Thrombotic thrombocytopenic purpura (TTP) is a rare hematologic syndrome. It is a multisystem disorder characterized by microangiopathic hemolytic anemia and thrombocytopenia and may be accompanied by fever and renal or neurologic abnormalities (1,2). Most adult patients acquire (3) the disease as a result of autoantibodies against ADAMTS13 (i.e., idiopathic TTP), or it is observed in association with collagen vascular disease, bone marrow transplantation, systemic sclerosis, infections, polymyositis, pregnancy, or drug treatment, including cyclosporine, tacrolimus, ticlopidine, and antineoplastic agents (i.e., non-idiopathic TTP) (1,4). However, TTP associated with mitral valve replacement surgery has not been reported. In this paper, we describe a case of a 41-year-old female who developed acute TTP after mitral valve replacement surgery. The patient was treated with plasma exchange (PE) and recovered following an uneventful course.
CASE DESCRIPTIONA 41-year-old woman with a four-year history of shortness of breath and chest tightness was admitted to our hospital for evaluation. Echocardiography revealed mitral valve stenosis (mitral valve area 1.06 cm2) as a result of rheumatic heart disease. The patient underwent mitral valve replacement via a right atriotomy with a mechanical mitral valve (tissue annulus diameter of 27 mm; St. Jude Medical, St. Paul, Minnesota USA). Cardiopulmonary bypass lasted for 115 minutes, and the aortic clamp time was 43 minutes. Postoperative echocardiography revealed satisfactory valve function and confirmed the successful removal of the intracavitary lesion.
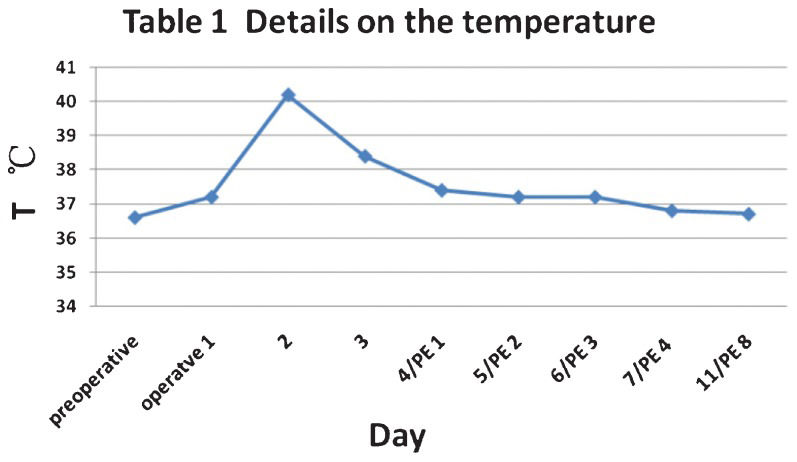
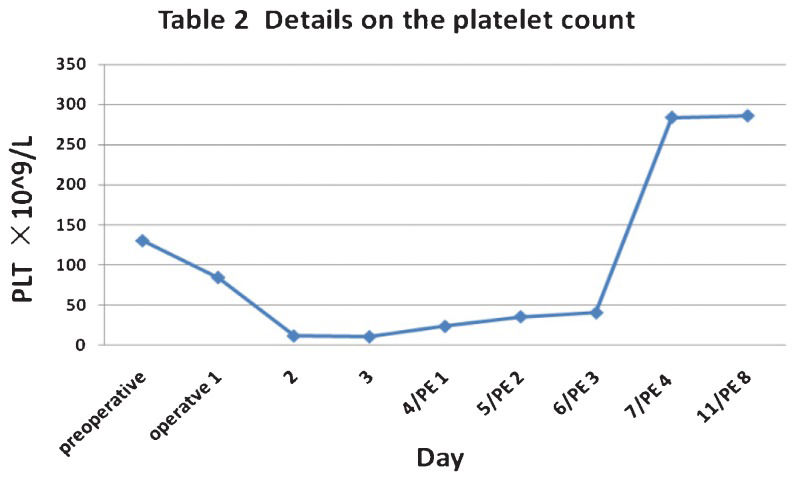
Cefoxitin (3 g/day) was initiated on postoperative day 1 for prophylaxis. A complete blood count (CBC) was obtained daily and revealed a low platelet count (Table 2) on day 2. Platelets (400 ml) were transfused, but the patient developed fever (Table 1), and the platelet count dropped continuously (Table 2). In addition, the patient developed neurological symptoms and subcutaneous ecchymosis. A blood biochemical analysis revealed a serum lactate dehydrogenase of 821 U/L and 7.7 μmol/L total bilirubin (direct bilirubin, 2.1 μmol/L; indirect bilirubin, 5.6 μmol/L). Her urine exam was positive for protein (3+), leukocytes (normal), hemoglobin (2+), and bilirubin (1+). A direct Coombs test was negative, and PT and aPTT were within the normal range. Liver and renal function tests were normal. Physical examinations of the cardiovascular and respiratory systems and abdomen were normal. Abdominal ultrasonography, computed tomography, and magnetic resonance imaging of the brain revealed no abnormalities. The patient was diagnosed with acquired TTP and received a bolus of dexamethasone (10 mg), an infusion of a high volume of fresh frozen plasma, and a red blood cell transfusion. However, the patient did not respond adequately. Until eight hours after one-volume (2000 ml fresh frozen plasma) PE was treated, the patient’s body temperature began to normalize, and her neurologic and respiratory parameters improved. The patient was discharged after an additional eight days of hospitalization without plasma exchange.
DISCUSSIONTTP is a rare hematologic emergency with an abrupt onset, and it is potentially fatal. It is clinically characterized by five typical symptoms: hemolytic anemia, thrombocytopenia, renal impairment, fever, and neurological disorders. Although TTP is associated with a severe deficiency of ADAMTS13 activity (5), measurements of ADAMTS13 activity are not required to conclusively confirm the diagnosis (6). Therefore, the diagnosis of TTP is based on the presenting clinical features (1). As in this case, there is typically insufficient time to evaluate ADAMTS13 activity, and a prompt diagnosis of TTP is critical for initiating treatment and reducing patient mortality.
Mitral valve replacement is one of the best treatments for mitral stenosis. It has been performed successfully with excellent results and limited complications. The major complications of mitral valve replacement surgery include postoperative bleeding, ischemic stroke, myocardial infarction and death. This is the first case report of TTP as a complication of mitral valve replacement surgery. Although ADAMTS13 activity was not measured in our case, the clinical course was not affected by PC transfusion, and the rapid response to plasma exchange supports the TTP diagnosis. We will follow up this case and evaluate plasma ADAMTS13 activity and autoantibodies to exclude the possibility of hereditary ADAMTS13 deficiency, which is extremely rare, or acquired autoantibodies against ADAMTS13, which often persist despite clinical resolution or remission (7).
Daily plasma exchange remains the mainstay of treatment for acquired TTP regardless of its etiology (1). However, plasma infusion once every two weeks appears to be sufficient for hereditary TTP (8). Our patient recovered with one plasma volume and showed a good clinical outcome, with a normal temperature and improvement of neurological and respiratory parameters eight hours later. The course over the next eight days of hospitalization was uneventful and did not require a second plasma exchange.
Although the occurrence of TTP associated with mitral valve replacement surgery is extremely rare, it is important to recognize TTP as a cause of thrombocytopenia and hemolytic anemia in any patient with mitral valve replacement surgery. The prompt initiation of treatment with plasma exchange remains the cornerstone of TTP treatment. Despite the prognosis of TTP associated with mitral valve replacement surgery, the schedule for PE remains poor, and further studies are necessary to improve the management of this disease.
The authors thank X. Long Zheng at The Children’s Hospital of Philadelphia and University of Pennsylvania for his careful revision of the manuscript.
No potential conflict of interest was reported.
Zhu J and Xi EP wrote the manuscript first draft. Zhu SB, Liu Y, Jiang W and Xia F contributed to the patient treatment and took part in the care of the patient. Liu Y participated in data collection and analysis. Zhu J conceived the study and performed the literature search. Xi EP revised the manuscript. Zhu SB was the first surgeon who provided clinical expertise, reviewed the manuscript and approved the manuscript final version.