The aim of this study was to evaluate the treatment of patients with chronic lesions in the posterolateral corner of the knee with reconstruction of the fibular collateral ligament, popliteus tendon and popliteofibular ligament and with autografts of the biceps femoris and fascia lata.
METHOD:A total of 129 patients with injuries of the posterolateral corner of the knee that lasted for more than three weeks and were associated with the lesion of at least one of the cruciate ligaments were included. All of the patients were operated on consecutively in the same hospital between March 2004 and April 2009. Clinical evaluation using the Lyshom scale and the International Knee Documentation Committee (IKDC, item 4, assessment ligament) protocol was performed in 114 patients for whom there were complete data available.
RESULTS:There was significant improvement in the Lyshom score and improved stability according to the IKDC protocol in the pre- compared to postoperative varus stress test at 30 degrees and the posterolateral rotation test.
CONCLUSIONS:Surgical reconstruction of the posterolateral corner of the knee with biceps femoris tendon and fascia lata autografts is effective in stabilizing the posterolateral corner of the knee.
The posterolateral corner of the knee has received relatively little attention because there is no consensus regarding the exact structures that are damaged in the case of injuries in this region (1,2). The involvement of these complex structures can lead to instabilities or to a severe derangement of the joint (3–6). The treatment is controversial in the literature, and various surgical techniques have been proposed (7,8), ranging from a surgical repair in the acute phase to a complete reconstruction of injured structures. Currently, the anatomical reconstruction of the posterolateral corner of the knee is advocated (2).
Lesions of the posterolateral structures of the knee are still underdiagnosed, and they are often neglected due to the difficulty of verifying which of the multiple structures are affected and with what intensity. It is known that the loss of opportunity to treat the posterolateral corner of the knee leads to failure in the primary reconstruction of the cruciate ligaments (3–6). Previous studies (9,14) argue that the main posterolateral structures to be rebuilt are the fibular collateral ligament, the popliteus tendon and the popliteofibular ligament.
The objective of this study was to evaluate the surgical outcome of the anatomical reconstruction of the fibular collateral ligament, popliteus tendon and popliteofibular ligament with biceps femoris tendon and fascia lata autografts in patients with chronic lesions (lesions lasting more than three weeks) (15) in the posterolateral corner of the knee.
MATERIALS AND METHODSThis work is a retrospective cohort study. Between March 2004 and April 2009, 129 patients with chronic injuries of the posterolateral corner of the knee associated with at least one injury of the cruciate ligaments were consecutively admitted and operated on at Hospital Nossa Senhora do Rosário (São Paulo) by the surgery service CEMKA (Centro Médico Kawano), in conjunction with the Orthopedics and Traumatology Department of Santa Casa de Misericórdia de São Paulo (SCMSP), Pavilhão “Fernandinho Simonsen”. We defined chronic injuries as those that occurred more than three weeks before hospital admission (6). Patients were excluded if they had neurological or vascular lesions or fractures around the knee, or if they had compromised integrity of the fascia lata or the biceps femoris tendon. All patients were evaluated and operated on by the same team using the techniques described below. The study was approved by the Ethics Committee of the Faculdade de Ciências Médicas da Santa Casa de Misericórdia de São Paulo, and the patients gave written informed consent for surgical procedures in the hospital in which they were operated.
A clinical evaluation was performed with objective and subjective parameters. We used item 4 of the International Knee Documentation Committee (IKDC) as an objective parameter with which to assess ligament laxity, which was classified into four grades: normal (1 to 2 mm), close to normal (3 to 5 mm), abnormal (60 to 10 mm) and very abnormal (greater than 10 mm). Although all patients underwent Lachman, anterior and posterior drawer, varus stress and posterolateral drawer tests, the results of these tests are only demonstrated in this study in relation to the varus stress and posterolateral drawer results.
For the subjective evaluation, we used the Lysholm scale, which ranged from 0 to 100 points and ranks the results as excellent (95 to 100), good (84 to 94), regular (65 to 93) and poor (less than 64). In the medical records, the Lysholm evaluation results were only available for 114 patients.
The patients were evaluated before the surgery and again at 12 months postoperatively. After a year of postoperative follow-up, the patients were questioned with regard to their personal satisfaction in performing the activities of daily living, answering either yes or no.
Surgical techniqueUnder spinal anesthesia, each patient was subjected to a clinical evaluation to identify all of the injuries to the posterolateral corner of the knee, which were operated on by the same route. The associated lesions (or those of the anterior cruciate ligament [ACL] or posterior cruciate ligament [PCL]) were treated by arthroscopy during the same surgery.
AccessAn incision approximately 12 cm long was made on the side of the thigh, in the lower limit of the iliotibial tract projection, from the middle third of the distal femur. This incision was made with the knee flexed at 30 degrees, extending to the region between the fibular head and Gerdy's tubercle (Figure 1).
The skin and subcutaneous tissue were opened, and we initially attempted to identify and isolate the peroneal nerve (the common fibular nerve) in the path that is superior and posterior to the fibular neck. Next, we identified the iliotibial tract and biceps femoris tendon, and prepared the grafts as described below. A section of the biceps femoris tendon was removed (7-cm long and with two-thirds of its original width) while maintaining its distal insertion on the fibular head. On its free end, a 2.0-cm-long suture was made (Figure 2).
The iliotibial tract graft was removed (14 cm long and 3.0 cm wide), and its insertion into the tubercle of Gerdy was preserved. A 2.0-cm-long suture was made in its free end, and the iliotibial tract was then divided into two bands of 1.5 cm each. One of the bands remained in Gerdy's tubercle, and a 2.0-cm-long suture was made in the other using the Kawano et al. technique (16).
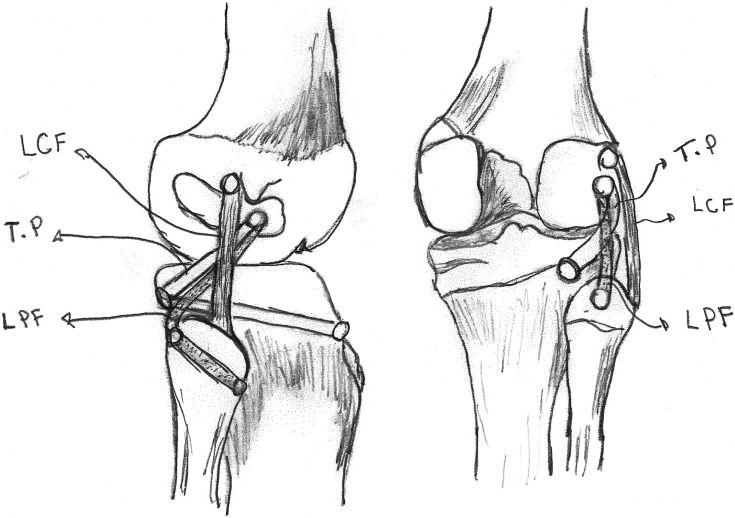
The construction of tunnels for the grafts took into account the following points of isometry (Figure 3):
- •
The fibular collateral ligament – the anterior region of the fibular head, with the posterior region of the lateral epicondyle of the femur;
- •
The popliteofibular ligament – the posterior region of the fibular head with the anterior lateral femoral epicondyle;
- •
The popliteus tendon – 1.5 cm below the intra-articular line, in the posterior cortex of the lateral tibial plateau, with the anterior region of the lateral femoral epicondyle.
The tunnels were constructed as follows (Figure 4):
Fibular collateral ligament – the femoral insertion was made 5 mm posterior and proximal to the midpoint of the lateral femoral epicondyle with a drill 7 mm in diameter and 2.5 cm in depth;
Popliteofibular ligament and popliteus tendon – the tibial insertion of the popliteus tendon was made through an anterior-posterior tunnel, 5 mm below the center point of Gerdy's tubercle, with a 7-mm drill, ending 15 mm from the intra-articular line in the posterior region of the tibia. The common femoral insertion was made 5 mm anterior and distal to the midpoint of the lateral femoral epicondyle, with a diameter of 7 mm and a depth of 2.5 cm. The fibular insertion of the popliteofibular ligament was made through an anteroposterior tunnel, with a diameter of 5 mm (Figure 5), 1 cm below the fibular styloid.
Before fixing the grafts, 25 cycles of pre-tensioning were conducted with 0 to 110 degrees of knee flexion. The graft fixation in the bone tunnels was performed with titanium interference screws with the knee in 30 degrees of flexion and internal valgus rotation. Finally, the suture was made, plane by plane.
Postoperative careThe lower limb of the patient was kept in a splint in extension for four weeks. Subsequently, the rehabilitation program began. The patient was released to passive, assisted physiotherapy, with the knee being flexed gradually from 0 to 90 degrees after four weeks of cast immobilization. After the removal of the splint, a period of four weeks of other isometric exercises was recommended, always with partial loading. After the knee was no longer immobilized, it was kept in a hinged brace for protection of the collaterals.
Eight weeks after the surgery, full loading was allowed, and the knee could be flexed beyond 90 degrees. The isometric exercises were maintained. Strength exercises were allowed (for strengthening and endurance, gradually) after 12 weeks, and running is allowed after 20 weeks. The patient was discharged nine months postoperatively.
Statistical analysisThe qualitative variables are presented in terms of absolute and relative frequencies. For the quantitative variables, summary statistics (mean and standard deviation, for example) and boxplot graphs are presented.
To compare the total Lysholm scores between the two evaluation times, the paired Student's t test was used. The comparison of the ligament evaluations (IKDC item 4) between the pre- and post-surgery times is demonstrated by descriptive tables.
The level of significance was set at 5%.
RESULTSOf the 129 patients operated on and included in the study, 94.6% were male (122 patients). The right side was affected in 58.9% of the patients (76 patients). The patients' ages ranged from 16 to 55 years, with a mean age of 30 years and 11 months. The causes of injury were major motor vehicle accidents in 54 cases, 52 of which involved motorcycle accidents. Sports were the cause of injury in 54 patients (soccer in 52 cases). The other 21 patients were injured in other accidents. The time between injury and surgery ranged from 2 to 156 months, with a mean time of 26 months and 27 days, a median of 18 days and a standard deviation (SD) of 27.27 days.
The chronic lesions of the posterolateral corner of the knee were always associated with at least one lesion of the cruciate ligaments and were distributed as follows: lesions of the anterior cruciate ligament (ACL) in 66 cases, lesions of the posterior cruciate ligament (PCL) in 35 cases and lesions of both the ACL and PCL in 22 cases; ACL lesions and varism in four cases, PCL lesions and varism in one case, and lesions of both the ACL and PCL plus varism in one other patient.
Of the 129 treated patients, Lysholm questionnaire results were available for 114 patients at the postoperative evaluation and were significantly different from the preoperative evaluation results (p<0.001), as shown in Table 1.
The results of the ligament evaluation (Tables 2 and 3), which compared the degree of instability between the pre- and postoperative periods for each type of lesion separately, were also obtained in 114 patients.
Regarding personal satisfaction, 92% of the patients reported having returned to activities similar to those in which they engaged before the injury with regard to sports, work and daily activities.
DISCUSSIONInjuries in the posterolateral corner of the knee are uncommon and often occur in association with other ligament injuries, particularly those to at least one of the cruciate ligaments (2,8,17). In our study, there were no isolated lesions of the posterolateral corner of the knee.
The correct diagnosis of the structures involved in posterolateral injury is important because this type of lesion causes great instability, with disastrous consequences to the cartilage of the knee, if not diagnosed. These lesions also cause failure in primary ACL reconstructions (3,5,6,18).
LaPrade et al. (14), in an anatomical study performed on cadavers, identified the main structures in the posterolateral corner of the knee as the fibular collateral ligament, the popliteus tendon and the popliteofibular ligament. We agree with these authors that these structures are the main anatomical components of this region and that, therefore, any surgical technique should include their reconstruction. The importance of these structures in resisting excessive forces in varus and external rotation of the tibia was indeed demonstrated by several authors (19–21) in biomechanical studies in which resistance tests were performed with a section of each structure. However, these studies did not show how these structures should be reconstructed.
The fibular collateral ligament is an important stabilizer in varus opening, and it functions in the secondary restraint of posterolateral tibial rotation at up to 30 degrees of knee flexion. However, at close to 70 degrees of flexion, this ligament becomes more vertical in the sagittal plane, which makes it difficult to resist the forces of external rotation. This resistance is the function of the popliteofibular ligament, as the tension in this ligament increases along with the flexion of the knee (22). The popliteofibular ligament is suggested to be the dominant structure when the knee is flexed and therefore should always be reconstructed (22).
Biomechanical studies have determined the maximum amount of force that the fibular collateral ligament, popliteus tendon and popliteofibular ligament can withstand. Maynard et al. (23) demonstrated that the popliteofibular ligament and the fibular collateral ligament cannot resist forces greater than 424 and 746 N, respectively. These authors proposed that the popliteofibular ligament could be reconstructed from the femur to the fibula.
In their studies, LaPrade et al. (19) found the following cut-off forces for the failure of the ligaments and tendon: 295 N for the collateral ligament, 298 N for the popliteofibular ligament, and 700 N for the popliteus tendon. The differences are likely due to the limitations of studies with cadavers, in which there is a lack of homogeneity regarding gender, age and means of preservation.
We used a 30-mm-wide section of the iliotibial tract, which is divided into two bands. One band is used as a graft to reconstruct the popliteus tendon (according to LaPrade et al. (19), this tendon fails when subjected to a 700-N force), and the other band is used to reconstruct the popliteofibular ligament (which fails when subjected to a 298-N force) (19). Each iliotibial tract band is 15 mm wide; according to Noyes et al. (4), an iliotibial tract width greater than 16 mm leads to failure when subjected to forces greater than 628 N.
Precise isometric point positioning has already been determined to be essential in ACL reconstruction (24). Camanho (25) believes that the concept of isometry could improve the principles of reconstruction of the posterolateral corner of the knee. There is isometry between the head of the fibula and the lateral epicondyle of the femur. The posterior aspect of the fibular head is isometric to the anterior aspect of the lateral epicondyle of the femur, and the anterior aspect of the fibular head is isometric to the posterior aspect of the lateral femoral epicondyle (26).
Sigward et al. (27) determined the ideal isometric location for the grafts of the fibular collateral ligament, popliteus tendon and popliteofibular ligament in the lateral femoral condyle using the foot-print of the fibular collateral ligament and popliteus tendon, in accordance with the studies of Fanelli and Larson (26). We therefore believe that the anatomical reconstruction agrees with the concepts of isometry, and together, these ideas can provide the best results in reconstructions of the posterolateral corner of the knee.
The treatment of injuries in the posterolateral corner of the knee has generated much controversy, especially in the past. Most authors agree that the surgical treatment should be performed during the acute phase of the disease, up to three weeks after the trauma that caused the injury (7,8), and should be aimed at repairing the damaged posterolateral structures. Several recent studies (28,29) also indicate that the results of surgical reconstruction in the acute phase of injury are better. This consensus is likely due to the difficulty in identifying the precise injury sites as time passes, as there is swelling and bruising during the acute phase of injury that may confuse the surgeons at the time of the repair of the lesions.
Posterolateral corner injuries are typically associated with other ligament injuries, and there is a general consensus in the literature that the best surgical results are obtained when all ligament injuries are corrected during the same surgery (5,15), which we also affirm. Accordingly, all of our patients had their lesions reconstructed during the same surgery. In our study, we found that 100% of the injuries to the posterolateral corner were associated with other ligament injuries.
There is no consensus in the literature regarding the best surgical technique. In cases of structural carus, there is consensus that a high tibial osteotomy should be performed as an initial procedure to prevent excessive loads on the posterolateral structures that were rebuilt (2,15,28,30,31). We also agree with this consensus, and in our study, the patients who had structural varus (4.6% of patients) underwent high tibial osteotomy in the same surgical procedure during which the posterolateral structures were rebuilt; thus, we obtained good results.
LaPrade et al. (11) proposed an anatomical reconstruction technique based on a biomechanical study in vitro, in which they rebuild the three main structures of the posterolateral corner of the knee (fibular collateral ligament, popliteus tendon and popliteofibular ligament). The authors reconstruct the popliteofibular ligament from the tibia to the fibula. LaPrade et al. (32) demonstrated the results of this technique with allografts of the Achilles tendon in a series of cases, and they concluded that the technique has increased the stability in patients with chronic injuries of the posterolateral corner. We also reconstructed the three main structures, but in our study, we reconstructed the popliteofibular ligament from the femur to the fibula and not from the tibia to the fibula as did LaPrade (11,32). Moreover, our results demonstrated improved stability of the posterolateral corner with 12 months of follow-up.
Jakobsen et al. (13) proposed a technique for the anatomical reconstruction of the posterolateral corner of the knee with the use of autografts of the semitendinosus and gracilis tendons. Their study was conducted in patients with isolated injuries of the posterolateral corner of the knee. The authors recreated the fibular collateral ligament, popliteus tendon and popliteofibular ligament. They used transtibial and transfibular tunnels with good results. In contrast, in our study, all of the patients had lesions associated with at least one of the cruciate ligament injuries, and the results achieved were excellent.
Patients with instability in more than one plane have a highly dysfunctional knee. They cannot play sports, and many experience difficulty in performing daily activities (33). This scenario is exactly what we found in our study, but our results were very encouraging, and we have provided to 92% of the patients the state of functionality they had before the injury.
There is no consensus in academia regarding how to perform the anatomical reconstruction of the posterolateral corner of the knee. There are disagreements over the use of autografts versus allografts, as well as over whether the popliteofibular ligament should pass from the femur to the fibula (11,32,34) or from the tibia to the fibula. We believe that the popliteofibular ligament has to proceed from the femur to the fibula, but only with additional biomechanical and surgical results, with long-term follow-ups, will we be able to reach a conclusion regarding which of these methods is the best surgical technique.
In the technique we use (34), the anatomical reconstruction of the posterolateral corner of the knee recreates the fibular collateral ligament, popliteus tendon, and popliteofibular ligament. The isometric, biomechanical and anatomical descriptions of previous studies (9,14,23,25,35,36) are used as references for the reconstruction of the three main posterolateral structures. The results were very good in general, as demonstrated by the Lysholm score and item 4 of the IKDC.
Because this study contains only complex lesions associated with at least one injury to the cruciate ligaments, and because autografts of the semitendinosus and gracilis tendons were used, we had no other option but to use the biceps femoris tendon and fascia lata in the reconstruction of the damaged posterolateral structures. However, allografts are not as easily accessible in our country, and when that option becomes widespread, we believe that this same technique will be performed with allografts, resulting in less morbidity.
The reconstruction of the posterolateral corner of the knee using the biceps femoris tendon and fascia lata was shown to be effective in stabilizing the posterolateral corner of the knee.
AUTHOR CONTRIBUTIONSOliveira MG participated in the study design, data collection, manuscript writing, and final revision. Severino NR participated in the study design, critical revision of the manuscript, and revision of the final version. Kawano CT participated in the data collection, data interpretation and final revision of the text.
No potential conflict of interest was reported.