In Brazil, patients with chronic myeloid leukemia (CML) in the chronic phase were not given first-line imatinib treatment until 2008. Therefore, there was a long period of time between diagnosis and the initiation of imatinib therapy for many patients. This study aims to compare the major molecular remission (MMR) rates of early versus late imatinib therapy in chronic phase CML patients.
METHODSBetween May 2002 and November 2007, 44 patients with chronic phase CML were treated with second-line imatinib therapy at the Hematology Unit of the Ophir Loyola Hospital (Belém, Pará, Brazil). BCR-ABL transcript levels were measured at approximately six-month intervals using quantitative polymerase chain reaction.
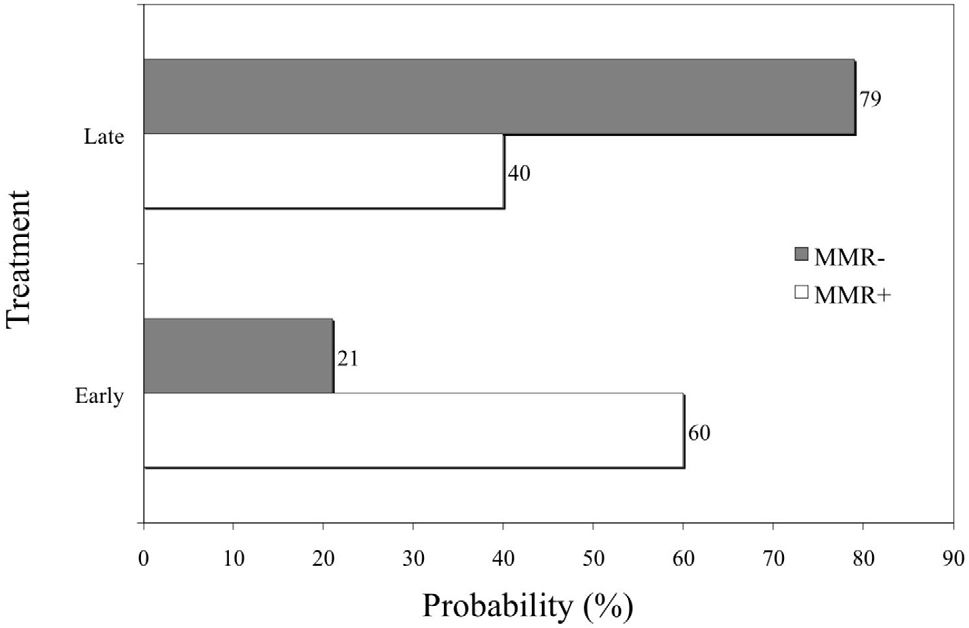
RESULTSThe early treatment group presented a 60% probability of achieving MMR, while the probability for those patients who received late treatment was 40%. The probability of either not achieving MMR within one year of the initiation of imatinib therapy or losing MMR was higher in patients who received late treatment (79%), compared with patients who received early treatment (21%, odds ratio=5.75, P=0.012). The probability of maintaining MMR at 30 months of treatment was 80% in the early treatment group and 44% in the late treatment group (P=0.0005).
CONCLUSIONSFor CML patients in the chronic phase who were treated with second-line imatinib therapy, the probability of achieving and maintaining MMR was higher in patients who received early treatment compared with those patients for whom the time interval between diagnosis and initiation of imatinib therapy was longer than one year.
Chronic myeloid leukemia (CML) is a disease that originates from a hematopoietic stem cell characterized by the reciprocal chromosomal translocation t(9;22) (q34;q11). This chromosomal translocation, also known as a Philadelphia (Ph) chromosome, is responsible for the formation of the fusion gene BCR-ABL.1,2 This chimeric gene codes for a cytoplasmic protein with constitutive tyrosine kinase activity, which has a fundamental role in the leukemogenic process.3,4
Historically, CML treatment was unable to halt the course of the disease, and almost all patients progressed to the blastic phase of CML after three to five years. Recently, however, imatinib mesylate has been found to induce hematologic and cytogenetic remission and, consequently, to modify the progression of CML.5 Cytogenetic remission is considered an important parameter for assessment of the therapeutic success of imatinib treatment.6 However, even patients with cytogenetic remission may present minimal residual disease7 that can only be detected by polymerase chain reaction (PCR).8 Real-time PCR (RT-PCR) from cDNA allows for the quantification of BCR-ABL transcript levels with a sensitivity of one in one hundred thousand cells. In patients with complete cytogenetic remission, quantification of this molecular response by RT-PCR correlates with the duration of remission of the disease.8,9
In Brazil, federal health authorities did not reimburse first-line imatinib therapy for patients with CML in the chronic phase until 2008. In many cases, this circumstance led to a long time interval between diagnosis and the initiation of imatinib therapy, which was eventually reimbursed only after patients had progressed to the accelerated phase or become intolerant to interferon therapy. The objective of this study was to compare the major molecular remission (MMR) rates of patients receiving early versus late imatinib therapy after the diagnosis of CML.
METHODSPatientsBetween May 2002 and November 2007, we evaluated 44 patients with chronic phase CML who were undergoing treatment at the Hematology Unit of the Ophir Loyola Hospital. All patients received second-line imatinib therapy (400 mg/day), due to intolerance or resistance to interferon, according to the criteria laid out in Resolution SAS 431 of the Ministry of Health of Brazil (2001). Two groups were established according to the time interval between the diagnosis of CML and the initiation of imatinib therapy: the early treatment group (time interval shorter than one year between diagnosis and treatment) and the late treatment group (time interval more than one year). MMR was defined as a reduction of at least three logs (0,1%) in relation to the baseline (100%) in BCR-ABL transcript levels.
The Brazilian National Ethical Committee approved this study in June 2001 (no. CONEP 2318).
Quantitative real-time polymerase chain reactionRT-PCR (TaqMan, Applied Biosystems) was utilized to quantify BCR-ABL expression relative to the control gene ABL, according to Lemos et al.10 The control gene ABL was chosen according to the recommendation of Europe Against Cancer (EAC).11,12
BCR-ABL transcript quantification based on the international scaleReduction in the BCR-ABL transcript level was calculated on the basis of the international scale,13 by direct calculation of the cycle threshold (CT) for the BCR-ABL/ABL ratio was employed, according to Lemos et al.,10 but without the use of the standard curve. To calculate the basal BCR-ABL transcript levels, the mean BCR-ABL/ABL (BCR-ABLL%) ratios of 38 patients were obtained before the initiation of imatinib therapy; 11 of these patients had the B2A2 transcript, and 29 had the B3A2 transcript. The difference in the transcript levels between the two groups was not statistically significant. Afterward, the MMREq was calculated, which is the BCR-ABL/ABLL equivalent of MMR established in the International Randomized Study of Interferon and STI571 (IRIS).14 The conversion factor (CF) was then calculated to convert the results to the international scale, dividing 0.1 (the value attributed to MMR on the international scale) by the MMREq value. Finally, the CF was multiplied by BCR-ABLL to obtain the quantification according to the international scale (BCR-ABL/ABLIS).
Statistical analysisSimple logistic regression was utilized to calculate the probability of MMR in the early and late treatment groups. The difference between the time of CML diagnosis and the initiation of imatinib therapy in the group achieving MMR and the group not achieving MMR was evaluated by Student’s t-test for independent samples. Maintenance of MMR was estimated by the Kaplan-Meier method, considering a reduction of ≥3 logs of BCR-ABL expression as the event of interest. The level of significance was set at 0.05 (two-tailed).
RESULTSOf the 44 patients evaluated, 18 (41%) were men, and 26 (59%) were women. Their ages ranged from 22 to 76 years, with a median age of 49 years. In 16 patients (37%), the time interval between the diagnosis of CML and the initiation of imatinib therapy was shorter than one year; in 28 patients (63%), this time was one year or longer.
The probability of achieving MMR was 60% in the group who received early treatment, versus 40% in the late treatment group. The probability of not reducing BCR-ABL transcript levels by three logs within one year of treatment, or of losing MMR, was 79% in the late treatment group and 21% in the early treatment group (P=0.012, odds ratio=5.75) (Figure 1).
The patients who sustained MMR up to the thirtieth month of treatment started the use of imatinib about 14.4 months after the diagnosis (standard deviation [SD], 13.6 months) (Figure 3). The patients who achieved MMR showed a probability of maintaining MMR after 30 months of therapy of 80% if they received early treatment with imatinib. On the other hand, this probability was only 44% for patients who received late treatment (P=0.0005) (Figure 2).
In the 2003 IRIS study,14 39% of patients with CML in the chronic phase who received first-line imatinib therapy showed a reduction of three logs in their BCR-ABL transcript levels within the first year of treatment. Moreover, patients achieving molecular remission showed a smaller risk of progression over the next 12 months. In the present study, the MMR rate was 31%, and the mean duration of MMR was 26 months (SD±15). The difference in MMR rates between the IRIS study and this one could be attributed to different time intervals between diagnosis and the initiation of imatinib therapy in each study. In the IRIS study, patients with recently diagnosed and previously untreated CML received first-line imatinib therapy, while in our study, imatinib was used as a second-line therapy. In a study conducted by Aziz et al. in Pakistan, the authors concluded that the biology of CML in Pakistani patients was not different from that in patients from developing countries.15 However, regarding Brazil, local treatment policies have delayed the initiation of imatinib therapy, thus affecting the results regarding molecular remission rates, which otherwise could be similar to those results observed in the IRIS study.
Matsuo et al. evaluated 99 patients with CML in the chronic phase treated with imatinib; 43 of these patients had been recently diagnosed, and 56 patients had been previously treated. The overall survival and progression-free survival rates were 88.7% and 85.2%, respectively, in the first group and 79.8% and 76.6% in the second.16 Because no statistically significant differences were observed in any of the main study endpoints, the authors concluded that patients receiving first-line imatinib therapy have the same outcome as those patients who had been previously treated with interferon or hydroxyurea. However, the authors did not report the time interval between diagnosis and the initiation of imatinib therapy, suggesting that the time elapsed between diagnosis and initiation of imatinib therapy in the previously treated group was not long enough to produce a meaningful difference.
In the present study, due to Brazilian federal legislation that would not reimburse first-line imatinib therapy until 2008, all patients received previous treatment with another drug. Because of the large variation in the time interval between diagnosis and the initiation of imatinib therapy, reaching up to 192 months, it was possible to define two different groups according to this variable. The probability of achieving MMR was significantly higher in the early treatment group, compared with the late treatment group.
The exact time interval between diagnosis of CML and the initiation of imatinib therapy that discriminates between early and late treatment is not well defined in the literature. We found that patients who sustained MMR up to the thirtieth month of therapy initiated imatinib therapy approximately one year after the diagnosis (mean of 14.4 months) (Figure 3). We also observed that patients who started imatinib therapy within one year of diagnosis had an 80% probability of sustaining MMR into the thirtieth month of treatment, while in the late treatment group, this probability was reduced to 44%.
Therefore, in view of our results, we suggest that 12 months should be considered the upper limit of the time interval for initiating imatinib treatment for CML. Moreover, after this time interval, the probability that a patient will lose MMR increases considerably.