Pulmonary alveolar microlithiasis (PAM) is a rare idiopathic lung disease, characterized by the formation and accumulation of tiny, round corpuscles called “microliths” that consist primarily of calcium and phosphorus mixed with small amounts of magnesium and aluminum1. Most of the reported cases are of patients between 20 and 40 years of age. Autosomal recessive inheritance has been suggested to be a possible cause of the disease. Clinical features vary, and some patients may be asymptomatic for a long time until pulmonary function testing begins to demonstrate lung impairment along with progressive fibrosis and the development of a restrictive ventilatory defect culminating in cardiorespiratory decompensation.2 Currently, there is no medical therapy capable of definitively changing the progression of the disease. Lung transplantation is required once end-stage lung disease is established. To date, seven patients have received lung transplantation for this condition. We report a successful case of bilateral sequential lung transplantation in a patient with PAM.
CASE DESCRIPTIONA 47-year-old man was referred for lung transplantation due to shortness of breath. He reported dyspnea that began two years prior to his presentation in our clinic, with progressive worsening that eventually required oxygen. There was no history of smoking or previous pulmonary disease, except for a history of tuberculosis 30 years prior, for which he had received treatment. On physical examination, there was marked digital clubbing, mild cyanosis, cor pulmonale and bilateral prominent inspiratory crackles. Chest X-ray showed bilateral pleural thickening, elevation of the hilum and diffuse interstitial opacity. A computed tomography (CT) scan demonstrated thickening of the interlobular septa and interstitia, lymph node enlargement, pleural thickening with calcification, ground glass opacity and areas of honeycombing due to multiples nodules diffusely distributed over the parenchyma (Figure 1). An echocardiogram showed pulmonary hypertension, left ventricular diastolic dysfunction and right systolic dysfunction. Open lung biopsy revealed PAM. Prednisone treatment was initiated, with partial improvement as a result. There was no family history of similar disease. He showed a restrictive ventilatory defect on pulmonary function test, with a Forced Expiratory Volume in 1 second (FEV1) of 1.63 L (46% of the predicted value), a Forced Vital Capacity (FVC) of 1.84 L (43% of predicted) and an FEV1/FVC ratio of 0.89 (108% of predicted).
The patient underwent bilateral lung transplantation after fourteen months on the waiting list. The procedure was performed by clamshell incision. The left lung was transplanted first, and cardiopulmonary bypass was necessary for 135 minutes due to hemodynamic instability. The right lung was transplanted without cardiopulmonary bypass. Total ischemic time was 540 minutes.
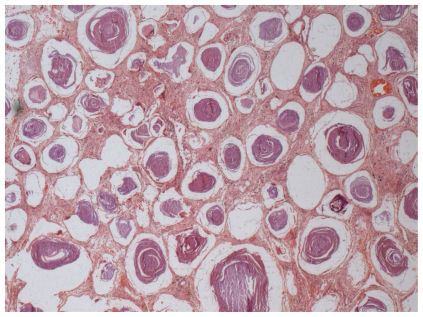
Histological examination showed PAM with foci of metaplastic ossification, extensive cicatricial fibrosis, primarily in the peripheral areas, and paraseptal emphysema in the apical portion of the upper lobes with formation of subpleural bubbles (Figure 2). In the early postoperative period, the patient presented with pulmonary reperfusion syndrome, distributive shock and acute renal failure, requiring dialysis for 26 days. Total mechanic ventilation time was 6 days, and ICU stay was 38 days. Immunosuppressive therapy was initiated with tacrolimus, sodium mycophenolate and prednisone. The patient progressed uneventfully with total recovery of renal function and remained well twelve months after transplantation, as may be observed from his current of 2.61 L (75% of pulmonary function testing results: FEV1 predicted), FVC of 3.43 L (81% of predicted) and FEV1/FVC ratio of 0.76 (92.2% of predicted).
DISCUSSIONAlthough the first cases of PAM were described by Malphighi, the disease was first named by Phur.3 The disease exists on all continents, without regional or ethnic differences, although most of the cases (37%) have been reported in Europe and Asia Minor. Turkey is the country with the highest prevalence (16.3%), followed by Italy and the USA. The etiology of the condition remains unknown, although some theories have been posited. One theory is based on an exudate that is not easily absorbed and that is formed as a result of an abnormal inflammatory response to infections or irritants, ultimately undergoing calcification. It is also postulated that a condensation of alveolar mucus due to a deficiency in mucociliary clearance is the cause of the disease. However, the most accepted hypothesis is that mucopolysaccharide deposition, triggered by increased alkalinity secondary to inborn errors in metabolism involving the carbonic anhydrase enzyme at the alveolar interface, promotes the local accumulation of calcium salts.4,5
Diagnosis is usually made between the second and third decade of life; however, the age group can be highly variable. The disease has been reported in neonates and octogenarians. In the present case, diagnosis occurred at the age of 45. The condition is sometimes misdiagnosed as miliary tuberculosis. Family history is present in 37% to 56% of the cases. In cases where there is a family history, a higher incidence in females has been described (53.3%). Otherwise, in sporadic cases, the predominance is higher in males (61.3%).2,3
The typical picture of PAM on chest X-ray is of fine, sand-like calcific micronodules (sandstorm lung) diffusely infiltrating both lungs; these characteristics are usually observed in the middle and lower zones.6 The protrusion of microliths under the visceral pleura may cause the granular aspect often present on the external surface of the lungs. On the anterior margin and at the apex, areas of bullous emphysema may also be found. CT scans demonstrate micronodular calcific densities with a greater concentration in the subpleural parenchyma and along the bronchovascular bundles, whereas high resolution CT scans show thickening of the lobular septae with a distribution of microliths along the septae and around the centrilobular distal bronchioles.
On gross examination, apical blebs and bullae may be present, and the lungs appear to remain inflated and are described as heavy with gritty texture (Figure 2). Concentrically laminated concretions (1 to 3 mm in diameter) may be found inside the alveoli, which are often considered normal, although diffuse interstitial fibrosis may be observed in more severe cases (Figure 3).
At present, there is no medical treatment capable of reducing the progression of the disease. Systemic corticosteroids, calcium-chelating agents and serial bronchopulmonary lavage have been shown to be ineffective and are used as palliative treatments. The use of diphosphonate has been proposed to reduce calcium phosphate precipitation in pulmonary alveoli.7 However, this therapy remains controversial given the limited number of reports in the literature.
Lung transplantation remains the only possible treatment for end-stage cases8. Nonetheless, decisions regarding the time at which transplantation should occur are not fully established due to the lack of well-defined prognostic indices and the insidious nature of PAM9. When either right heart failure or severe respiratory failure with a requirement for oxygen is present, as was the case in our study, transplantation should be considered. In order to maximize the chances of a successful outcome, patients should be referred before the development of severe right ventricular dysfunction. In the only postoperative death reported after bilateral lung transplantation, prolonged cardiopulmonary bypass (six hours) in combination with extensive pleural involvement and increased vascularity led to uncontrolled hemorrhagic complications. Shigemura et al. have reported the oldest successful lung transplant recipient, with ten years of follow-up.10
Bilateral lung replacement is preferred to unilateral replacement, because the replacement of only one lung might result in persistent shunting of blood through the native lung, as PAM leads to filling of the alveolar spaces and the consequent creation of large areas of intrapulmonary shunt.11 However, two patients have undergone a single lung transplantation with acceptable results and have had no evidence of recurrence in the transplanted lung thus far.12,13 Furthermore, even for bilateral transplantation, it is not known whether PAM can recur. Recurrence after transplantation has not been reported to date, suggesting that, in fact, PAM is a result of local inflammatory responses or a genetically determined error in alveolar metabolism, rather than a systemic disorder. Increased right ventricular ejection fraction and the regression of right ventricular hypertrophy are examples of heart function recovery after bilateral lung transplantation, which is an effective treatment option for end-stage PAM patients, despite the reduced number of reported cases worldwide.