To present nine patients with ankylosis in their knees that were submitted to a total arthroplasty to lessen their pain and improve their functional limitation. For these patients, arthrodesis remained a possibility in the event of arthroplasty failure.
INTRODUCTIONAnkylosis of the knee is a severe functional limitation that becomes worse when pain is present. Arthrodesis of the knee is a classical indication for such patients, since it resolves the pain; however, the severe functional limitation remains.
METHODSIn the present study, we evaluated the clinical course of nine patients who underwent total arthroplasty of the knee, and were followed up for at least five years.
RESULTSThe results demonstrate that all of the patients experienced a significant reduction in pain and some improvement in the degree of knee flexion and extension.
CONCLUSIONBased on the latest follow-up, there has been no need to perform arthrodesis for any of our patients, showing that a total arthroplasty could be a option for treatment in knee ankylosis.
Total arthroplasty of the knee is one of the biggest advances in reconstructive surgery. It is classically indicated in cases of degenerative processes and sequelae of inflammatory diseases, and has been greatly developed in orthopedic practice.
The indications, which initially presented only functional limitations, are becoming increasingly broadened as a result of the availability of prosthetic materials of better quality and the growing familiarization of medical teams with the tools used.
Consistent with this trend, we started carrying out total arthroplasty for a few patients with painful ankylosis of the knee several years ago. These patients were also presented with the alternative of arthrodesis of the knee as a therapeutic procedure that could reduce the pain, but not the severe functional limitation.
A select group of patients was presented with the therapeutic option of total arthroplasty of the knee to reestablish movement and significantly reduce pain, followed with arthrodesis in the event of arthroplasty failure. Some of the patients accepted the challenge and, in the present study, we report the clinical course of the first nine of these cases who have now been followed up for at least five years.
MATERIALS AND METHODSOver a minimum period of five years, we studied the clinical course of nine patients with ankylosis in their knees who underwent total arthroplasty for treatment. At their initial assessment, these nine patients presented pain and joint limitation that allowed less than five degrees of movement.
The patients’ characteristics and the initial diagnoses are reported in table 1.
Description of the cases, with initials of the names, sex, age in years, side affected, and initial diagnosis
| Name | Sex | Age | Side | Initial diagnosis |
|---|---|---|---|---|
| JBF | M | 41 | R | Sequela of fracture |
| MFS | M | 32 | R | Sequela of fracture |
| LJBR | M | 36 | L | PO infection |
| MGM | F | 42 | L | PO infection |
| LFG | M | 43 | R | Sequela of fracture |
| GMA | M | 41 | L | PO infection |
| MFS | F | 39 | R | Sequela of fracture |
| JNN | F | 41 | R | Sympathetic dystrophy |
| EHN | M | 36 | R | Sequela of fracture |
Legend: R = right; L = left; PO = postoperative.
All patients with sequelae from fractures had suffered joint fractures that had been treated surgically. They had all undergone at least two operations to improve their range of motion, without success.
Three patients had experienced postoperative infections: two following surgery for ligament repair and one following surgery to realign the extensor apparatus. These three patients with previous infection were declared as surgically fit for total arthroplasty after assessment by an infectologist based on C-reactive protein assays and scintigraphy with radiolabeled leukocytes.
The only case of reflex sympathetic dystrophy occurred following arthroscopy to treat “chondromalacia patellar”. This patient had undergone nine surgical attempts to improve her range of motion without success.
Six patients presented with permanent deformities and ankylosis, which they had been experiencing for 4.8 years, on average.
Table 2 describes the deformities observed at the time of preoperative assessment, the clinical course (duration) of the ankylosis, and the assessment system score used by the Hospital for Special Surgery (HSS)1, taking into account the preoperative functional score obtained for the knee.
Description of the deformity, clinical course (duration) of ankylosis, and assessment score of the Hospital for Special Surgery (HSS) at the preoperative assessment
| Name | Sex | Age | Side | Deformity | Duration | HSS |
|---|---|---|---|---|---|---|
| JBF | M | 41 | R | Flexion 10 degrees | 8 years | 53 |
| MFS | M | 32 | R | Flexion 5 degrees | 4 years | 56 |
| LJBR | M | 36 | L | Flexion 10 degrees | 4 years | 53 |
| MGM | F | 42 | L | None | 4 years | 61 |
| LFG | M | 43 | R | Flexion 5 degrees | 5 years | 57 |
| GMA | M | 41 | L | None | 4 years | 59 |
| MFS | F | 39 | R | Flexion 5 degrees | 6 years | 55 |
| JNN | F | 41 | R | None | 3 years | 56 |
| EHN | M | 36 | R | Flexion 10 degrees | 4 years | 53 |
The patients were informed that there would be two possibilities for treating their ankylosis:
- arthrodesis of the knee
- total arthroplasty, with the risk of short durability and the need for arthrodesis in the event of arthroplasty failure.
The nine patients signed a consent statement to undergo total arthroplasty.
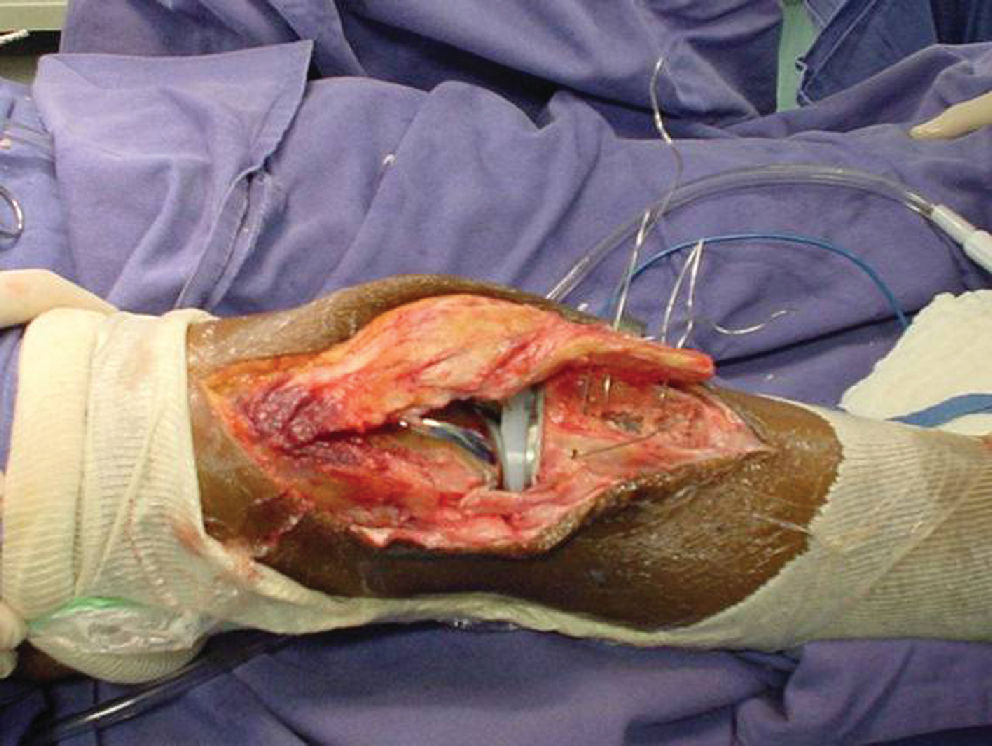
In all cases, the access route consisted of detachment of the anterior tuberosity of the tibia with bone fragments, followed by osteotomy (Figure 1).
After detaching and pushing back all of the extensor apparatus proximally, the joint was approached and the ankylosis was released. In all cases, we were able to identify the level of the joint interline.
With the knee flexed at 90 degrees, the first cut was made in the tibia, using an intramedullary guide. The level of the proximal cut was limited to a line perpendicular to the axis of the tibia, at the level of the proximal epiphysis of the fibula.
After resecting the tibial fragment, we approached the femur using an intramedullary guide and a resection level close to the bi-epicondyle line. We then carried out the resections needed to fit the femoral specimen in place.
After the cuts were prepared, we introduced the tibial and femoral specimens and performed flexion-extension with the test pieces made of polyethylene. We considered the thickness of the polyethylene to be good when flexion-extension occurred without any pressure.
We attached the anterior tuberosity of the tibia using three or four wire loops, with the knee flexed at 60 degrees (Figure 2).
In all cases, we used primary prostheses without posterior stabilization, and without patella replacement (Figure 3).
During the postoperative treatment, no continuous movement equipment was used for any of the cases. Physiotherapy was performed by a physiotherapist from the third postoperative day onwards. Strengthening and stretching of the leg musculature were performed, the joint was mobilized to gain range of motion, and cryotherapy was applied for pain relief and to control the inflammatory process.
The patients were followed up by means of weekly visits, during which radiography and functional assessments were carried out.
RESULTSSix of our nine patients were male. The mean age was 36 years, and the right side was more affected than the left (six of the nine patients).
All nine patients presented significant reductions in pain following the surgery, such that five reported only mild or occasional pain, and four described moderate pain upon exertion.
Table 3 summarizes the results, including the current degree of deformity, the degree of movement obtained after a minimum of five years of follow-up, and the HSS assessment (1). The cases that presented complications (Comp) are indicated with an asterisk.
Results of total arthroplasty in patients with ankylosis of the knee after follow-up for at least five years and taking into account current deformity, current degree of movement, HSS assessment, and complications (Comp*)
| Name | Sex | Age | Side | Deformity | Movement | HSS | Comp |
|---|---|---|---|---|---|---|---|
| JBF | M | 41 | R | None | 0–90° | 87 | |
| MFS | M | 32 | R | Flexion 5 degrees | 5–50° | 78 | * |
| LJBR | M | 36 | L | None | 0–70° | 81 | * |
| MGM | F | 42 | L | None | 0–70° | 84 | |
| LFG | M | 43 | R | Flexion 5 degrees | 5–50° | 81 | |
| GMA | M | 41 | L | None | 0–80° | 86 | |
| MFS | F | 39 | R | Flexion 5 degrees | 5–60° | 79 | |
| JNN | F | 41 | R | None | 0–70° | 82 | |
| EHN | M | 36 | R | Flexion 5 degrees | 5–50° | 78 |
The complications indicated with an asterisk were two cases of late infection. In the first case, the ankylosis was a sequela of a fracture without prior infection and, in the second case, the patient had experienced an infection following ligament repair of the knee. Both of these cases of infection occurred during the second year of follow-up. The first case required surgical cleaning, placement of a spacer for six weeks and subsequent replacement with a revision prosthesis, and the use of a flap from the medial gastrocnemius. This patient has now been followed for six years following the revision, and no new symptoms resulting from the infection have been presented.
In the second case, surgical cleaning was performed with the use of a spacer for eight weeks, followed by revision prosthesis. This patient has now undergone five years of follow-up following the revision and is well, without any symptoms of infection.
DISCUSSIONAnkylosis of the knee is a severe incapacity that causes significant functional limitation, especially when associated with pain. Using total arthroplasty for this group of patients, we sought to reduce the pain and simultaneously improve their knee movement.
In our sample of young patients, the severe limitation was reflected in their low HSS scores.1 We believe that their young ages were not contraindications, because of the severity of their limitation.
Other authors who have described their experiences in dealing with severe joint limitations have also carried out arthroplasty in young patients. Schurman et al.2 described arthroplasty of an ankylosed knee in the case of a 24-year-old patient. Given the young age of these patients and the possible need for future revision, we sought to perform arthroplasty in the least aggressive manner possible. For this, we used prostheses without posterior stabilization, and we did not replace the patella, since there was less bone resection.
Aglietti et al.3 described their experience in treating knees with severe joint limitations using prostheses with posterior stabilization. We believe that, although the bone resection and consequent ligament resection are extensive in cases of ankylosis, the anteroposterior stability in this group of patients is less important, due to the limitation of movement that consistently remains.
Postoperative rehabilitation was carried out by a physiotherapist. We did not use continuous movement equipment, since we judged that it was not necessary to detect any adherence or movement restriction within the first 72 hours”, since we judged that it was necessary to detect any adherence or movement restriction within the first 72 hours. If any limitations were present, the intensity of the manipulation could have been immediately increased. Manipulation of postoperative joint limitations should be performed as early as possible, as suggested by Yercan et al.4
Improved movement was observed in all of our patients, although a limitation of five degrees of extension occurred in four patients, and the mean flexion gain was 65°. Naranja et al.5 described a mean flexion gain of 62° in a multicenter study. Rajgopal et al.6 reported a mean flexion gain of 61° in 84 knees of 54 patients who presented severe joint limitation.
A significant reduction in pain was observed in all our patients, in addition to gains in movement. However, we were unable to reestablish normality for any of the cases.
From a two-year follow-up of a series of nine cases similar to ours, Bradley et al.7 considered their results to be satisfactory with regard to reductions in pain and partial gains in movement.
Rajgopal et al.6 presented a series of 84 knees among 53 patients with severe joint limitation. After a mean follow-up of nine years, they considered their results to be good because their patients experienced reduced pain and improved quality of life.
In the present study, two serious complications that required extensive revision occurred. Both were due to infections, and one of our patients developed ankylosis as a consequence of infection.
Kim et al.8 performed arthroplasty in 16 patients with ankylosis of the knee following pyogenic infection or tuberculosis. In most of those cases, the results were satisfactory, with postoperative infection occurring in just two cases.
In a multicenter study of 35 patients who underwent total arthroplasty of their ankylosed knees, Naranja et al.5 reported an early complication frequency of 24% and a major complication frequency of 35%. The frequency of infection was 14% in their group of patients.
There is no doubt that arthroplasty of ankylosed knees is a risky procedure, and this limitation must be clearly laid out for potential patients. Nevertheless, the possibility of gains in movement and significant reductions in pain may compensate for the risks.
The evident shortcoming of the present study is our small number of cases, which precluded the ability to obtain definitive conclusions.
In the event of complete failure in the attempt to perform arthroplasty, we would have performed arthrodesis, the only procedural indication for this group of patients other than arthroplasty.
However, based on the latest follow-up, there had been no need to perform arthrodesis for any of our patients.