Lipomas may be defined as benign lesions of mature adipose tissue without evidence of cellular atypia.1 Lipomas are the most common soft tissue lesions1,2 and surprisingly are among the rarest bone neoplasias.1–3
Osseous lipomas have been classified according to their site of origin: either within bone (intraosseus) or on its surface (juxtacortical). Surface osseous lipomas are subdivided into parosteal and subparosteal lipomas.4 Parosteal lipomas often induce a periosteal reaction.1 The most frequently affected sites are the diaphysis5 and metaphyseal regions4 of long bones.
The parosteal type is a rare tumor accounting for 0.3% of all lipomas6, usually asymptomatic,3 and affecting mainly adults aged over 40.7 The most frequent complaints are a tumoral convexity presenting as a visible or palpable mass8 or a mild-intensity pain.
A literature review in the English language MEDLINE database revealed that 12 new cases have been described since the first detailed report of a parosteal lipoma of the femur with hyperostosis by Kenin et al9 in 1959.
The present article describes a rare case of parosteal lipoma located in the femur, with extensive hyperostosis, and reviews this entity in the English language medical literature.
CASE REPORTA 55-year-old female patient noticed an increase in the volume of her left thigh, without associated pain, approximately 8 years ago. She reported a related local trauma after a ground-level fall at the time. In 2003 she was admitted to our Service, and the clinical evaluation revealed a nonpulsatile mass in the anteromedial face of the distal two-thirds of the left thigh that had a tender consistency and regular contour adhered to the deep planes and that was painless upon diffuse palpation.
Conventional radiographs of the left thigh showed the presence of a spiculated periosteal bone formation in the anteromedial face of the distal region of the femur and an increase in the amount of soft tissue with a radiodensity characteristic of fatty tissue (radiolucent image) (Figure 1).
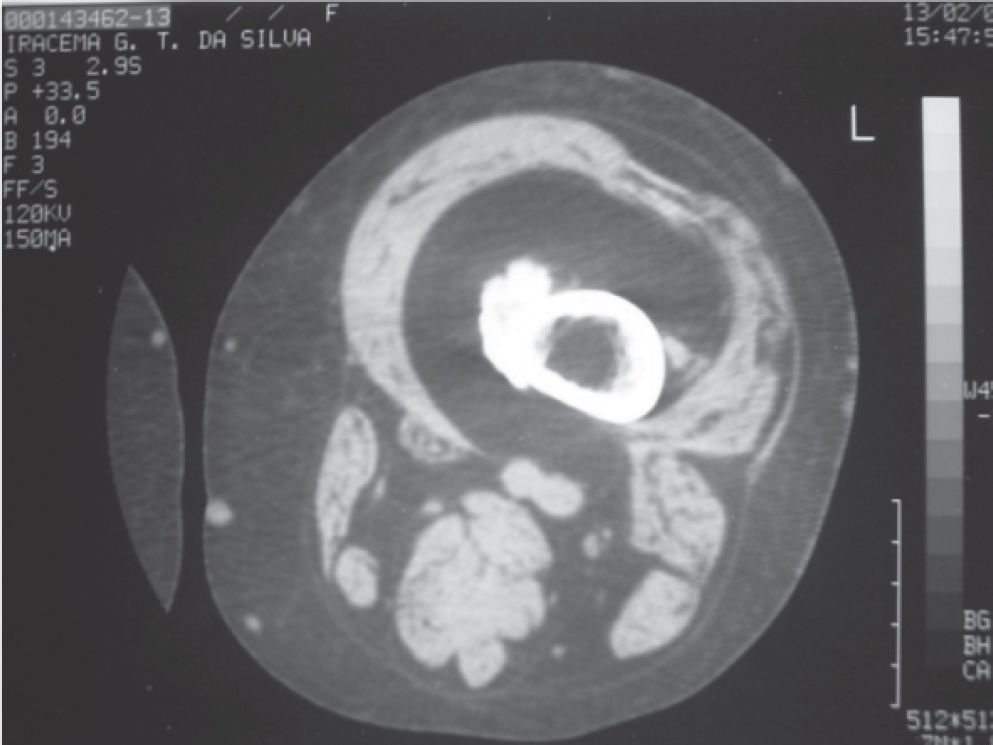
Computed tomography of the left thigh showed a heterogeneous calcification image in the periosteal topography located in the medial region of the distal third of the femur in the metadiaphyseal junction, without rupture of the cortical or bone marrow invasion. In the muscular plane, the density was similar to that of subcutaneous tissue in the intermediate vastus muscle topography, suggesting fat replacement (Figure 2).
After the evaluations were completed, only in January 2005 did the patient return to the outpatient facility with a small increase in the size of the tumor.
Due to the early differential diagnosis of the liposar-coma, abdominal ultrasonography and thoracic computed tomography were requested in order to discard the possibility of synchronic mass of the retroperitoneum or pulmonary metastatic process.
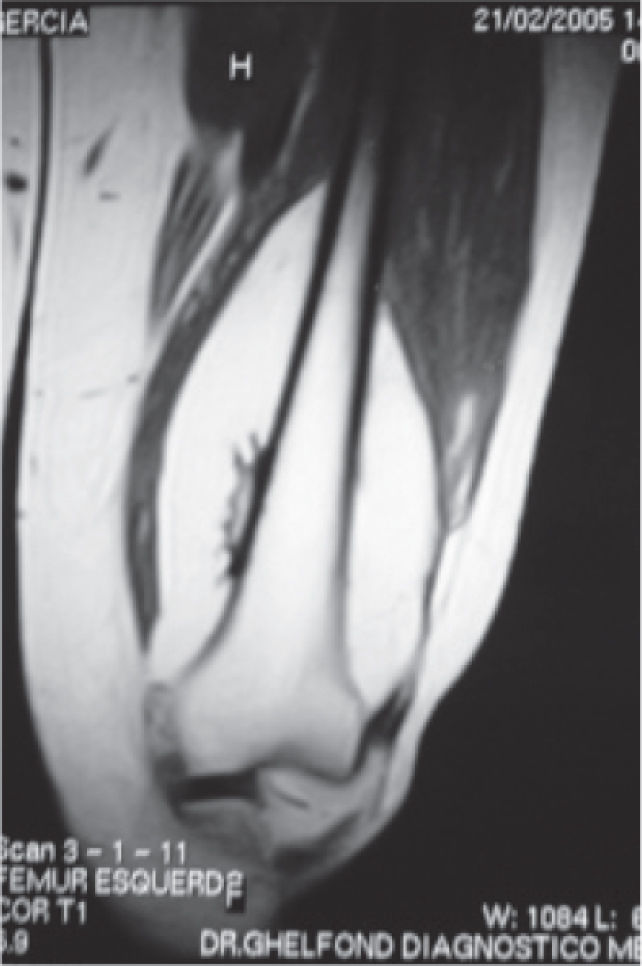
In the MRI of the left thigh, we observed an expansive process measuring 19 x 8 x 9 cm with hypersignal in T1 around the distal femur under the intermediate vastus muscle as well as hyperostosis in the metadiaphyseal region of the femur. In the T2 weighted images, as well as in the region of the hyperostosis, the tumor mass was revealed by hyposignal (Figure 3).
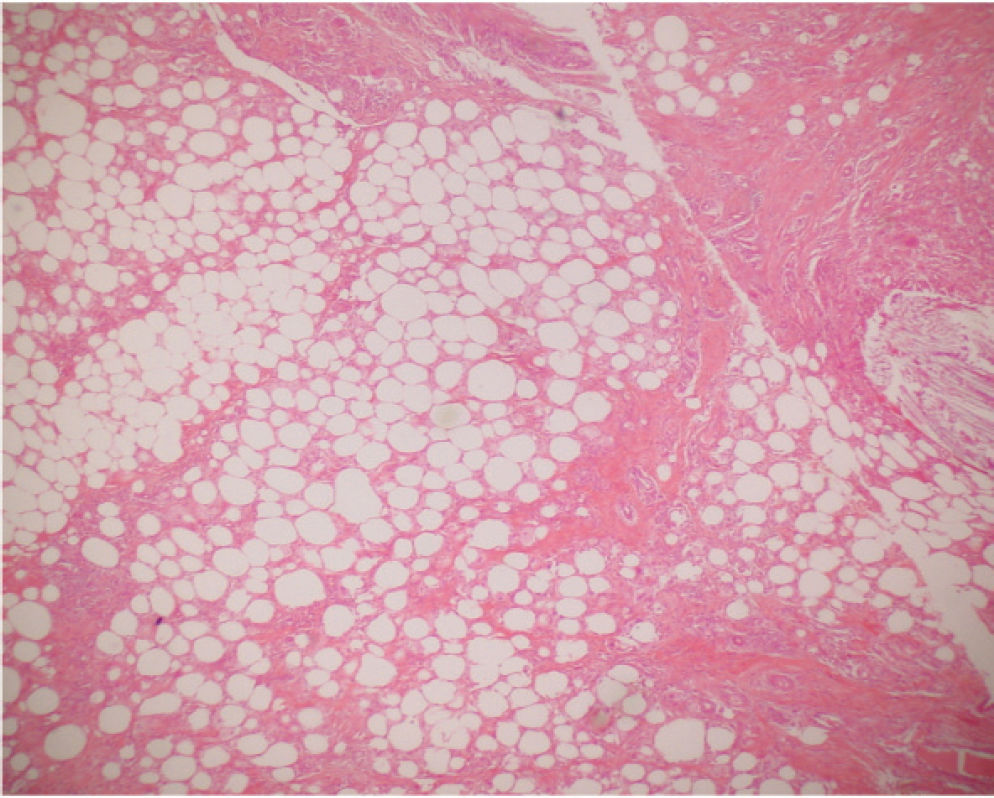
We performed an incisional biopsy of the tumor in March 2005 for anatomopathological study; it was mature adipose tissue without cellular atypia.
In the following month the patient underwent surgical intervention for tumor resection. During the surgery, it was confirmed that the lesion had adhered to the femur in the region of the hyperostosis (periosteal reaction) (Figure 4).
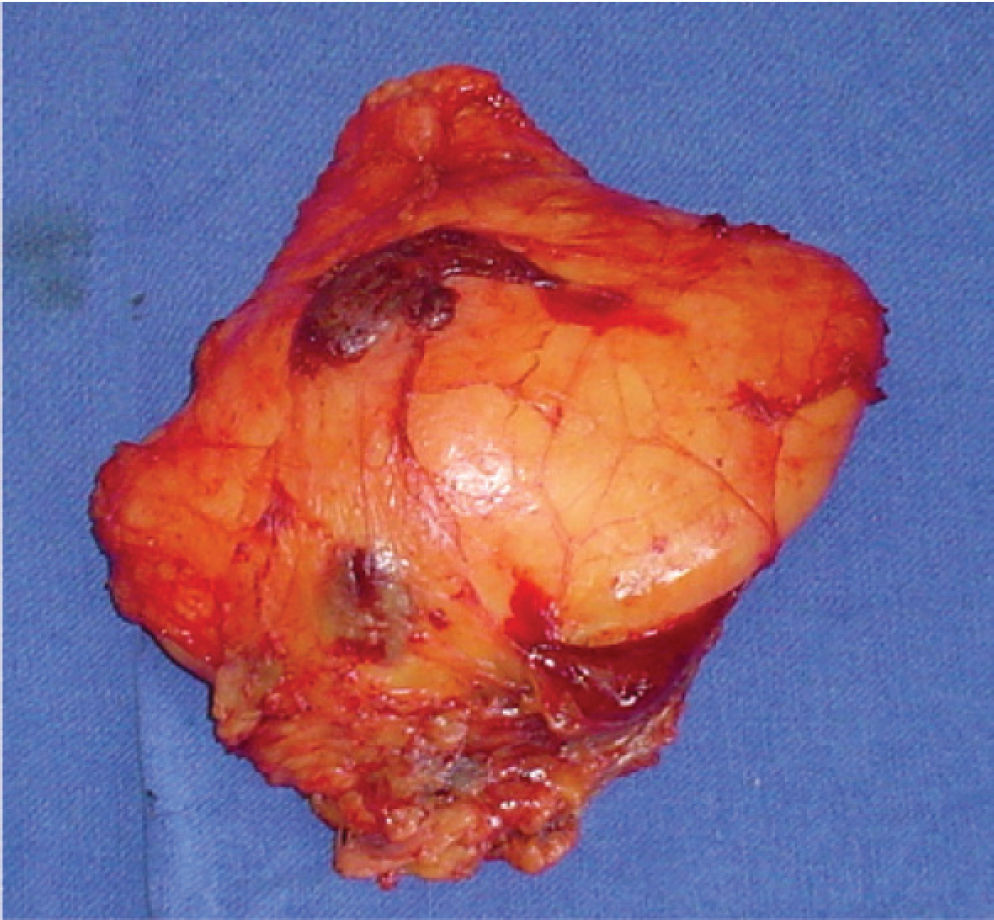
The tumor specimen weighed 437 g and had a lobulated appearance, with an intact, thin, and translucent pseudocapsule (Figure 5). Microscopic examination showed that the neoplasia was adhered to the strip of skeletal muscular tissue in its most superficial portion by fibrous tissue, with mature bone metaplasia in the deep portion with no evidence of malignancy (Figure 6). The results showed a lipoma with periosteal reaction.
There has been no recurrence during the postoperative period, and the (ambulatory) patient is periodically followed-up (for 24 months now) with no signs of recurrence.
DISCUSSIONThe World Health Organization (WHO) currently defines bone lipoma as a benign neoplasia of adipose tissue that is formed inside the medullary cavity, the cortex, or the bone surface.8
The original description of this neoplasia was published in the German medical literature by Seerig* in 1836 (as reported in Fleming et al6). The subject was approached in the English medical literature in 1866 by Smith.10 How-these rare lesions are associated with reactive changes in the adjacent bone.3,6,13 These changes include bone deformity, cortical erosion, and overproduction of the cortical bone (hyperostosis).3,6–8 More than half of parosteal lipomas presenting bone reactions are associated with hyperostosis.6
Several authors consider that cortical hyperostosis can be explained by the contact of the lipoma with the bone,3,14 being presumably caused by stimulation or irritation of the periosteum.15 However, it is not clear why some lipomas located near the periosteum cause this reaction while others do not.15
Although many cases of parosteal lipomas have been reported over the years, the data have not been appropriately described, either due to incomplete clinical history and/or reproduction of imaging evaluations, or lack of anatomopathological diagnosis in some cases.
Fleming et al6 reviewed the world literature between 1918 and 1962, having identified only 16 cases of parosteal lipoma with a well-defined radiolucent area in association with reactive bone changes; the radiological characteristics of those changes found in 11 of the 16 cases were compatible with overproduction of cortical bone (hyperostosis). Prominent hyperostosis promotes a typical appearance that, when combined the radiolucence of the soft parts of the tumor, has been described as pathognomonic for parosteal lipoma.6,15 However, the amount of cortical hyperostosis can vary from a small area of the thickened cortical to exuberant exostoses.6,13
Of the 11 cases identified in the study by Fleming et al,6 9 affected the femur, but only 2 were published in English (Tables 1A and B).
Patients with parosteal lipoma of the femur with hyperostosis (identified in literature in English language)
| Year of publication | Author | Age (years) | Sex | Duration of signals and symptoms | Body Half | Presence of pain | Imaging Technique |
|---|---|---|---|---|---|---|---|
| 1959 | Kenin et al. | 49 | Male | — | Left | No | R |
| 1960 | Fleming et al. | 52 | Female | 7 months | Right | Yes | R |
| 1982 | Rich and King | 59 | Male | 1 year | Left | Yes | R + CT |
| 1989 | Jones et al. | 32 | Male | 20 years | Right | Yes | R + CT + NMR |
| 1992 | Miller et al. | 61 | Female | — | Right | No | R + BS |
| 1993 | Goldman et al. | 53 | Female | 1 year | Right | No | R + CT + NMR |
| 1994 | Asirvatham and Linjawi | 40 | Female | — | Right | No | R + CT + NMR |
| 1994 | Rodriguez-Peralto et al. | 39 | Male | 5 years | Left | Yes | R + CT |
| 1995 | Bridge et al. | 51 | Female | 5 months | Left | Yes | R + CT + NMR* + BS* |
| 1999 | Kim et al. | 46 | Female | 7 months | Left | Yes | R + NMR |
| 2000 | Yu et al. | 37 | Male | — | Left | No | R + NMR |
| 2006 | Kapukaya et al. | 17 | Male | — | Left | Yes | R + CT + NMR |
| 2006 | Kubo et al. | 56 | Male | — | Right | Yes | R + BS + NMR |
| 2007 | Present Case | 55 | Female | 8 years | Left | No | R + CT + NMR |
R: Radiograph; CT: Computerized Tomography; BS: Bone Scintigraphy; NMR: Nuclear Magnetic Resonance.
B – Patients with parosteal lipoma of the femur with hyperostosis (identified in literature in English language)
| Year of Publication | Author | Treatment | Bone Region | Largest size of lesion (Specimen or NMR) | Recurrence | Follow-up | Anatomopathological | Hyperostosis |
|---|---|---|---|---|---|---|---|---|
| 1959 | Kenin et al. | Surgery | Diaphysis | — | No | 8 months | Yes | Exuberant |
| 1960 | Fleming et al. | Surgery | Diaphysis | 17 cm | No | 3 years | Yes | Exuberant |
| 1982 | Rich and King | Surgery | Diaphysis | — | — | — | Yes* | Small |
| 1989 | Jones et al. | Surgery | Metadiaphysis | 18 cm | — | — | Yes | Exuberant |
| 1992 | Miller et al. | Surgery | Diaphysis | — | — | — | Yes | Exuberant |
| 1993 | Goldman et al. | Surgery | Metadiaphysis | 9 cm | — | — | Yes | Exuberant |
| 1994 | Asirvatham and Linjawi | Expect | Diaphysis | — | — | — | No | Exuberant |
| 1994 | Rodriguez-Peralto et al. | Surgery | Metadiaphysis | 16.5 cm | — | — | Yes | Exuberant |
| 1995 | Bridge et al. | Surgery | Diaphysis | 10 cm | — | — | Yes* | Exuberant |
| 1999 | Kim et al. | Surgery | Diaphysis | — | — | — | Yes | Small |
| 2000 | Yu et al. | Surgery | Diaphysis | 8.5 cm | — | — | Yes | Exuberant |
| 2006 | Kapukaya et al. | Surgery | Metadiaphysis | — | — | 29 months | Yes | Exuberant |
| 2006 | Kubo et al. | Surgery | Metadiaphysis | 10 cm | No | 2 years | Yes* | Exuberant |
| 2007 | Present Case | Surgery | Metadiaphysis | 19 cm | No | 2 years | Yes | Exuberant |
Since the review by Fleming et al6 up to now, 12 new cases of parosteal lipoma of the femur with hyperostosis, including ours, have been published in English, totaling 14 in almost 90 years (Tables 1A and B). Details of these cases are listed as follows:
- •
In the 1980s, Rich and King16 described 4 cases of soft part neoplasia adjacent to the femur, presenting asymmetric cortical thickening. One of these 4 cases (Case #4) was a parosteal lipoma of the femur with a small hyperostosis (cortical thickening).
- •
Another case of these tumors was reported in English in 1989.14
- •
In spite of the 4 cases of parosteal lipoma of the femur mentioned in the study by Miller et al5 in 1992, only 1 case (Case #3) was described in detail, including clinical history, imaging, and anatomopathological evaluations.
- •
In 1993 other authors published a coincidental case of concomitant intramuscular lipoma in the left leg and a parosteal lipoma of the right femur.17
- •
In 1994 in Saudi Arabia, a large-volume parosteal lipoma with exuberant hyperostosis was found in the right thigh of a young patient; however, in spite of the characteristics, the lipoma was not surgically resected.7
- •
Also in 1994, another finding was published concerning this rare benign neoplasia in the femur, also with relevant reaction of bone.3
- •
Genetic characteristics were shown in the article by Bridge et al.18
- •
Another case was reported in 1999 by Kim et al.12
- •
Yu et al reported the eleventh case of parosteal lipoma of the femur with hyperostosis in the English language literature.19
- •
Blair and Resnick20 (2000) reported 1 case of ‘subperiosteal lipoma’ of the femur whose appearance, as stated by the authors themselves, was not that of a cortical or parosteal lipoma.
- •
Another case was published in 2006 concerning parosteal lipoma of the femur with hyperostosis.4
Recently, genetic and magnetic resonance imaging characteristics were described in another patient with this neoplasia in the femur (Case #1).21 Conventional radiographic exams showed an increase in the extra-bone soft tissues and formation of bone spicula over the periosteum. The radiodensity of the tumoral mass in conventional radiographs, which was consistent with fatty tissue, suggested the diagnosis.8,15
These case studies provide diagnostic, therapeutic, and prognostic guidance for future cases. Computed tomography and magnetic nuclear resonance help with the diagnosis13,14 and therapeutic planning. Treatment consists of resecting the lipomatous tumor15,22 with further exeresis of the bone and periosteal excrescence in cases with hyperostosis.3,4 Usually the prognosis is favorable, with no proven reports of malignancy4 or recurrence and with full recovery of the patient.