statistical tests (analysis of variance [ANOVA], Mann-Whitney U-test, Kruskal-Wallis) were performed with SPSS 16.0 software.
This study was approved by the local Research Ethics Committee and acknowledged by the National Commission of Research Ethics (CONEP) and Institutional Review Board (IRB).
RESULTSThe average patient age was 63.3±7.8 years (range 35 to 77 years). The preoperative PSA level in this studied population ranged from 0.8 to 47.2 ng/mL, with a median of 9.3±4.9 ng/mL. The mean prostate weight of the RP specimens was 48.9±19.8 g (19-121 g). The median number of positive core biopsies was 4.0±2.8 (1–14), and 45% of the global sample were bilateral. These data are expressed in Table 1.
Patient demographics, laboratory results and a comparison of the Gleason scores of prostate biopsy (PB) and radical prostatectomy (RP) specimens in the study population.
| Gleason score | ||||||
|---|---|---|---|---|---|---|
| 3+3 | 3+4 | 4+3 | ≥4+4 | TOTAL | p-value | |
| N. of patients | 110 | 73 | 40 | 12 | 235 | - |
| Age (X ± S), years | 63.7±7.1 | 62.4±6.5 | 63.8±6.8 | 64.1±7.8 | 63.3±7.8 | 0.3861 |
| Race | ||||||
| Caucasian (%) | 84 (76%) | 58 (79%) | 30 (75%) | 9 (75%) | 181 (77%) | 1.0002 |
| African-Brazilian (%) | 26 (24%) | 15 (21%) | 10 (25%) | 3 (25%) | 54 (23%) | 1.0002 |
| PSA (X ± SD), ng/mL | 8.6±4.3 | 9.3±5.2 | 15.9±9.4 | 14.5±6.3 | 9.3±4.9 | 0.0011∗) |
| Previous biopsies (X ± SD), n | 0.4±0.8 | 0.3±0.8 | 0.2±0.5 | 0 | 0.3±0.8 | 0.2962 |
| Prostate weight (X ± SD), g | 51.9±21.3 | 45.6±18.5 | 46.5±15.8 | 51.9±16.4 | 48.9±19.8 | <0.0011∗∗ |
| Number of biopsy cores (X ± SD), n | 15.1±4.8 | 13.8±3.7 | 14.9±3.6 | 13.5±3.9 | 14.2±3.9 | 0.5732 |
| Positive cores (X ± SD), n | 3.1±1.9 | 4.6±3.1 | 5.2±2.1 | 9.3±3.6 | 4.0±2.8 | 0.7862 |
| Biopsy positive bilaterally | ||||||
| Yes (%) | 42 (38%) | 31 (42%) | 24 (60%) | 9 (75%) | 106 (45%) | 1.0002 |
| No (%) | 68 (62%) | 42 (58%) | 16 (40%) | 3 (25%) | 129 (55%) | 1.0002 |
| Gleason score | ||||||
| PB = RP (%) | 56 (51%) | 42 (58%) | 20 (50%) | 4 (33%) | 122 (52%) | 0.1842 |
| PB | 54 (49%) | 22 (30%) | 5 (12%) | 2 (17%) | 83 (35%) | 0.2642 |
| PB>RP (%) | - | 9 (12%) | 15 (38%) | 6 (50%) | 30 (13%) | 0.0712 |
Legend:1- ANOVA test; 2 - Mann-Whitney U-test. p<0.05 as significant. PSA: prostate-specific antigen.
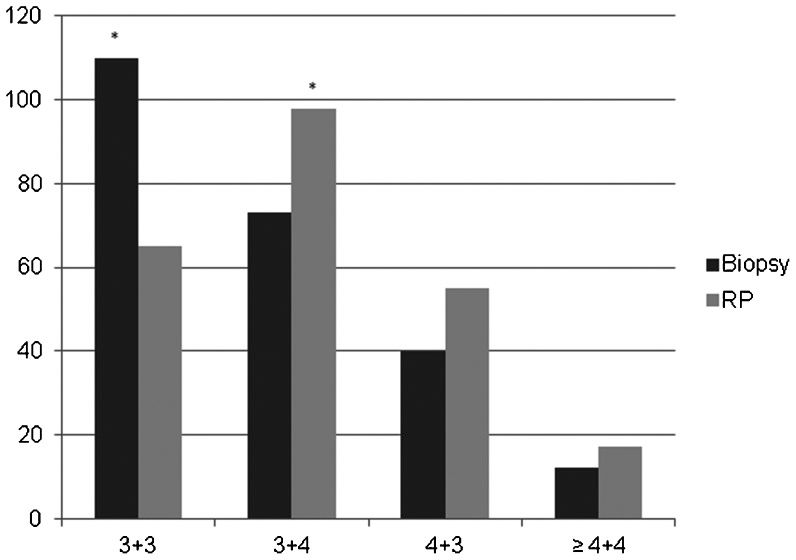
The presence of Gleason scores 3 + 3, 3 + 4, 4 + 3 and ≥8 occurred in 47%, 31%, 17% and 5%, respectively, in the needle biopsies and in 28%, 42%, 23% and 7%, respectively, in the final histopathological analysis of the surgical specimens. The most frequent Gleason scores were 3 + 3 (47%) in the needle biopsy and 3 + 4 (42%) in the RP specimens (p = 0.011). These data are shown in Figure 1.
The preoperative PSA levels were higher in the groups 4 + 3 and ≥8 (p<0.05). There was no significant difference in the mean PSA level between groups 3 + 3 and 3 + 4 (p>0.05).
The median number of biopsy cores was 14.2±3.9, without a significant difference among the 4 groups. The number of previous prostate biopsies among groups 3 + 3, 3 + 4 and 4 + 3 was similar (p>0.05), and all patients in group ≥8 were diagnosed in the first prostate biopsy.
The number of cores positive for malignancy grew with the progression of the Gleason score but did not reach a significant value among the 4 groups (p>0.05). The same effect was observed in the percentage of patients diagnosed with bilateral tumors in the prostate biopsy. The prostate weight was higher in groups 3+3 and ≥8 (p<0.05).
The comparison of the Gleason scores from the biopsy and RP specimens demonstrated identical scores in 122 cases (52%), under-grading in 83 cases (35%) and over-grading in 30 cases (13%) (Table 1). Evaluating 168 of the 235 (71%) cases that had either a needle biopsy or RP specimen analyzed inside our institution, we observed results similar to the global sample: 55% concordance, 32% under-grading and 13% over-grading of the Gleason score in the prostate biopsy (p>0.05).
Overall, 153 (65%) and 82 (35%) patients presented preoperative PSA levels of <10 and ≥10 ng/mL, respectively. The Gleason scores from the biopsy and RP specimens were identical in 86 of 153 patients (56%) and 36 of 82 patients (44%), respectively (p = 0.017). The biopsy Gleason score was underestimated in 45 of 153 (30%) patients with PSA levels <10 ng/mL and 38 of 82 patients (46%) with PSA levels ≥10 ng/dL (p = 0.243). Overestimation of the Gleason score was similar in patients with PSA levels <10 ng/mL and ≥10 ng/dL, (14% vs. 10%, respectively, p = 0.708) (Table 2).
PSA levels, patient demographics and comparison of the Gleason scores of prostate biopsy (PB) and radical prostatectomy (RP) specimens.
| PSA values (ng/mL) | |||
|---|---|---|---|
| <10 | ≥10 | p-value | |
| N. of patients | 153 | 82 | - |
| Age (X ± SD), years | 63.1±7.1 | 64.3±6.5 | 0.3041 |
| Race | |||
| Caucasian (%) | 121 (79%) | 60 (73%) | 1.0002 |
| African-Brazilian (%) | 32 (21%) | 22 (27%) | 1.0002 |
| PSA (X ± SD), ng/dL | 6.5±2.1 | 15.3±6.1 | <0.0011 |
| Previous biopsies (X ± SD), n | 0.3±0.7 | 0.3±0.8 | 0.7812 |
| Prostate weight (X ± SD), g | 47.0±18.8 | 53.0±20.8 | 0.7081 |
| Number of biopsy cores (X ± SD), n | 14.3±3.7 | 13.9±4.7 | 0.7212 |
| Positive cores (X ± SD), n | 3.4±2.2 | 5.3±3.3 | 0.1782 |
| Biopsy positive bilaterally | |||
| Yes (%) | 54 (35%) | 52 (63%) | 0.5162 |
| No (%) | 99 (65%) | 30 (27%) | 0.8972 |
| Gleason Score | |||
| PB = RP (%) | 86 (56%) | 36 (44%) | 0.0172 |
| PB | 45 (30%) | 38 (46%) | 0.2432 |
| PB>RP (%) | 22 (14%) | 8 (10%) | 0.7082 |
Legend:1- ANOVA test; 2 - Kruskal-Wallis test. p<0.05 as significant.
Considering patients with PSA levels <10 ng/dL, the concordance in the Gleason score was 61%, 61%, 33% and 0% for patients in the 3 + 3, 3 + 4, 4 + 3 and ≥8 groups, respectively. Patients with preoperative PSA levels ≥10 ng/dL had concordance in 23%, 50%, 68% and 44% of cases in the 3 + 3, 3 + 4, 4 + 3 and ≥8 groups, respectively.
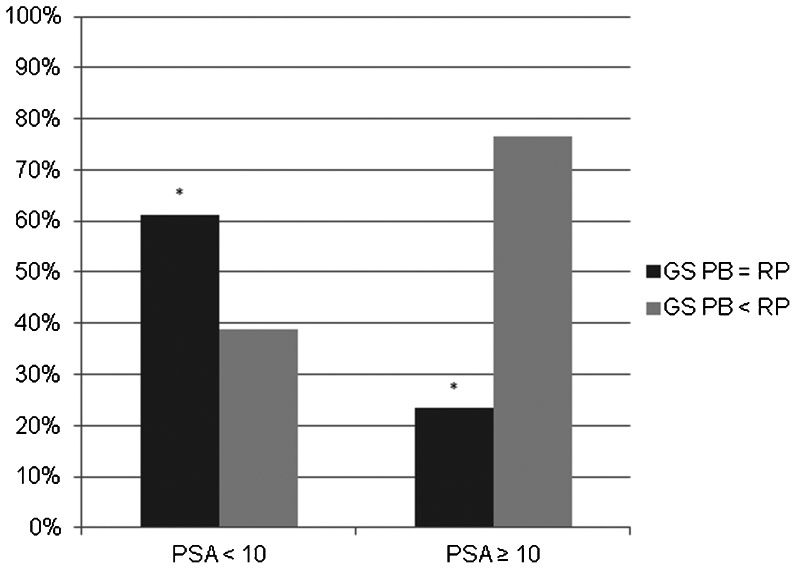
Specifically, patients with Gleason score 3 + 3 in the prostate biopsy demonstrated global concordance in 56 of 110 cases (51%). In this group, patients with a preoperative PSA level <10 ng/mL had higher identical Gleason scores (61%, p = 0.023). With a preoperative PSA level ≥10 ng/mL, this group showed a concordance rate of 23%, resulting in 77% of patients with an upgraded Gleason score after radical prostatectomy (Figure 2).
Concordance of Gleason score (GS) 3 + 3 in the needle prostate biopsy (PB) and radical prostatectomy (RP) according to preoperative prostate-specific antigen (PSA) levels < and ≥10 ng/dL. ∗The patients with preoperative PSA levels <10 ng/dL had higher concordance rates (61% vs. 23%) than the patients with preoperative PSA ≥10 ng/dL (p<0.023). p<0.05 was significant.
According to the literature, the Gleason score discrepancy between the needle prostate biopsy and RP ranged between 35% and 76%. Some of the most important studies (Table 3) have described predictive factors for Gleason concordance (8–21).
Results of the current study and published series regarding the concordance between the Gleason score (GS) of prostate biopsy (PB) and radical prostatectomy (RP) specimens.
| N. of patients | GS PB = RP | GB PB < RP | GS > RP | |
|---|---|---|---|---|
| Steinberg et al. (1997) (8) | 499 | 58% | 36% | 6% |
| Djavan et al. (1998) (9) | 415 | 37% | 50% | 13% |
| D'Amico et al. (1999) (10) | 653 | 35% | 51% | 14% |
| King CR (2000) (11) | 428 | 41% | 42% | 17% |
| Noguchi et al. (2001) (12) | 222 | 36% | 46% | 18% |
| San Francisco et al. (2003) (13) | 126 | 76% | 14% | 10% |
| Chun et al. (2006) (14) | 4,789 | 54% | 33% | 13% |
| Mian et al. (2006) (15) | 225 | 68% | 17% | 15% |
| Divrik et al. (2007) (16) | 392 | 56% | 37% | 10% |
| Kato et al. (2008) (17) | 153 | 50% | 37% | 13% |
| Fine et al. (2008) (18) | 1,455 | 76% | 18% | 6% |
| Kvale et al. (2009) (19) | 1,116 | 53% | 38% | 9% |
| Moreira Leite et al. (2009) (20) | 464 | 57% | 29% | 14% |
| Tapia et al. (2011) (21) | 168 | 63% | 27% | 10% |
| Current study | 235 | 52% | 35% | 13% |
The rates of discrepancy are influenced by the number of biopsy cores. This aspect could be observed in the elegant study conducted by San Francisco et al., which observed an exact concordance of 76% for 12 core biopsies and 63% for 6 core biopsies (13). Additionally, Mian et al. (15) described concordance rates of 68% and 48% for a mean of 12.4 and 6.7 cores, respectively. Today, the discussion about the number of cores in s prostate biopsy is obsolete because sextant biopsy is no longer considered adequate (22). The British Prostate Testing for Cancer and Treatment Study has recommended a minimum of 10 core biopsies (23). Taking more than 12 cores is not significantly more conclusive (24).
Some articles have also described that the reproducibility of the Gleason score depends on the pathologist's experience and education level (19). However, in our series, there was not a significant difference in Gleason score concordance between the prostate biopsy analyses performed inside and outside our institution. The consensus conference in 2005, which was organized by the International Society of Urological Pathology (ISUP) (6), modified the Gleason grading system, eliminating pattern 1 and almost extinguishing pattern 2; this change might reduce the difference between high and low volume pathology units (19). In addition, ignoring <5% of Gleason pattern 3 at biopsy in the presence of pattern 4 or 5 was recommended. The updated grading system may be one reason why the most recent studies have shown a higher concordance in the Gleason scores, as shown in Table 3.
Most studies (14–21) performed after the resolution of the ISUP Consensus, including the current study, have demonstrated a rate of concordance ranging from 50% to 76%; in contrast, in studies published before 2005, the concordance rate ranged from 35% to 76% (8–13). Interestingly, San Francisco et al. (2003) demonstrated a higher concordance in their series, which may be attributed to the fact that a different extended biopsy approach was adopted, whereas most prior studies have included biopsies with fewer than 10 cores.
The importance of the preoperative PSA levels and their correlation with the Gleason score has also been described. Kvale et al. (19) described 39%, 50% and 57% Gleason upgrading rates in radical prostatectomy with PSA levels of <10, 10 to 14.9 and ≥15 ng/mL, respectively; interestingly, the upgrading of the Gleason score was associated with increasing PSA levels. In the current study, considering PSA values < and ≥ than 10 ng/mL, a similar relationship could be observed (Table 2). The most concerning issue is that approximately 80% of the patients with Gleason scores of 3 + 3 and PSA levels of ≥10 ng/mL were upgraded after their RP surgical specimens were analyzed. This observation indicates that PSA levels ≥10 ng/mL with Gleason scores <7 should be carefully evaluated.
There are some implications associated with this conclusion. As a PSA level ≥10 ng/dL excludes patients from being diagnosed as low-risk, according to D'Amico (25), the prostate cancer risk classification also excludes these patients from being offered transperineal brachytherapy or active surveillance. Indeed, if radiation therapy is the chose curative modality treatment, hormonal therapy should be added (26).
These data highlight the necessity of obtaining a reliable Gleason score, which is not always possible with a prostate biopsy. We emphasize that regardless of the available treatment options after a prostate cancer diagnosis, the Gleason score directly influences the treatment modality to be used (e.g., the extent of pelvic lymphadenectomy in RP, the dose of radiotherapy and its association or not with androgen deprivation therapy, the possibility of performing brachytherapy or even active surveillance). Establishing the final Gleason score by prostate biopsy alone is highly questionable and might involve making decisions based on data that are not always correct. Additionally, this study discusses the importance of PSA levels in the actual prostate cancer itself and in determining the best treatment option.
In conclusion, the Gleason scores of the needle prostate biopsies and those of the radical prostatectomy specimens were concordant in approximately half of the global sample. Moreover, the real impact of our results was in highlighting the importance of the preoperative PSA level in the concordance of the Gleason score. Together with clinical factors, the preoperative PSA level may improve the identification of those patients who tend to be upgraded after surgery, mainly the patients with the 3 + 3 Gleason score in the prostate biopsy with a preoperative PSA ≥10 ng/mL. Despite efforts of the ISUP to standardize Gleason score analyses, the discrepancy between biopsy and RP persists.
AUTHOR CONTRIBUTIONSLima NG collected the retrospective study data, wrote and reviewed the manuscript. Soares DF collected the retrospective study data. Rhoden EL wrote and reviewed the manuscript.
No potential conflict of interest was reported.