The six-minute walk test has been widely used to evaluate functional capacity and predict mortality in several populations. Thus, the aim of this study was to evaluate the prognostic value of the six-minute walk test for the life expectancy of end-stage renal disease patients.
METHODS:Patients over 18 years old who underwent hemodialysis for at least six months were included. Patients with hemodynamic instability, smoking, chronic obstructive pulmonary disease, physical incapacity and acute myocardial stroke in the preceding three months were excluded.
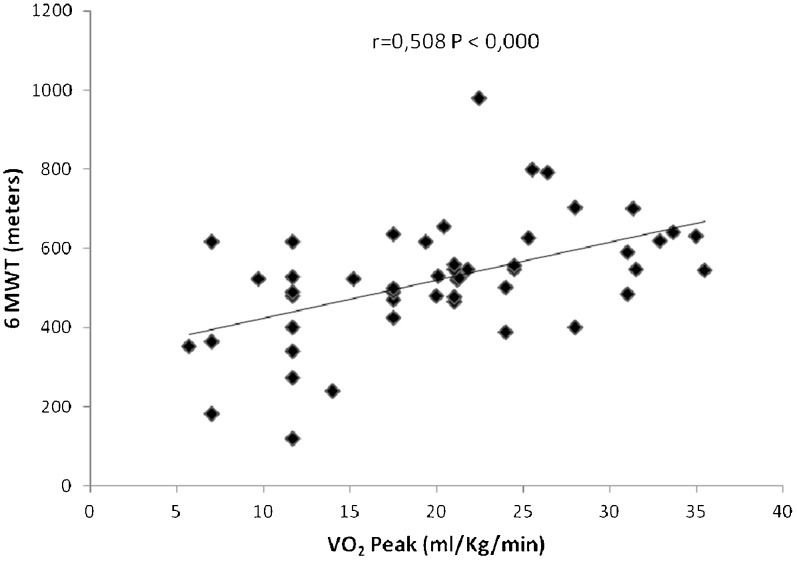
RESULTS:Fifty-two patients (54% males; 36±11 years old) were followed for 144 months. The distance walked in the six-minute walk test was a survival predictor for end-stage renal disease patients. In the multivariate analysis, for each 100 meters walked with a 100-meter increment, the hazard ratio was 0.53, with a 95% confidence interval of 0.37-0.74. There was a positive correlation between the distance walked in the six-minute walk test and peak oxygen consumption (r = 0.508). In the multivariate analysis, each year of dialysis treatment represented a 10% increase in death probability; in the severity index analysis, each point on the scale represented an 11% increase in the death risk.
CONCLUSIONS:We observed that survival increased approximately 5% for every 100 meters walked in the six-minute walk test, demonstrating that the test is a viable option for evaluating the functional capacity in patients with end-stage renal disease.
Chronic kidney disease (CKD) has become a serious health problem due to its prevalence, high cost, and the subsequent reductions in life expectancy and quality of life (1). Cardiovascular disease is the main cause of death in end-stage renal disease (ESRD) patients, as observed in the Hypertension Detection and Follow-up Program (2) and the British Regional Heart Study (3). This result is because these patients show reduced functional capacity, exercise tolerance, resistance and muscle strength compared with patients with conservatively treated CKD (4).
The peak oxygen consumption (VO2 peak) measurement, the most used parameter for evaluating functional capacity, was identified as a strong survival predictor in ESRD (3). In addition, the six-minute walk test (6MWT) has proved to be an excellent tool for functional capacity evaluation and has been widely used in patients with chronic diseases (5–9). This method has demonstrated prognostic value in pulmonary hypertension patients (10) and has been considered to be a predictor of mortality in patients with heart failure (HF) (6,11). The 6MWT is a sub-maximum effort test that is more representative of daily life activities than other effort tests (12) and has low cost and easy applicability (13,14). The distance walked in the 6MWT shows an association with the VO2 peak, making it a viable and safe alternative for patients who cannot tolerate the ergometric test (11,15,16), and may also be used as a parameter to evaluate different therapeutic interventions (17).
The 6MWT has been used to evaluate the functional capacity of CKD patients (11,18). However, its value as a mortality predictor has not yet been investigated in this population. Thus, the aim of this work was to evaluate the prognostic value of the 6MWT in ESRD patients.
MATERIALS AND METHODSResearch designThis was a prospective cohort study performed with patients selected by convenience who underwent a regular hemodialysis program between March 1996 and January 2009 at Santa Lucia Renal Clinic, Cruz Alta/Rio Grande do Sul (RS) State - Brazil. The ethical and legal aspects of the project were approved by the Ethics Committee on Research of the Institute of Cardiology of Rio Grande do Sul/University Foundation of Cardiology (n° 4286/09).
Inclusion and exclusion criteriaThe study included patients over 18 years old who were undergoing hemodialysis treatment for at least six months and optimized clinical treatment for at least three months with a complete clinical data record available from a routine database service. Subjects who had exhibited uncontrolled hypertension, recent ischemic heart disease (no more than three months ago), unstable angina, severe cardiac arrhythmias, skeletal disease limiting physical activity and several respiratory and neurological diseases were excluded from the study.
Study variablesVariables of functional capacity (distance walked in 6MWT, the ergospirometric test and the ESRD-SI) were measured at the time the subjects were admitted to the study in March and April of 1996. The 6MWT was performed during an inter-dialysis period in a 30 m long corridor that was demarcated at every meter, and the patients were assisted by a trained physiotherapist and a nurse.
The ergospirometry test was also performed in the inter-dialysis period during the same week as the 6MWT on an ergometric treadmill (Imbramed Ltd., Brazil) according to the criteria of the American Heart Association (19) and the National Consensus on Ergometry (20). The Bruce Modified Protocol (21,22) and the Ergo–PC13 system (Micromed Biotecnologia Ltd., USA) were used. The analysis of the respiratory gases was recorded via the Teem 100 (Aerosport Ind., USA) metabolic system, which evaluates oxygen consumption (VO2). Electrocardiographic effort monitoring occurred with three derivations for recording the ST follow up. At the end of each stage, blood pressure was measured with the BORG scale (23).
The ESRD-SI indicates morphologic disease and physiologic disturbance rates, measuring the impact of the process on the patient's functional and psychological capacity (24).
The patient clinical and demographic characteristics, including cardiovascular disease risk factors, hemodialysis time, transplant and death date, were semiannually updated by consulting the database service, the patients and/or family members. Mortality data were updated using patient charts, family members or information obtained from consulting public registries about patient deaths. Patient charts were reviewed by two independent investigators. Blood examinations and biochemical analyses were performed monthly at the hemodialysis unit, and their results were collected from a routine database.
Follow upPatients were followed up monthly by a hemodialysis service team and the researchers, who collected data regarding laboratory exams, clinical condition and morbidity. Transplants performed or transfers to another city were updated during the follow-up period, and they were considered as a census in the survival analysis. The patients selected for the study underwent hemodialysis regularly with three sessions per week, with each session lasting approximately four hours. Data were collected until January 2009.
Statistical analysisContinuous variables are expressed as averages and standard deviations, and categorical variables are expressed in percentages with the 95% confidence interval (CI). Student's t test and the Mann-Whitney U test were used when appropriate for continuous variables. Categorical variables were compared using the chi-square test. The Pearson correlation coefficient was used to correlate the variables. Predictor variables (ESRD-SI, 6MWT, age, dialysis time and VO2 peak) and mortality were evaluated for associations using the Cox univariate and multivariate models. Variables that were found to be statistically significant in the univariate and multivariate analyses were used for the model. Data with an alpha error of 5% (p<0.05) were considered to be significant.
RESULTSThe sample characteristics are shown in Table 1. Of 89 patients initially selected for the study, 16.8% (n = 15) were excluded due to decompensated ischemic cardiopathy, and an additional 24.7% (n = 22) were excluded because they moved to another county and/or refused to continue undergoing the periodic functional evaluations. A total of 52 patients (Figure 1) were followed up: 21 patients died, representing a survival index of 59.6%. During the 12-year follow-up period, 23.1% of the sample underwent a transplant. Systolic blood pressure was approximately 20 mmHg higher in patients who survived (p = 0.01). The use of calcium antagonists was approximately 50% higher in patients (p = 0.037) who died [RR: 2.03; 95% confidence interval (95% CI): 0.99 – 4.18]. Other biochemical and pharmacological variables did not differ between the patients who died or survived (Table 1).
Clinic and biochemical characteristics of patients stratified by life expectancy and death.
| Variables | Sample (n = 52) | Death (n = 21) | LifeExpectancy(n = 31) | p-value |
|---|---|---|---|---|
| Age (years) | 36±11 | 33.8±12 | 38±10 | 0.185 |
| Male (%) | 54 | 28.6 | 71 | 0.002* |
| BMI (kg/m2) | 22±4 | 22.4±3.4 | 22±4 | 0.518 |
| HD time (months) | 110±59.3 | 92.3±49 | 140±58.1 | 0.168 |
| Transplant (%) | 23.1 | 52.4 | 3.2 | |
| SBP (mmHg) | 157.6±26.6 | 146.2±23.2 | 165.4±29 | 0.01* |
| DBP (mmHg) | 96±19.3 | 91.7±17 | 99±20 | 0.193 |
| ESRD-SI | 7.5±5.5 | 5±4 | 9.3±6 | 0.002* |
| Urea (mg/dL) | 146.5±38 | 145.0±36.6 | 147.4±40 | 0.845 |
| Creatinine (mg/dL) | 9.4±1.3 | 9.3±1.5 | 9.4±1.3 | 0.424 |
| Calcium (mg/dL) | 8.6±1.1 | 9.1±2.5 | 9.6±4 | 0.656 |
| Phosphorus (mg/dL) | 6±2.2 | 5.4±1.7 | 6±2 | 0.282 |
| HT (%) | 26.5±5.1 | 26.1±5 | 27±5.4 | 0.435 |
| HG (g/dL) | 8.6±1 | 8.6±0.6 | 8.7±0.5 | 0.649 |
| HBsAg + (Elisa) (%) | 5.7 | 4.7 | 9.6 | 0.568 |
| HCV + (EIE) (%) | 13.4 | 4.7 | 19.3 | 0.149 |
| Digitalis (%) | 46 | 57 | 42 | 0.212 |
| Nitrates (%) | 5.7 | 0 | 9.6 | 0.155 |
| Beta-adrenergics (%) | 11.5 | 5 | 16 | 0.233 |
| Adrenergic central action (%) | 17.3 | 14.3 | 16 | 0.914 |
| Calcium antagonists (%) | 36.5 | 52.4 | 26 | 0.037* |
| 6MWT (meters) | 517.1±144 | 477.3±119 | 525±121.5 | 0.168 |
| VO2 peak (obtained) (mL/kg-1/min-1) | 20.1± 8 | 21.6±7.5 | 19.2±8 | 0.270 |
| VO2 peak (expected) (mL/kg-1/min-1) | 34.2±8# | 39±7 | 31.3±7 | 0.001* |
Values are presented as the mean±standard deviation. HD, hemodialysis; ESRD-SI, End-Stage Renal Disease Severity Index; 6MWT, six-minute walk test; BMI, body mass index; VO2 peak, peak oxygen consumption; SBP, systolic blood pressure; DBP, diastolic blood pressure; HT, hematocrit; HG, hemoglobin; HBsAg, hepatitis B surface antigen; HCV, hepatitis C antibodies; *p<0.05; #p<0.001.
Regarding the relationship between hemodialysis time and mortality, the univariate and multivariate analyses indicated a 10% increase in death risk for each year on hemodialysis, with an odds ratio (OR) of 1.01 and a 95% CI between 1.00-1.02 (Tables 2 and 3).
Cox univariate analysis stratified per 100 meters.
| Variables | OR | 95% CI HR | p-value |
|---|---|---|---|
| 6MWT | 0.79 | 0.62 – 1.01 | 0.064 |
| Age | 1.03 | 0.99 – 1.07 | 0.090 |
| ESRD-SI | 1.15 | 1.08 – 1.23 | 0.000* |
| HD time | 1.01 | 1.00 – 1.02 | 0.003* |
| VO2 peak | 0.96 | 0.91 – 1.01 | 0.122 |
OR, odds ratio; 6MWT, six-minute walk test stratified per 100 meters; ESRD-SI, End-Stage Renal Disease Severity Index; HD, hemodialysis; VO2 peak, peak oxygen consumption; CI, confidence interval; HR, hazard ratio; *p<0.05.
Cox multivariate analysis stratified by 100-meter increments.
| Variables | OR | 95% CI HR | p-value |
|---|---|---|---|
| 6MWT | 0.53 | 0.37 – 0.74 | 0.000* |
| Age | 1.28 | 1.16 – 1.41 | 0.000* |
| ESRD-SI | 1.01 | 1.00 – 1.02 | 0.001* |
| HD time | 1 | 0.94 – 1.03 | 0.651 |
| VO2 peak | 1.04 | 0.97 – 1.13 | 0.259 |
OR, odds ratio; 6MWT-100, distance walked in six-minute walk test stratified by 100 meters; ESRD-SI, End-Stage Renal Disease Severity Index; HD, hemodialysis; VO2 peak, peak oxygen consumption; CI, confidence interval; HR, hazard ratio; *p<0.05.
The End-Stage Renal Disease Severity Index (ESRD-SI) was higher in patients who survived until the end of the study (p = 0.002). In the univariate analysis, the ESRD-SI presented an OR of 1.15, with a 95% CI of 1.08-1.23 (Table 2). These results were similar to the multivariate analysis, in which a one-point increase in the score led to an 11% increase in the death risk (Table 3).
The VO2 peak was approximately 50% lower (p<0.001) than the predicted values for age and gender (Table 1). No difference was observed in the VO2 peak among patients who survived and those who died. The VO2 peak did not differ significantly (univariate and multivariate analyses) after adjusting for the confounding factors, with the OR for death equal to 1.04 (95% CI: 0.97–1.13) in the multivariate analysis (Tables 2 and 3). An association was observed between the distance walked in the 6MWT and the VO2 peak (Figure 2).
The stratification of distance walked in the 6MWT in 100-meter intervals showed that the OR for death was 0.79 (95% CI: 0.62–1.01) in the unadjusted analysis and 0.53 (95% CI: 0.37–0.74) in the adjusted analysis (Tables 2 and 3). Additionally, for every 100 meters walked, there was a correction factor of approximately 5.3%.
DISCUSSIONThe main findings in our study demonstrate that dialysis time, ESRD-SI and the distance walked in the 6MWT are independent predictors for mortality in ESRD patients. For every 100 meters walked, a protection factor of approximately 5.3% occurs in relation to life expectancy, and the 6MWT is also associated with the VO2 peak.
Our study demonstrated that the association between ESRD-SI and life expectancy increases in patients: for each point obtained in the ESRD score, there is an 11% increase in death risk. These findings elevate this scale as an independent predictor of mortality. We believe that this test is an effective measure to evaluate and predict the quality of assistance given to a patient, and it is also useful for investigating renal disease progression (25). A trend similar to the ESRD-SI was observed for dialysis time, and a 10% increase in death probability was verified for every year the patient remained under treatment.
End-stage renal disease patients show high rates of hospital admissions and mortality (11). Cardiac complications cause over 50% of deaths and induce low tolerance to exercise, which consequently compromises the performance of daily activities (26). In this population, it is important to practice physical exercise (aerobic or anaerobic) both between and during dialysis sessions because it reduces the deleterious effects of this condition (27). In part, these alterations occur due to low functional capacity resulting from uremic syndrome and a high sedentary index (3). The reduction of functional capacity evaluated by the 6MWT was observed in several studies of patients with pulmonary hypertension and HF (6,28), demonstrating the prognostic and predictive value of the 6MWT for mortality (6,11,18). Our study demonstrates that the distance walked in the 6MWT is also an independent mortality factor in end-stage renal disease patients.
The VO2 peak value and the distance walked in the 6MWT have been noted as strong independent predictors of mortality in HF (29) patients. Sietsema et al. (3), analyzing the VO2 peak and life expectancy in ESRD patients, stated that values less than 17.5 mL/kg-1/min-1 are strong mortality predictors. ESRD patients demonstrate an approximately 64% VO2 peak reduction compared with age-matched control subjects (30). These results are similar to the VO2 values obtained in our study, which were 50% below the expected values.
The gold standard for functional capacity evaluation is the VO2 peak, which is evaluated by the ergospirometric test (31). However, this method requires a trained team and specialized equipment, involves high cost and is not always tolerated by terminal renal insufficiency patients, limiting its large-scale use in this population (26,32). Our results demonstrate that the 6MWT presents a moderate correlation with the VO2 peak obtained in this evaluation. In clinical experiments carried out with HF patients (NYHA class: II and III) who were followed for a 6-month period, functional capacity, measured by the ergospirometric test, showed a moderate correlation with the distance walked in the 6MWT and the life expectancy of these patients (33). It is important to note that Gayda et al. (15), Guyatt et al. (34), and Lipkin et al. (16) suggest a strong correlation between these variables in cardiac patients. Our group previously showed a moderate correlation between the distance walked and the VO2 peak in patients with ESRD (35). However, it is also important to highlight that there are no papers in the literature establishing the prognostic value of the 6MWT in these patients.
Anemia is an important complication in ESRD patients and is associated with disease severity (36,37). In our study, all of the patients with anemia were treated in accordance with Diretrizes Brasileiras de Doença Renal Crônica (38). Moreover, the hematocrit and hemoglobin values were similar between “death” and “life expectancy”, suggesting that this variable did not influence our results.
Thus, our results suggest that the 6MWT can be recommended as a viable, low-cost, easy-to-apply and highly accurate alternative for the determination of the functional capacity of ESRD patients.
In the analysis of the distance walked during the 6MWT with 100-meter increments, our findings show that the shorter the distance walked, the greater the probability of death in terminal renal insufficiency patients. A similar result was found by Rostagno et al. (39) when evaluating a series of HF patients. Thus, performing physical activities would improve the functional capacity and, consequently, the distance walked, constituting a protection factor for these types of patients (32). Due to the great prevalence of comorbidities, any physical activity prescribed must follow the principle of specificity and account for the functional capacity of the patients to avoid adversely affecting their health status (13). Based on our study, the distance obtained in the 6MWT may be considered as a reliable alternative to elaborate community rehabilitation programs for ESRD patients and a method of evaluating the physical capacities of these patients. The latter recommendation has already been adopted for the management of patients with HF (40).
This study is potentially limited by the sample size, which was reduced due to the difficulty of adherence of the subjects to the proposed evaluations and the loss of patients during the follow-up period. Another limitation is the possibility that only a single measure of distance walked in the 6MWT may not accurately represent the real functional capacity of the individuals. However, in patients with chronic renal insufficiency, a previous study (41) showed only a 3.7% increase in the distance walked when the test was repeated after 48 h. Additionally, it was not possible to determine the cause of death of some patients because the registries presented the cause of death simply as HF, which renders it difficult to analyze the data.
In conclusion, the distance walked in the 6MWT, hemodialysis time and ESRD-SI were predictors of the life expectancy of ESRD patients. The 6MWT is an accessible tool for determining functional capacity that is reliable and easy to apply. Furthermore, it may be used as a strategy to identify the progression and aggravation of the disease and, consequently, the death risk in terminal renal insufficiency patients. Therefore, its incorporation into clinical practice and the follow up of patients with chronic nephropathy in hemodialysis programs is recommended.
AUTHOR CONTRIBUTIONSKohl LM and Signori LU designed the study, analyzed the data and wrote the paper. Plentz RDM designed the study, analyzed the data, wrote the paper and had primary responsibility for the final content. Silva AMV and Lukrafka TJ analyzed the data. Ribeiro RA analyzed the data and wrote the paper. Moreira PR wrote the paper. All the authors conducted the research, read and approved the final manuscript.
The study was financially supported in part by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
No potential conflict of interest was reported.