Drug hypersensitivity reactions are adverse reactions to drugs that were administered at a dose that is tolerated by normal subjects, but produce symptoms that, from a clinical perspective, resemble an allergy. The revised nomenclature for allergies classifies hypersensitivity reactions to drugs as either allergic or non allergic. Drug allergies occur when immunologic mechanisms have been demonstrated.1
Allergic reactions caused by antifungal drugs are not frequently reported in clinical practice. Until now, the pathogenesis of hypersensitivity reactions to ketoconazole and other azole derivatives is unknown.2 Herein, we report an immediate reaction to ketoconazole and review the usefulness of a drug provocation test for diagnosis.
CASE DESCRIPTIONA 40-year-old man began oral treatment with ketoconazole at a dosage of 400 mg per day for prophylaxis of candidiasis. Forty minutes after administration of the first dose, he developed angioedema of the face in addition to generalized urticaria. The symptoms were quickly reduced by administration of parenteral steroids and anti-histaminics. Notably, the patient had no personal or familiar history of allergies. In addition, while the patient had never taken this drug before, he had taken fluconazole approximately one year ago without noticing any adverse reactions. The patient denied the use of any other medicine at the time of taking ketoconazole and indicated that he did not have any previous episodes of urticaria or angioedema.
Skin prick tests with ketoconazole at a concentration of 1, 10, 20, and 40 mg/ml were all negative. A single blind placebo controlled oral challenge test with commercial ketoconazole (200 mg) was performed, showing an immediate response characterized by urticariform exanthema and angioedema within 50 minutes from ingestion of the drug. Parenteral hydrocortisone (200 mg) and diphenidramine (50 mg) were subsequently administered after which the symptoms were abated. In addition, no late response to the drug was observed.
DISCUSSIONDrug hypersensitivity can affect as many as 12 % of the general population, whereby non-steroid anti-inflammatory drugs and antibiotics are the most frequently implicated drugs.3 This case, which involves an immediate hypersensitivity to ketoconazole, is extremely rare and in fact, this is the first case study suggestive of an allergic reaction to ketoconazole to be reported in Brazil.
Immediate drug hypersensitivity occurs within the first hour after drug administration and is probably mediated by an IgE-dependent mechanism. The reaction, from a clinical perspective, is characterized by urticaria, angioedema, rhinitis, bronchospasm and anaphylactic shock. This patient presented an immediate reaction that was characterized by a rapid onset of the aforementioned symptoms (urticaria and angioedema).
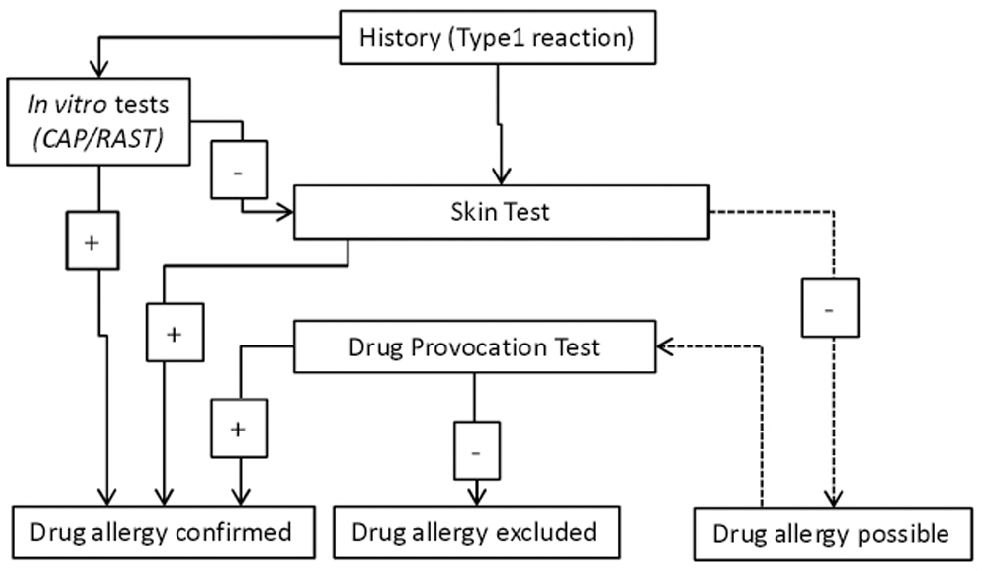
The diagnosis of an immediate hypersensitivity reaction should include both in vitro and in vivo tests (Figure 1).
However, the required serum specific IgE assays are only available for a few drugs, not including the azole derivatives. Additional in vitro tests, such as the flow cytometric basophil activation test, have not yet been validated, and their sensitivity is not 100 %.4
Skin tests are the most readily available method for physicians to test for the presence of an allergy. Currently, skin prick tests to determine if there is an allergy to a specific drug can only be validated for beta-lactam antibiotics and insulin. Due to their greater sensitivity, skin tests cannot be replaced by in vitro tests. The skin prick test administered in this case study was performed as described previously for ketoconazole.5 However, unlike the results from this previous report, our results were negative. This was probably due to the lack of a standardized procedure for administering the prick test for ketoconazole.
The drug provocation test (DPT) is the gold standard for the identification of an eliciting drug when allergologic tests results are negative, not available, or cannot be validated. As recommended by the European Network for Drug Allergy, the commercial preparation of the drug was administered in the same way as it was administered when the reaction occurred. The starting dose was 10 % of the therapeutic dose, with an increasing dose of 20 % of the therapeutic dose to be administered 20 minutes after the starting dose.6 However, the first symptoms appeared prior to the second dose, whereby the test was stopped.
Despite its potential risk, the DPT was useful in this particular case since ketoconazole was not a frequent cause for a reaction. In this case, avoiding ketoconazole will prevent other severe reactions. Since cross-reactivity between azole derivatives is possible, a DPT should be performed before the use of another drug from this group.