After burn injuries, scarred skin lacks elasticity, especially in hypertrophic scars. Topical treatment with tretinoin can improve the appearance and quality of the skin (i.e., texture, distensibility, color, and hydration). The objective of this prospective study was to examine the effects of treatment with 0.05% tretinoin for one year on the biomechanical behavior and histological changes undergone by facial skin with post-burn scarring. Setting: Tertiary, Institutional.
METHOD:Fifteen female patients who had suffered partial thickness burns with more than two years of evolution were selected. Skin biopsies were obtained initially and after one year of treatment. The resistance and elastance of these skin biopsies were measured using a mechanical oscillation analysis system. The density of collagen fibers, elastic fibers, and versican were determined using immunohistochemical analysis.
RESULTS:Tretinoin treatment significantly lowered skin resistance and elastance, which is a result that indicates higher distensibility of the skin. However, tretinoin treatment did not significantly affect the density of collagen fibers, elastic fibers, or versican.
CONCLUSION:Topical tretinoin treatment alters the mechanical behavior of post-burn scarred skin by improving its distensibility and thus leads to improved quality of life for patients.
The evolution of medical knowledge and techniques, including improved intensive care units and surgical procedures, has increased the survival of major burn patients.1–3
Burn victims live with sequelae that may decrease their self-esteem and, therefore, their quality of life. A specialized multi-disciplinary professional team that can treat the multiple aspects of rehabilitation is critical for the proper re-integration of patients into their familiar professional and social environments. Post-burn scars induce profound changes in skin structure, such as epidermal and dermal abnormalities. Within the dermis, changes in the extracellular matrix (ECM) include increased concentrations of collagen fibers, which can be arranged in whorls or nodules, and decreased levels of elastic fibers.4,5 Versican, a proteoglycan with hydrophilic properties, is usually present in large amounts in recent hypertrophic scar tissue. As the scar matures and becomes less rigid, the amount of versican decreases.4 After tissue repair, alterations in ECM composition and organization lead to changes in the mechanical properties of the skin that result in decreased elasticity, especially in hypertrophic scars.4, The severity of these changes varies, depending on the depth of the original injury and other factors. When spontaneously restored, burns that involved deep dermal injury can take from three to five weeks to epithelize completely. Injuries that take longer to epithelize are more likely to evolve with hypertrophy.9
Due to the limitations of surgical techniques, many burn patients require additional treatment to improve the texture and appearance of their skin.10,11 The use of topical tretinoin improves the appearance of keloids and hypertrophic scars and seems to increase skin elasticity in scar sequelae.12–15 The topical use of tretinoin with glycolic acid in both restored skin and in grafted skin has been shown to increase the extent of mouth opening in burn patients with facial scarring.10
Several studies addressing the properties of post-burn scars or their cicatricial sequelae have characterized the tegument qualitatively by examining coloration, smoothness (texture, flexibility), or thickness. Previous authors have highlighted the importance of using objective measurements to analyze skin mechanical properties with such equipment as linear extensometers or cutometers (devices that measure cutaneous elasticity by suction).6,7 Measurements of skin elastance have been used in studies assessing the mechanical properties of the skin in patients with systemic sclerosis.16 Using an instrument called an “elastometer,” the skin elastance of these patients was found to be significantly greater than that of control individuals. In addition, this measurement was correlated with clinical scores that indicated thickening.17 In our hands, these devices (i.e., extensometers, autometers, and elastometers) did not provide homogeneous measurements when we attempted to reproduce these data in pilot studies. An alternative method of measuring the mechanical oscillation of tissue using a computer to record tissue resistance and elastance has been described for analyzing lung tissue in various diseases.18,19 The mechanical oscillation of tissue has been used previously to assess the viscoelastic properties of the superficial aponeurotic muscle system in rhytidoplasties20, but it has not yet been used for skin.
To investigate more accurately the reported improvements in the distensibility of post-burn scarred skin after topical treatments with tretinoin, we examined skin tissue using mechanical oscillation analysis to measure biomechanical behavior and immunohistochemistry to study possible mechanisms underlying these improvements.
METHODSFifteen female patients between 18 and 40 years of age (mean age = 26.7) were included in the study. These patients exhibited residual facial scars resulting from superficial partial thickness facial burns that had been caused by ethanol and spontaneously restored with conservative treatment two or more years before. All patients signed an informed consent form approved by the Review Board and Ethics Committee of the institution in accordance with the Declaration of the World Medical Association (number 515/5). Exclusion criteria included previous surgeries, corticosteroid treatment, keloid scars, systemic diseases, pregnancy, and smoking. All patients were instructed to use contraceptive methods because of the potential teratogenic effects of tretinoin.
All selected patients had whole-face scarring. At the beginning of the study, we performed an initial biopsy of the injured skin of each patient in the pre-auricular (“non-treated”) region. The patients received a supply of tretinoin hydroalcoholic solution (tretinoin – 0.05%; propylene glycol – 5% and alcohol 50% - 20 ml) to be used every night on the face.
Patients were instructed to wash their faces at night with water and neutral soap. After washing, they were to apply five drops of the tretinoin solution over their faces without massaging. In the morning, they were instructed to wash their faces again. This procedure was to be performed once daily for one year, unless clinical signs of dermatitis (i.e., erythema or redness) appeared. If dermatitis was observed, they were instructed to interrupt the treatment and to call the researchers. To minimize bias in the study, patients were instructed not to use sunscreen but were strongly advised to avoid sun exposure and to use mechanical sun protection, such as hats and umbrellas.
To ensure adequate treatment and to check for possible complications, such as signs of dermatitis (e.g., redness or itching), patients were required to visit the hospital weekly during the two first months of treatment and bimonthly over the following ten months. After one year of treatment, a second biopsy of the injured skin was taken, from a point 1 cm below the ear lobe (“treated”) and at least 1 cm from the first biopsy scar. We chose to perform the two biopsies on the same side of each patient's face to ensure similar scar quality when comparing treated versus non-treated skin (Figure 1).
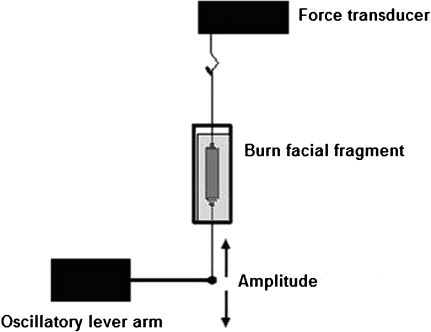
Skin strips were obtained from the biopsies (10.0×2.0×2.0 mm each) and were subjected to oscillatory mechanical analysis, and resistance (R) and elastance (E) were measured, as previously described21 (Figure 2). Briefly, the resting length (Lr) of each strip was first measured. Metal clips were glued to either end of the tissue strip with cyanoacrylate. Steel wires (0.5 mm in diameter) were attached to the clips; one end was connected to a force transducer (Model 404A; Cambridge Technologies), and the other end was connected to a servo-controlled lever arm (Model 300B; Cambridge Technologies). The lever arm was connected to a function generator (Model 3030; BK Precision, Chicago, IL), which controlled the frequency, amplitude and waveform of the oscillation. The resting force (T) was set by movement of a thumb-wheel screw system, which effected slow vertical displacements of the force transducer. Length and force signals were converted from analogue to digital and recorded in a compatible computer. The oscillation frequency was 0.1 Hz (six excursions per minute), and the amplitude was 1% Lr. Estimations of R and E were determined by applying the recursive least-squares algorithm to the equation of motion: T = EΔl+R (Δl/Δt)+K; where R = resistance, E = elastance, T = force, l = length, Δl/Δt is the change in l per unit time, and K is a constant reflecting resting force22. Resistance and elastance measurements were recorded for ten minutes.
After the mechanical oscillation, the strips were fixed in 10% formalin and embedded in paraffin for histological analysis. Next, 5-μm-thick slices were stained with Sirius red and resorcin-fuchsin to identify total collagen and elastic fibers, respectively. Type III collagen fibers and versican were stained by immunohistochemistry.23 Using image analysis software (Image-Pro® Plus 4.1 for Windows®), we determined the densities of type III collagen fibers, total collagen fibers, elastic fibers, and versican in the superficial, middle, and deep layers of the dermis. Protein density was calculated as the relationship between areas of stained protein and total tissue area and was expressed as a percentage.
The Wilcoxon test for paired non-parametric variables was used to compare the treated and non-treated areas from each of the 15 patients. The level of significance was established at p<0.05.
RESULTSAll patients completed the entire tretinoin treatment. Five patients exhibited temporary clinical signs of dermatitis (e.g., erythema, desquamation, pruritus) with spontaneous remission after a one-week interruption of tretinoin use. Because they continued with tretinoin treatment after this period, these patients were not excluded from the study. At the end of the study, three patients exhibited post-inflammatory hyperpigmentation, one exhibited mild telangiectasis on the malar region, and one had keloid development in the biopsy scar. The hyperpigmentations were later treated with 4% hydroquinone and sunscreen for three months.
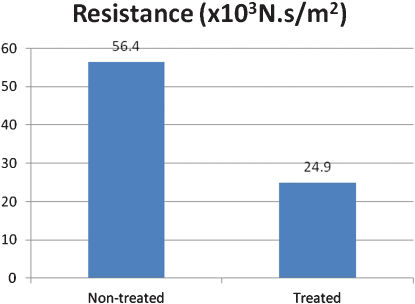
Significant decreases in the mean values of resistance (R) and elastance (E) were observed in treated scarred skin compared to the non-treated scarred skin (p = 0.003 and p = 0.047, respectively). The mean decreases in resistance and elastance after treatment were 31.4% and 14.8%, respectively (Figures 3 and 4).
There were no evident histological differences in the distributions of ECM components between treated and non-treated specimens. The quantification of total collagen, collagen III, elastic fibers, and versican content by image analysis did not reveal significant differences between treated and non-treated specimens in any of the layers of the skin dermis. Figure 5 shows representative photomicrographs of the post-burn scarred skin stained for total collagen fibers, collagen III, elastic fibers, and versican. There were also no differences in epidermal thickness, as measured pre- and post-treatment.
DISCUSSIONThere is a high demand for cutaneous treatment among burn patients. The skin is a communication organ and is vital for the perception of the limits of an organism and for the body image of an individual. Improvements in skin quality, especially in the face, can contribute to increased self-esteem and quality of life for burn patients.10,24,25
We have been using topical tretinoin to treat burn patients for more than a decade. Satisfaction is high among the patients, especially with respect to the observed improvements in tegument quality. The potential for topical treatments using tretinoin combined with glycolic acid to improve the mechanical properties of scarred skin has been indirectly shown through mouth-opening measurements.10 In this study, clinical improvements in burned skin distensibility after tretinoin topical treatment were demonstrated by a decrease in resistance and elastance, as determined by biomechanical analysis. Tissue resistance represents the energy loss resulting from the opposition to movement, and elastance (i.e., the inverse of compliance) is a measure of the tendency of tissue to recoil toward its original dimensions upon the removal of a distending or compressing force. Therefore, lower elastance (or greater compliance) corresponds to greater distensibility in a given tissue.
In this study, the mechanical properties of burned skin with and without tretinoin treatment were assessed by adapting a mechanical tissue oscillation method used for analyzing the mechanical behavior of lung tissue in various diseases.18,19 We are not aware of any other reports in the literature in which this method has been used to evaluate post-burn scarred skin. The main disadvantage of this method was the requirement for skin biopsies, which can lead to scar complications. The potential cosmetic concerns associated with biopsies were largely avoided in this protocol because the biopsies were taken from the center of existing burn scars and thus did not cause additional scarring in patients. Additionally, the biopsies were not taken from an extremely visible area.
Topical treatments with tretinoin have been shown to increase skin distensibility in post-burn scarring and acne scars with high levels of patient satisfaction.10–13,24,26,27 However, the mechanisms underlying these clinical effects are not completely understood. Retinoids, such as tretinoin, affect cell growth and differentiation and alter cell-cell cohesion. In the dermis, tretinoin modulates ECM synthesis by fibroblasts and increases angiogenesis.10,13,28,29
Scar bleaching and texture improvements achieved by topical treatments can promote secondary improvements in self-esteem and quality of life.10,30 Topical therapy with tretinoin should always include sunscreen preparations to prevent hyperpigmentation, and patients should be encouraged to avoid sun exposure.10 Because of the potential teratogenic effects of tretinoin, patients receiving this drug should use contraceptive methods.28
The most common adverse effect of topical tretinoin is local and temporary cutaneous irritation (i.e., “retinoid dermatitis”) characterized by erythema, peeling, dryness, and itching.31 This effect was observed in 20% of the patients in this study. This high incidence is probably related to the high concentration (0.05%) of tretinoin that was used in this study. These cases were treated by temporary interruption of tretinoin use, which resulted in spontaneous remission. Other adverse effects included hyperpigmentation and increased telangiectasias in 5% of patients. We currently prefer to use lower doses of tretinoin (0.025%) to minimize skin irritation.
Patients with facial burns with over two years of evolution were selected to avoid the period when the spontaneous involution of the tegument occurs because of cicatricial process maturity.6,8,9,30,32,33 ECM remodeling depends on the equilibrium between fiber synthesis and degradation. Collagen fibers are responsible for the tensile force of connective tissue, and elastic fibers return the deformed collagen network to its previously relaxed condition through traction forces. When elastic fibers are injured, there is a loss of elasticity. Additionally, maturation of post-burn scars depends on the normalization of dermal proteoglycan levels.31,34,35 Collagenase production may be favored in the cicatricial tissue with the use of tretinoin, in keeping with what is seen after the compression of hypertrophic areas.10,36
The histological analyses and the quantitative assessments of collagen, elastic fibers, and versican content performed in this study were not sensitive enough to explain the observed changes in the mechanical behavior of the post-burn skin after treatment. The results and tables with these comparisons are available in a doctoral thesis;37 however, they were not referenced here because they were not statistically significant. It is possible that the structural arrangement, distribution and/or organization of the fibers play a more relevant role in determining the mechanical behavior of the tissue than do the quantitative changes. In addition, it is possible that the mechanical experiments may have disturbed the subsequent histological analyses. In the previous studies performed in the lungs, this phenomenon was not observed, but it may be beneficial to use different skin strips for mechanical and histological analyses in future studies.
Long-term maintenance of the beneficial effects of topical tretinoin treatment can be achieved through sustained adherence to the recommended treatment regimen. This was observed in this study, as patients completely adhered to the treatment to improve their appearances.8,10
We conclude that topical treatment with tretinoin changes the mechanical behavior of the skin in patients with facial post-burn scarring, thereby improving distensibility.
The authors thank Dr. Luiz Fernando Ferraz da Silva for technical support with image analyses and Claudia Garcia (RC Farmácia Dermatológica) for manufacturing the topical products.
No potential conflict of interest was reported.
Dematte MF conceived and designed the study. Gemperli R supervised the study and was responsible for the final version of the manuscript. Salles AG conceived and designed the study, coordinated one of the groups in the institution, guided the analyses of clinical results, and helped in the preparation of the manuscript. Dolhnikoff M supervised the laboratorial data and was also responsible for the statistical analyses. Lanças T was responsible for the laboratorial measurements. Ferreira MC supervised the clinical care of the patients.