Most cases of sporadic primary hyperparathyroidism present disturbances in a single parathyroid gland and the surgery of choice is adenomectomy. Conversely, hyperparathyroidism associated with multiple endocrine neoplasia type 1 (hyperparathyroidism/multiple endocrine neoplasia type 1) is an asynchronic, asymmetrical multiglandular disease and it is surgically approached by either subtotal parathyroidectomy or total parathyroidectomy followed by parathyroid auto-implant to the forearm. In skilful hands, the efficacy of both approaches is similar and both should be complemented by prophylactic thymectomy.
In a single academic center, 83 cases of hyperparathyroidism/multiple endocrine neoplasia type 1 were operated on from 1987 to 2010 and our first surgical choice was total parathyroidectomy followed by parathyroid auto-implant to the non-dominant forearm and, since 1997, associated transcervical thymectomy to prevent thymic carcinoid. Overall, 40% of patients were given calcium replacement (mean intake 1.6 g/day) during the first months after surgery, and this fell to 28% in patients with longer follow-up. These findings indicate that several months may be needed in order to achieve a proper secretion by the parathyroid auto-implant. Hyperparathyroidism recurrence was observed in up to 15% of cases several years after the initial surgery. Thus, long-term follow-up is recommended for such cases. We conclude that, despite a tendency to subtotal parathyroidectomy worldwide, total parathyroidectomy followed by parathyroid auto-implant is a valid surgical option to treat hyperparathyroidism/multiple endocrine neoplasia type 1. Larger comparative systematic studies are needed to define the best surgical approach to hyperparathyroidism/multiple endocrine neoplasia type 1.
Primary hyperparathyroidism (HPT) is highly prevalent in patients with multiple endocrine neoplasia type 1 (MEN1), and its penetrance is almost complete by the age of 40 years (1–7). HPT associated with MEN1 (HPT/MEN1) is an asynchronic, asymmetric multiglandular and multifocal disorder; the vast majority of cases are benign tumors and represented by parathyroid hyperplasia or adenoma (8); it occurs equally in males and females, and it frequently occurs at ages under 30 years (1),(2). Despite relatively mild elevations in serum parathormone (PTH) and total/ionized calcium usually seen in HPT/MEN1, there have been recent reports of early onset, and progressive, frequent, extensive and severe bone and renal complications (7),(9)
In recent years, routine genetic screening performed in at-risk family members of index MEN1 cases has significantly increased the recognition rate of young asymptomatic patients presenting at early metabolic stages of HPT in our and other institutions (10),(11). Furthermore, in recent decades, the clinical picture of sporadic or familial HPT has changed dramatically and most cases are more frequently recognized and diagnosed early, at asymptomatic stages (12),(13).
Medical non-surgical strategiesThe medical treatment of HPT associated with MEN1 is still under investigation. The experience with cinacalcet in HPT is limited to few cases, and no long-term follow-ups of disease end-points are available, despite short-term (up to 24 weeks) reductions of calcium and PTH (14–16).
Also, the use of percutaneous ethanol injection in cases of HPT recurrence after subtotal parathyroidectomy in HPT/MEN1 patients resulted in short-term eucalcemia. However, hypercalcemia recurred in 90% of cases after 32 months of therapy (17).
Furthermore, high-intensity focused ultrasound applied to sporadic, uniglandular HPT is under investigation, although temporary palsy of the recurrent laryngeal nerve in one out of four cases has been reported. Recovery was noted only 40 days after therapy (18), and the role of high-intensity focused ultrasound in multiglandular parathyroid disease is yet to be defined.
Long-term annual clinical follow-up has been recommended for selected sporadic cases of HPT, because bone mineral density may remain stable up to 10 years after diagnosis (19),(20). To date, it is not clear whether this recommendation can be extended to HPT/MEN1.
Surgical treatmentSurgery is the classic therapy for primary HPT in MEN1. However, the criteria to indicate parathyroidectomy in these cases remain under debate. The International Consortium/National Institutes of Health Consensus on MENs (1) recommended that indications for parathyroidectomy in MEN1 should follow the same criteria used for sporadic asymptomatic primary HPT (21),(22).
Most HPT/MEN1 patients are younger than 50 years at diagnosis, and thus fulfill the indication for parathyroid surgery based solely on this criterion. However, it may not be easy to convince an asymptomatic patient that he/she will benefit from an operation that can be considered palliative, as recurrence rates are usually high (23). In some young asymptomatic cases, the treatment may be perceived as worse than the disease itself (24).
Surgery in HPT/MEN1The surgical treatment of HPT/MEN1 is a challenge to the surgeon for several reasons. First, in the vast majority of cases, HPT/MEN1 is a multiglandular disease that usually occurs asymmetrically and asynchronically. Second, the frequency of supernumerary parathyroid glands is considerable. Furthermore, the surgeon is frequently confronted with parathyroid glands with macroscopic features resembling normal characteristics and he/she must decide how much tissue should be taken, evaluating the risk for permanent hypoparathyroidism versus disease persistence or early recurrence. One parathyroid gland may appear normal macroscopically, but may cause persistent hypercalcemia (24). Finally, although questionable as a 100% effective preventive strategy for thymic carcinoid tumors (25),(26), transcervical thymectomy has been recommended to be carried out during parathyroidectomy in HPT/MEN1 cases (27).
Presurgical diagnosis of MEN1As the first manifestation of MEN1 is usually HPT, and was found to increase >70% in one of our series (28), clinicians and surgeons must be strictly committed to making or ruling out a diagnosis of MEN1 before neck exploration in each patient with apparently sporadic HPT. An adequate preoperative diagnosis may help the surgeon to choose the best surgical option (24),(29),(30). It is well documented that measurement of intraoperative PTH may fail in patients undergoing parathyroidectomy for whom MEN1 is not suspected (31). Moreover, early diagnosis of MEN1 is critical to the adequate management of other MEN1-related tumors that have a clinical impact (3). In this context, mutation analysis of the MEN1 gene in apparently sporadic cases of HPT in which the patient is younger than 30 years of age may be helpful in the surgical management of HPT (1).
Genetic testing is crucial to confirm the familial character of HPT disease within clinically affected family members identified in MEN1 kindreds genetically characterized by a MEN1 germline mutation. Although rare, relatives presenting primary HPT but not harboring a germline MEN1 mutation have been reported. According to MEN1 clinical criteria, these patients would have been diagnosed as a MEN1 affected case (1). However, they are classified as sporadic HPT cases and should be surgically treated accordingly. Such cases represent MEN1 phenocopies, and do not need further surveillance for MEN1-related neoplasias.
Parathyroid hyperplasia or adenoma accounts for the vast majority of HPT cases in MEN1, as carcinoma seems to be an extremely rare event in this condition (32). The prevalence of parathyroid carcinomas in MEN1 tends to be much lower than in sporadic cases of HPT (33). Accordingly, we have seen no cases of parathyroid carcinoma in our HPT/MEN1 series, compared with higher frequencies observed in our sporadic HPT cases, in which we observed a 1.8–6.1% frequency of parathyroid carcinoma (34),(35).
What is the best surgical approach to HPT in MEN1?The best surgical approach to HPT in MEN1 is under debate, and includes resection of tissues other than parathyroid glands themselves.
Preventive thymectomyPresently, preventive thymectomy is highly recommended to be performed during either subtotal or total parathyroidectomy in HPT/MEN1 patients.
Since its proposal in 1997 (36), there is a general agreement that transcervical thymectomy should be performed during parathyroidectomy in all MEN1 cases, in order to: (a) detect supernumerary parathyroid glands, (b) prevent thymic carcinoids (occurrence in MEN1 ranges from 2.6% (37) to 8% (38), and (c) to disclose intrathymic parathyroid tissue when less than four parathyroid glands are identified during neck exploration (39). It has been estimated that transcervical thymectomy usually excises only 30–40% of the thymus (39). Consequently, thymic carcinoids have developed in a few cases, even after preventive transcervical resection, and this has caused its value to be questioned (25).
Accordingly, we have adopted routine transcervical thymectomy during parathyroid intervention in HPT/MEN1 cases since 1997. To date, no thymic carcinoid has been detected in the thymic specimens, and none of our patients has developed thymic carcinoid after this procedure. However, before 1997, in a specific HPT/MEN1 patient submitted to parathyroidectomy not associated with transcervical thymectomy, a thymic carcinoid with metastases was documented (27). Absence of thymic carcinoid with metastases in prophylactic thymectomy specimens has been reported in large series by others (30),(39).
Subtotal versus total parathyroidectomyRegarding the metabolic control of the HPT in MEN1, in the past many groups have favored more aggressive strategies, such as total parathyroidectomy followed by immediate parathyroid autotransplantation (40–43). However, in the last 20 years, several authors have advocated subtotal parathyroidectomy as the most suitable strategy in HPT/MEN1 cases (39),(44–47). Currently, only a few authors recommend total parathyroidectomy with autotransplantation (30),(48–50). In fact, for many years, it was claimed that only a prospective randomized trial would help to answer this issue; however, as far as we know, no such study has been published to date.
Data on this topic vary according to the group, but subtotal resection seems to be associated with a lesser risk of hypoparathyroidism. In 57 HPT/MEN1 cases, 34 were subjected to subtotal parathyroidectomy and 23 to total parathyroidectomy and autotransplantation. Rates of HPT persistency or recurrence were higher in the first group, while post-surgical hypoparathyroidism was more prevalent in the second group (51). In a large case series comprising 92 HPT/MEN1 patients treated over a period of 42 years, the 10-year actual recurrence-free interval data were 49% for subtotal parathyroidectomy and 84% for total parathyroidectomy and autotransplantation (47). In that series, post-surgical hypoparathyroidism rates were 26% for subtotal parathyroidectomy and 46% for total parathyroidectomy, but no significant difference was documented (p = 0.18). Notwithstanding, it was concluded that the high incidence of severe hypoparathyroidism after total parathyroidectomy with autotransplantation favored subtotal resection as the procedure of choice at the initial operation. It is worthwhile noting that a limited number of cases (n = 16) underwent total parathyroidectomy and parathyroid autotransplantation in that study (47). However, in another recent HPT/MEN1 series (n = 47), patients submitted to total parathyroidectomy and immediate autotransplantation presented with 22% postsurgical permanent hypoparathyroidism, whereas this rate was 45% in cases submitted to subtotal parathyroidectomy (30).
The rate of permanent hypoparathyroidism may be different in patients undergoing a first cervical exploration or a secondary cervical surgery. Thus, Tonelli et al. observed hypoparathyroidism in 10 out of 45 patients (22%) after the first surgery and in three out of six patients (50%) after a second cervical operation (48). Also, the rate of postsurgical hypoparathyroidism may be affected by the time of follow–up of the patient. Accordingly, there are reports of cryopreserved autografted parathyroid tissues achieving adequate PTH secretion only 2–4 years after implantation (45).
A recent meta-analysis suggested that subtotal parathyroidectomy is superior to total parathyroidectomy with immediate autotransplantation (52). Conversely, other authors favor a more aggressive initial operation (50),(53). In this context, it has been claimed that further high-quality evidence for the best surgical approach for HPT in MEN1 is lacking.
Experience from a single academic centerIn our experience, surgical treatment of HPT in MEN1 is a highly complex procedure, and the medical residents in our institution have been trained intensively in this technique (54),(55). Despite improvements in imaging techniques and intraoperative PTH sampling, the skillfulness of the surgeon is crucial. Therefore, parathyroidectomy in MEN1 patients is usually performed to a better standard in specialized tertiary academic centers where medical personnel and residents are highly trained (55),(56). Moreover, it is also important that MEN1 patients can be followed-up in specialized outpatient services in order to receive support for both oncological and end-organ diseases (43),(45),(47),(48),(51),(57–59).
Case seriesFrom 1987 to August, 2011, 83 HPT/MEN1 patients were submitted to 99 parathyroid interventions at the Hospital das Clínicas, University of São Paulo School of Medicine. There were 43 females and 40 males and the age at the parathyroid surgery varied from 17 to 74 years old (mean, 40.8 years). No difference in age distribution according to gender was noticed, as shown in Figure 1. Almost 75% of the patients were younger than 50 years of age and this finding may be related to the criteria used to indicate parathyroidectomy for these patients. In this HPT/MEN1 series, no child carrying the MEN1 gene had an indication for parathyroidectomy, although young HPT cases have been operated on in our group for other reasons, such as neonatal HPT (60).
Figure 2 shows that there has been an increasing number of HPT/MEN1 patients in recent years, most probably due to the active clinical and biochemical search for MEN1 diagnosis, as well as to the routine familial genetic MEN1 screening procedure performed by our group (3),(6),(7),(10),(11),(28),(61). In a recent study, HPT/MEN1 accounted for 17% of all cases undergoing parathyroidectomy at our institution (62).
Seventy-five out of the 83 cases of HPT/MEN1 (90.4%) had their initial operation at our institution between 1987 and 2011. Of the other eight cases, two underwent parathyroidectomy in our institution before 1987 and data from their first operation are unavailable. Surgeons initially involved in treating these two HPT/MEN1 cases might have been unaware of MEN1 at the time, excising only enlarged parathyroid glands. The remaining six cases underwent parathyroidectomy in other institutions, and their previous medical records were not available (Figures 3 and 4).
We had a reoperative rate due to HPT persistence of 8.0% (6/75) and an HPT recurrence rate of 6.75% (5/75), including all cases. However, taking into account only those patients with more than 5 years of follow-up (i.e., patients operated on up to 2006), the gross recurrence rate was 10.6% (5/47). This latter rate may in fact be slightly higher because a longer period of follow-up could not be performed in a few cases.
Total parathyroidectomy and autograftThe standard initial operation for HPT/MEN1 cases at our institution has been total parathyroidectomy followed by immediate parathyroid autograft to the non-dominant forearm, associated with transcervical thymectomy. Of note, although other groups have abandoned cryopreservation of parathyroid fragments because of the good results obtained with subtotal parathyroidectomy (46), we continue to advise cryopreservation whenever this procedure is possible. Parathyroid cryopreservation may have some limiting factors (63), but it is recommended when available, irrespective of the type of parathyroid surgery, since subtotal resection involves also a significant risk of permanent hypoparathyroidism (24),(30). Our experience with long-term cryopreserved tissue in secondary HPT (64) is similar to that reported by others in MEN1/HPT (30).
Initially, parathyroid autografts consisted of 20 fragments (each fragment was approximately 2×1 mm) that were transplanted in individual pockets. Presently, based in our experience in secondary HPT, 30 parathyroid gland fragments are usually implanted in a single pocket (65).
Intra-operative PTHIntra-operative parathyroid hormone (ioPTH) measurements have been obtained in more recent cases, although in our protocol all glands should be searched and excised irrespective of their macroscopic appearance. In our experience, ioPTH in HPT/MEN1 cases has presented some limitations. Indeed, preoperative diagnosis of MEN1 is much more informative to the surgeon than imaging studies or ioPTH. Thus, it can inform: (a) whether additional high hyperfunctional parathyroid tissue was left behind (which has not happened yet in our group); or (b) whether the exploration can be finished, despite the fact that fewer than four glands have been identified after an extensive search.
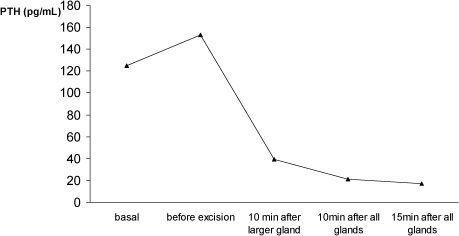
For academic purposes, we usually measure PTH at the following times: at the induction of anesthesia (basal), after identification of all parathyroid tissue (pre-excision), 10 min after the resection of the largest parathyroid gland, and again 10 min and 15 min after the excision of the remaining parathyroid tissue and thymus. In some circumstances, a decrease >50% of ioPTH has been observed after the excision of the largest parathyroid gland (Figure 5). This finding has been described previously (66), and may explain failures of ioPTH in the surgical management of HPT/MEN1 patients (31).
A marked decrease of intra-operative parathyroid hormone (ioPTH) after excision of the largest parathyroid gland only, in a case of hyperparathyroidism/multiple endocrine neoplasia type 1. Persistence or early hyperparathyroidism recurrence may occur if surgery is guided solely by ioPTH.
Fourteen out of the 75 HPT patients (18.7%) were reoperated in a total number of 16 reoperative procedures (Figure 3). Not all neck reoperations were related to HPT. Two consisted of total thyroidectomy and neck dissection for associated metastatic papillary thyroid carcinoma. In five cases, the parathyroid autograft at the forearm was excised due to recurrent HPT. One patient with non-functioning tumors was operated on due to goiter, and recurrence occurred later (see details of this case below). In five cases (6.7%), fewer than four glands could be initially identified at the first operation, and early HPT recurrence or persistence was observed: two retropharyngeal right superior parathyroid glands (one patient with right thyroid lobe agenesia), one intrathyroidal gland, one superior gland, and one located at the aortic arch in medium mediastinum and excised by thoracoscopy. Two further cases presented with late HPT recurrence due supernumerary parathyroid glands. One was located at the cervical region and the other at the mediastinum and, in this latter case, total thymectomy was performed by sternotomy. A rate as high as 33% for supernumerary glands has been reported in MEN1/HPT cases, including intrathyroidal supernumerary glands in 2.5% of patients (8). In our current experience, no patient with MEN1/HPT has presented a supernumerary intrathyroidal gland; however, it has been observed in some patients with renal HPT at our center (67). Our rate of intrathymic supernumerary glands was 4.9% (unpublished data). This rate is rather inferior to the rate of almost 30% reported by others (8). However, in a large series of routine bilateral cervical thymectomy in renal HPT, the frequency of supernumerary thymic parathyroids was 6.5% (68). A similar rate of 6% has been described in MEN1/HPT (39).
Of note, two specific cases were called our attention, and they are commented on below.
Non-functional tumor progressionThe first case of non-functional tumor progression was a female patient who was initially submitted to cervical surgery in 1993 and presented MEN1-related tumors: a non-functioning pituitary adenoma, multiple pancreatic endocrine tumors, as well as a goiter. No calcium abnormality was present at that time. During the partial thyroidectomy (lobectomy), an enlarged parathyroid was excised, although total parathyroidectomy was not performed at that time. She had no evidence of HPT until 13 years after parathyroid adenomectomy, when HPT ensued and she was subjected to reoperation. This case illustrates that hyperparathyroidism may ensue many years after an apparent non-functional enlargement of the parathyroid gland.
Relative of a MEN1 patient, with HPT due to a phenocopyAnother case, not included in the present series, is a person with HPT who was a relative of a MEN1 patient. This case came to the hospital with a clinical diagnosis of HPT/MEN1. However, after sequencing all MEN1 and p27 exons and their boundaries, no germline mutations were found characterizing a phenocopy, as previously reported in this condition (69). Thus, the surgical choice for this specific patient was a single parathyroid resection, with resolution of HPT. The patient is still under observation, without any sign of recurrence five years after the operation.
Reoperations from other centersAs mentioned, six of our HPT/MEN1 cases were initially operated on in other centers. Two were previously subjected to total thyroidectomy due to papillary thyroid carcinoma; a simultaneous intra-operative single parathyroid adenoma was found by the first surgeon. The two reoperations involved resection of the three additional parathyroid glands, central neck dissection and thymectomy. The third patient had been subjected to an intentional subtotal parathyroidectomy due to HPT/MEN1 at his primary center seven years before. His remnant was excised and partially autografted.
Three other cases had been subjected previously to surgery due to “a parathyroid adenoma”; in these cases, excision of the remaining parathyroid glands was carried out, followed by parathyroid autografts and thymectomy in one of the patients. One of these patients had been previously subjected to two cervical surgical explorations in another center; however, HPT persisted due an undescended left inferior parathyroid gland located close to the submandibular gland. This residual gland was discovered after a careful review of sestamibi scintigraphy. A first quick view may be misinterpreted as a negative result in planar projection (Figure 6). We excised this remaining parathyroid gland and part of it was immediately auto-implanted to the non-dominant forearm.
Sestamibi scintigraphy after two previous neck interventions in a patient with hyperparathyroidism/multiple endocrine neoplasia type 1 who had been treated initially at another hospital. There was a focal radiopharmacological concentration close to the left submandibular gland due to an undescended left inferior parathyroid.
Papillary thyroid carcinoma was found in five out of 83 cases (6%). This frequency was similar to that observed in sporadic HPT cases (9%) and carcinomas incidentally found in compressive multinodular goiter (11%) treated at the same institution (70). In four out of five cases, pathological data were available: all cases had microcarcinomas, which were multicentric in two instances. Microscopic metastases were present in two cases, and one had unilateral neck lymph node metastasis. One of these patients had apparently been subjected to high-dose radiotherapy due to a pituitary tumor many years before the neck operation.
Recurrence and hypoparathyroidismRecently, we attempted to contact 71 out of the 85 patients operated on from 1987 to 2010 in our institution, and information of 45 was available. As a first approach, a compact questionnaire was given to these patients in order to update the information on post-surgical therapy with the calcium supplement. Ten out of the 45 patients had died because of neoplasias other than MEN1-related tumors (22.2%). This observation might serve to re-emphasize the importance of early MEN1 detection and treatment, with the aim of decreasing morbidity and mortality, with reference to MEN1-related tumors in MEN1 (3). Five out of the 35 remaining cases (14.3%) had recurrent HPT disease; 14 others (40.0%) required calcium and/or calcitriol replacement therapy; and the remaining 16 cases did not take either calcium or calcitriol (45.7%). It is worthwhile noting that in HPT/MEN1 cases calcium requirement rates are impacted by the time elapsed since the parathyroidectomy. In Figure 7, the percentages of patients requiring calcium supplements were obtained at different periods after parathyroid intervention. We found that the longer the follow-up, the lower the frequency of patients requiring calcium supplement. Accordingly, in one of our HPT/MEN1 series, parathyroid auto-implants took from 6 to 15 months to secrete sufficient amounts of PTH in order to lead to normal calcemia (58).
For each individual HPT/MEN1 patient, it is necessary to decide which is the best operation to achieve the ultimate goal of maintaining normocalcemia and avoiding both iatrogenic hypocalcemia and operative complications; and facilitating future surgery for recurrent disease (71,72).
In many cases, calcium/calcitriol supplemental therapy could be stopped 15 months after total parathyroidectomy followed by parathyroid auto-implant, but not in all patients (58). A question to be addressed is the amount of calcium supplement required for each case. In our patients taking calcium supplement for more than one year, the mean intake was 1.6 g/day (range, 0.5–3.0 g/day), and 50% were taking 1.5 g/day or less.
Our present observations are in accordance with others: parathyroid autografts may take long periods, sometimes up to seven years, to achieve adequate function, and PTH levels increase with time (23),(58).
Subtotal and total parathyroidectomy followed by immediate parathyroid autotransplantation are surgical approaches that are currently accepted to treat cases with HPT associated with MEN1. In our single academic center, total parathyroidectomy followed by parathyroid autotransplantation to the non-dominant forearm associated with preventive transcervical thymectomy has been the surgical approach of choice for cases of HPT/MEN1. This strategy has been successful in achieving low rates of HPT recurrence. The considerable number of calcium-dependent patients, who were mainly observed in the first nine months after operation, tended to decrease during long-term follow-up.
RAT is a recipient of FAPESP post-doctoral fellowships (2009/15386-6 and 11942/2009). SPAT is partially supported by a CNPq fellowship and a CNPq grant (401990/2010-9).
No potential conflict of interest was reported.
Montenegro FLM, Lourenço DM Jr, Nascimento Junior CP, Arap SS, Massoni Neto LM, D'Alessandro A, Toledo RA, Coutinho FL, Cordeiro AC, and Toledo SPA conceived the study and were responsible for the collection and analysis of data, the draft and critical review of the manuscript, and approval of the final version of the manuscript. Tavares MR, Brandão LG and Silva Filho GB conceived, drafted and critically reviewed the manuscript, and approved the final version of the manuscript.