The concept that extracorporeal shock wave lithotripsy (ESWL) may be used to successfully fragment urinary calculi in a noninvasive manner has revolutionized the management of urolithiasis.1 Complications of this procedure are usually limited to the kidneys and almost always resolve spontaneously.2 Whereas subcapsular renal hematomas have been present in up to 15% of patients in radiological studies,3 hepatic hematomas have been reported only anecdotally and, to our knowledge, no case of infected hepatic hematoma has been previously described. The authors report a case of a patient who had an infected hepatic hematoma as a late complication of ESWL.
A 35-year-old woman presented with a 1-year history of recurrent right renal colic and episodic macroscopic hematuria. The patient’s medical history was unremarkable, and she was taking no medication. Physical examination disclosed an apparently healthy patient with no abnormality, with arterial blood pressure of 115/70 mm Hg. A plain radiograph of the abdomen, an ultrasound examination, and an excretory urogram (IVP) showed a 7-mm stone in the middle calices of the right kidney. Extracorporeal shock wave lithotripsy was then performed with a Dornier Compact-S lithotriptor requiring 5500 shocks at a potency of 6 (on a 1-9 scale). There was apparently no difficulty with stone fluoroscopic localization.
Thereafter, the patient had 30 days of continuous pain in the flank and right upper quadrant. A plain radiograph of the abdomen disclosed a 4-mm stone in the pelvis of the right kidney. Ultrasound examination was not performed, as the stone was thought to be the cause of the pain. Extracorporeal shock wave lithotripsy was repeated under fluoroscopic guidance. The stone was completely fragmented with 2500 shocks at a potency of 6. In none of the ESWL procedures were antibiotics used, following the standard protocol of our service.
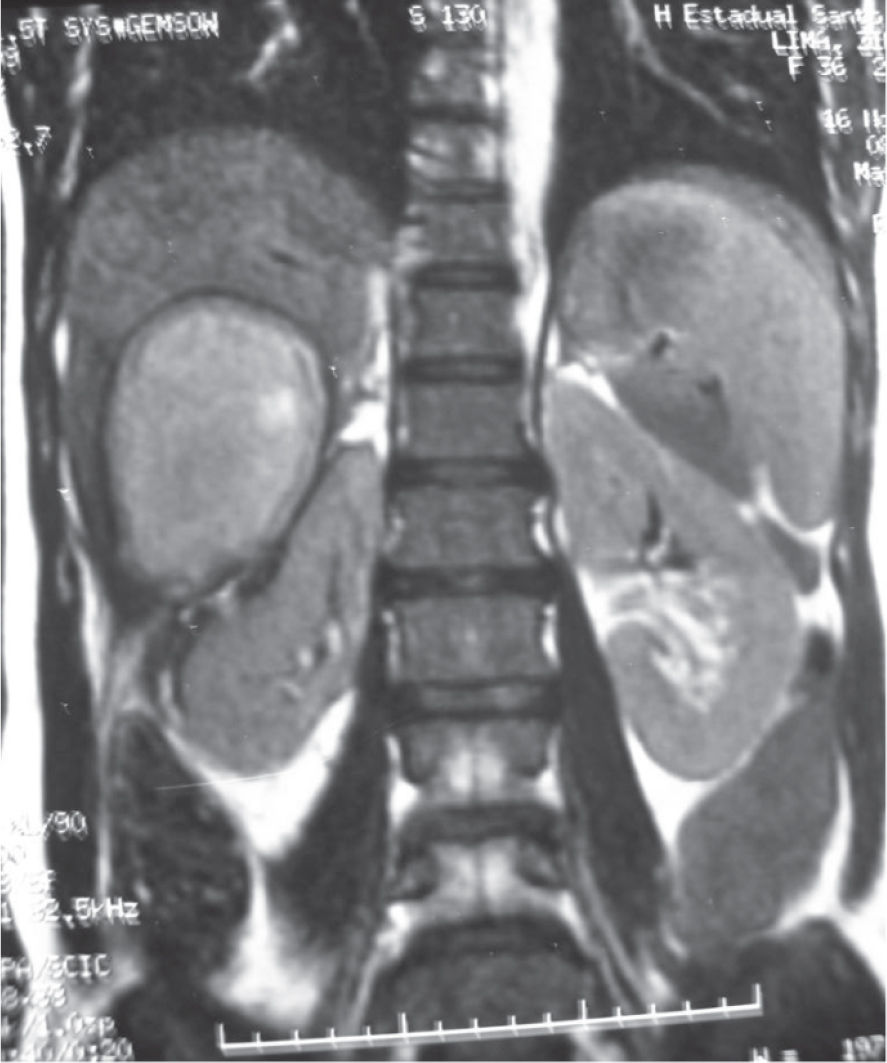
Right upper quadrant pain persisted in the same fashion for 2 more consecutive months, now associated with occasional fever and weight loss (5 kg). Physical examination showed tenderness of the right upper quadrant of the abdomen. Hemoglobin was 12.2 g%, white blood cells 11800 mm3, urea 36 mg/dL, and creatinine 0.9 mg/dL. The urine culture was negative. Abdominal ultrasound revealed a 9.9 x 6.7 x 7.6-cm heterogenic mass in the inferior portion of the right hepatic lobe. All tumor markers for liver were negative. A computed tomography (CT) of the abdomen demonstrated a round, 6.0-cm diameter collection of fluid and air in the undersurface of the right hepatic lobe (Figure 1). A magnetic nuclear resonance (MRI) of the abdomen disclosed a 7.0-cm diameter homogeneous mass in the right hepatic lobe, suggestive of a hepatic abscess (Figure 2).
Computed tomography image of the abdomen showing a gas-containing fluid collection in the inferior portion of the right hepatic lobe, suggesting an infected collection. Abdominal ultrasound revealed a 9.9 x 6.7 x 7.6-cm heterogenic mass in the inferior portion of the right hepatic lobe in close contact with the right kidney.
The fluid collection was percutaneously drained, revealing 60 mL of brownish viscous fluid, suggesting a liquefied hematoma. Culture showed Klebsiella sp as an infecting organism. Fourteen days of third generation cephalosporin were administered. The symptoms subsided, and the follow-up CT showed no residual fluid.
Extracorporeal shock wave lithotripsy is known to induce acute structural changes in the treated kidney in most treated patients. The two most common renal side effects after ESWL are hemorrhage and edema within or around the kidney. Isolated cases of hepatic hematoma when ESWL is performed in the right kidney have been reported,2,4 although infection occurred in none, in contrast to the case with our patient.
Defined risk factors for renal hematoma after ESWL are pre-existing hypertension and the use of aspirin-containing compounds.5 There is no correlation with the number of shocks or with their potency. However, neither in our case nor in the cases so far reported in the literature were these risk factors present in patients developing hepatic hematoma. The presentation of hepatic hematoma after ESWL may be of an asymptomatic patient with a control image study disclosing the lesion,2 but most patients with hepatic hematoma have continuous abdominal pain after ESWL.4 Therefore, in the present case, this diagnosis or the diagnosis of perirenal hematoma should have been suspected after the first ESWL, and the patient should have been studied. Fever and weight loss in our patient suggested an associated subacute infection. MRI and CT scans are more sensitive for detecting renal hemorrhage after ESWL. We believe this is also true for hepatic hematomas.
Expectant treatment has been successful in hepatic hematomas after ESWL.2 However, when a hepatic abscess is suspected, percutaneous drainage may be advisable, as in the cases described by Meyer (1995) and herein.
Hepatic hematoma after ESWL is a rare complication, and this is the first reported case of infected hepatic hematoma after ESWL. Hepatic hematoma should be suspected in any patient with persistent abdominal pain after ESWL, when an imaging study is usually diagnostic. Whereas most simple hematomas subside spontaneously, percutaneous drainage is necessary whenever infection is suspected.