Sleep disorders include a number of different processes, of which the most prevalent is the sleep apnea-hypopnea syndrome (SAHS).
Prevalence of SAHS has increased worldwide, and has a significant social and health impact because of the increased cardiometabolic risk attributed to obesity and the associated metabolic syndrome.
Material and methodsA cross-sectional epidemiological study of 1110 workers from public service companies in the Spanish Mediterranean area (Balearic Islands and Valencian Community) was conducted between January and December 2015. Cardiovascular risk was calculated using the Castelli, Kannel and TG/HDL indices, and prevalence of obesity using body mass index, waist circumference, waist-height ratio, and visceral fat. SAHS risk was assessed using the Stop-Bang questionnaire.
ResultsRisk of SAHS was low in 77% of patients and intermediate-high in 23% of patients. All obesity parameters showed a statistically significant association (p<0.001) with intermediate/high risk of SAHS. Obesity prevalence is higher the worse the quality of sleep. There was a statistically significant relationship between risk of SAHS and cardiovascular risk with the atherogenic indexes found.
ConclusionsTwenty-three percent of workers had intermediate/high SAHS risk. The results of this study support the relationship of SAHS with an increased CVR and with obesity parameters.
Further prospective studies in different productive sectors may be useful to confirm the results of this research.
Los trastornos durante el sueño engloban un conjunto de procesos diversos, de los que el más prevalente es el síndrome de apnea-hipopnea del sueño (SAHS).
La prevalencia del SAHS ha aumentado en todo el mundo, y tiene importante repercusión sociosanitaria por riesgo cardiometabólico aumentado atribuido a la obesidad y al síndrome metabólico asociado.
Material y métodoEstudio epidemiológico transversal en 1.110 trabajadores de empresas del sector servicios de la Administración Pública del área mediterránea española (Islas Baleares y Comunidad Valenciana), realizado entre enero a diciembre de 2015. Se calcula el riesgo cardiovascular con los índices de Castelli, Kannel y TG/HDL y la prevalencia de obesidad mediante el índice de masa corporal, perímetro de cintura, índice cintura-altura y grasa visceral. Se valora el riesgo de SAHS mediante el cuestionario Stop-Bang.
ResultadosEl 77% de los pacientes tienen un riesgo bajo de SAHS frente al 23% con riesgo intermedio-alto. Todos los parámetros de obesidad muestran asociación estadísticamente significativa (p valor < 0,001), con riesgo intermedio/alto de SAHS. Hay mayor prevalencia de obesidad cuanto peor es la calidad del sueño. Se observa relación estadísticamente significativa entre el riesgo de SAHS y el cardiovascular con los índices aterogénicos estudiados.
ConclusionesUn 23% de los trabajadores presentaban riesgo intermedio/alto de SAHS. Los resultados de este estudio apoyan la relación del SAHS con el incremento del RCV y con los parámetros de obesidad.
Estudios posteriores prospectivos en diversos sectores productivos pueden resultar de utilidad para confirmar los resultados obtenidos en este trabajo.
Sleep respiratory disorders encompass a number of conditions, the most prevalent of which is obstructive sleep apnea-hypopnea syndrome (OSAHS), with recurrent airway restriction episodes resulting from anatomical and functional changes in the upper respiratory tract that cause them to collapse. This causes decreased oxyhemoglobin saturation levels and micro-awakenings, non-restorative sleep, and excessive daytime sleepiness, as well as neuropsychiatric, respiratory, and cardiac disorders.1
OSAHS prevalence is very high, ranging from 3% to 6% in Spain.2 Current estimations vary depending on age and sex: 10% of moderate to severe cases in males aged 30–49 years; 17% in males aged 50–70 years; 3% in females aged 30–49 years and 9% in older females. These rates have increased 14–55% depending on the subgroup in the past two decades.3
Studies conducted in different age groups show that there are in Spain 1,500,000–2,500,000 patients with OSAHS, plus an unknown number of asymptomatic patients with risk factors and pathological apnea-hypopnea index. Only 25% of them are being treated, but this is a much greater proportion as compared to the 4%-6% of patients on treatment in previous years.4
The increased prevalence of OSAHS worldwide has a great social and health impact because it increases the cardiometabolic risk partly attributed to obesity and metabolic syndrome in affected patients.5
There are different questionnaires to assess OSAHS, including the Stop-Bang Questionnaire, which is considered to be the most effective, with a sensitivity of 93–100% and a specificity of 43%.6 Early detection, control and treatment of OSAHS are especially important because they reduce secondary conditions and save health resources form the silent or preclinical stage of the disease. Patients with OSAHS not diagnosed or treated consume two to three times more resources than the general population, and incur 50–100% higher healthcare costs.7,8
Obesity is a major cause of sleep disorders, while atherogenic complications deserve special mention among their consequences. Clinical manifestations of atherosclerosis do not usually appear until advanced age, but the atherogenic process starts earlier, and changes in lipoproteins are a determinant factor of the risk related to atherosclerosis and its complications. They must therefore be detected at an early stage based on atherogenic indices to be able to more precisely establish the individual risk.
CVD causes 43.5% of fatal work accidents. A total of 629 fatal work accidents occurred in 2015, of which 43.5% were the consequence of a myocardial infarction or stroke.9
This study was intended to assess cardiovascular risk using the atherogenic indices of Castelli and Kannel and the TG/HDL ratio, to classify obesity based on mass index (BMI), and to estimate prevalence of obesity based on waist circumference (WC), waist/height ratio (WHR), and visceral fat (VF) and its relation to risk of OSAHS as assessed using the Stop-Bang Questionnaire.
Subjects and methodsA cross-sectional epidemiological study on workers from service companies of the Spanish public administration located in the Mediterranean area (Balearic Islands and Valencian Community). Subjects were studied from January to December 2015 when they attended regular health check-ups. Participation was voluntary, informed consent was obtained, and safety and health committees of the companies were previously informed, as required by preventive regulations in Spain.10 A total of 1110 of the 4325 workers of the participating companies (25.6%) took part in the study.
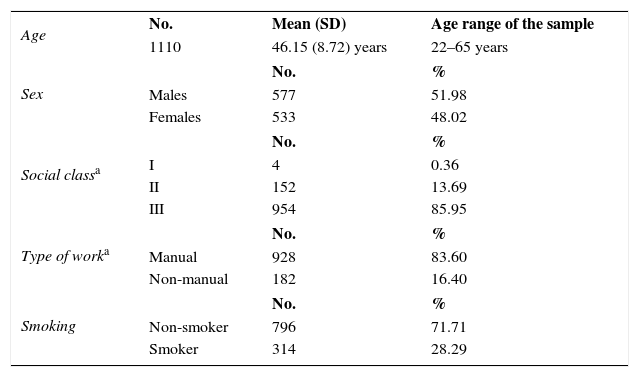
Table 1 shows the sociodemographic characteristics of the population sample.
Sociodemographic characteristics of study population.
Cardiovascular risk was estimated using atherogenic indices including different relations between cholesterol and triglyceride fractions, because of the proven relationship between cardiovascular risk and altered indices: the Castelli index (TC/HDL) considers low risk <5% in males and <4.5% in females, moderate risk 5%-9% in males and 4.5–7% in females, and high risk >9% in males and 7% in females; the Kannel index (LDL/HDL) considers low risk <3% and high risk ≥3%; and the TG/HDL ratio considers high risk values of 3% of higher.
Four BMI categories were used to classify and assess obesity11: low weight (BMI <18.5kg/m2); normal weight (BMI 18.5–24.9kg/m2); overweight (BMI 25–29.9kg/m2); and obesity (BMI ≥30kg/m2).
WC categories12: for males, normal <95cm, high risk 95–102cm, and very high risk >102cm. For females, normal <82cm, high risk 82–88cm, and very high risk >88cm. WHR categories13: WHR of risk ≥0.5, WHR with no risk <0.5. VF measured using a Tanita AB-140 Viscan body composition analyzer that considers normal values <12%.
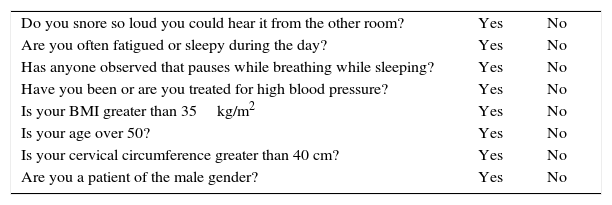
Risk of OSAHS was assessed using the validated Stop-Bang Questionnaire (Annex 1).
A statistical study including descriptive analysis, with absolute frequencies and percentages for categorical variables and mean and standard deviation for continuous variables. In the bivariate analysis, a Chi-square test χ2 or a Fisher's exact test was used to compare proportions. The significance level used was 0.05. Analysis was performed using R statistical software (version 3.3.2).
ResultsThe sample consisted of 1110 workers with a mean age of 46 years, 577 males and 533 females, most of them blue collar workers (83.60%) and belonging to social class III (85.95%). A great majority (71.71%) did not smoke.
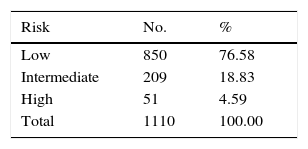
Results of the Stop-Bang Questionnaire showed that 77% of workers had low risk of OSAHS, while 23% had high/intermediate risk of OSAHS (Table 2). Only 1.62% of all participating subjects were on CPAP therapy.
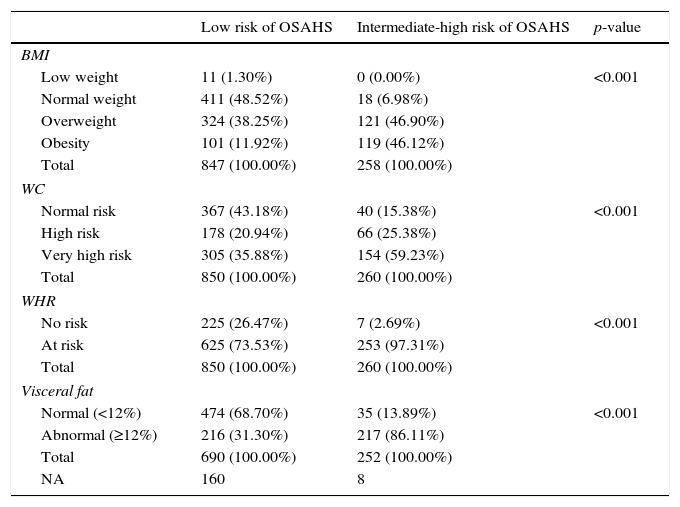
The relationship between obesity parameters (BMI, WC, WHR, and VF) and risk of OSAHS using the Stop-Bang Questionnaire showed for all parameters a statistically significant association (p<0.001), with higher proportions of subjects with high obesity risk in all its parameters and related to an intermediate-high risk of OSAHS, thus suggesting a significant relation between prevalence of obesity and risk of OSAHS detected (Table 3).
Descriptive statistics of prevalence of obesity (BMI, WC, WHR) by risk of OSAHS detected with the Stop-Bang Questionnaire.
| Low risk of OSAHS | Intermediate-high risk of OSAHS | p-value | |
|---|---|---|---|
| BMI | |||
| Low weight | 11 (1.30%) | 0 (0.00%) | <0.001 |
| Normal weight | 411 (48.52%) | 18 (6.98%) | |
| Overweight | 324 (38.25%) | 121 (46.90%) | |
| Obesity | 101 (11.92%) | 119 (46.12%) | |
| Total | 847 (100.00%) | 258 (100.00%) | |
| WC | |||
| Normal risk | 367 (43.18%) | 40 (15.38%) | <0.001 |
| High risk | 178 (20.94%) | 66 (25.38%) | |
| Very high risk | 305 (35.88%) | 154 (59.23%) | |
| Total | 850 (100.00%) | 260 (100.00%) | |
| WHR | |||
| No risk | 225 (26.47%) | 7 (2.69%) | <0.001 |
| At risk | 625 (73.53%) | 253 (97.31%) | |
| Total | 850 (100.00%) | 260 (100.00%) | |
| Visceral fat | |||
| Normal (<12%) | 474 (68.70%) | 35 (13.89%) | <0.001 |
| Abnormal (≥12%) | 216 (31.30%) | 217 (86.11%) | |
| Total | 690 (100.00%) | 252 (100.00%) | |
| NA | 160 | 8 | |
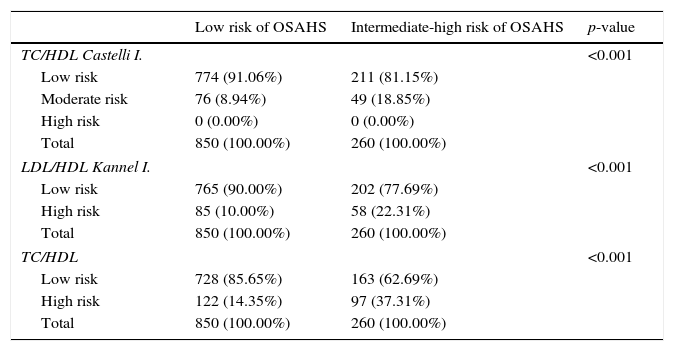
According to all atherogenic indices used, there was a statistically significant relationship between risk of OSAHS and CVR: TC/HDL, LDL/HDL, and TC/HDL, so that high CVR risk levels correspond to intermediate-high risk of OSAHS. The proportion of workers with low risk according to the Stop-Bang test was greater in workers with low CVR indices. Mean blood pressure values, both minimal and maximal, were higher in patients with intermediate-high risk, with statistically significant differences for both. Presence of MS and its relation to risk of OSAHS, as detected using the Stop-Bang Questionnaire, showed both variables to be statistically related to both IDF and ATP III criteria (Table 4).
Descriptive statistics of cardiovascular risk and risk of OSAHS-Stop-Bang.
| Low risk of OSAHS | Intermediate-high risk of OSAHS | p-value | |
|---|---|---|---|
| TC/HDL Castelli I. | <0.001 | ||
| Low risk | 774 (91.06%) | 211 (81.15%) | |
| Moderate risk | 76 (8.94%) | 49 (18.85%) | |
| High risk | 0 (0.00%) | 0 (0.00%) | |
| Total | 850 (100.00%) | 260 (100.00%) | |
| LDL/HDL Kannel I. | <0.001 | ||
| Low risk | 765 (90.00%) | 202 (77.69%) | |
| High risk | 85 (10.00%) | 58 (22.31%) | |
| Total | 850 (100.00%) | 260 (100.00%) | |
| TC/HDL | <0.001 | ||
| Low risk | 728 (85.65%) | 163 (62.69%) | |
| High risk | 122 (14.35%) | 97 (37.31%) | |
| Total | 850 (100.00%) | 260 (100.00%) | |
| Risk of OSAHS-Stop-Bang Questionnaire and metabolic syndrome (IDF and ATP III criteria) | ||||
|---|---|---|---|---|
| Metabolic syndrome | Low risk | Intermediate-high risk | p-value | |
| IDF criteria | Yes | 726 (85.41%) | 128 (49.23%) | <0.001 |
| No | 124 (14.59%) | 132 (50.77%) | ||
| ATP III criteria | Yes | 751 (88.35%) | 145 (55.77%) | <0.001 |
| No | 99 (11.65%) | 115 (44.23%) | ||
| Mean blood pressure values as related to risk of OSAHS-Stop-Bang test | ||||||||
|---|---|---|---|---|---|---|---|---|
| Risk of OSAHS | No. | Maximum blood pressure values | p-value | |||||
| Min. | P25 | Median | Mean | P75 | Max. | |||
| Low risk | 850 | 88 | 112 | 124 | 125 | 136 | 187 | <0.001 |
| Intermediate-high risk | 260 | 90 | 131.8 | 146 | 145.7 | 158 | 211 | |
| Risk of OSAHS | No. | Minimum blood pressure values | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Min. | P25 | Median | Mean | P75 | Max. | |||
| Low risk | 850 | 52 | 68 | 75 | 75.61 | 83 | 117 | <0.001 |
| Intermediate-high risk | 260 | 57 | 79.75 | 87 | 86.95 | 94 | 129 | |
Note: Percentage of the total in each of the risk groups.
Atherosclerosis is the leading cause of cardiovascular (CV) morbidity and mortality in the Western world. Detection and treatment of risk factors such as obesity, dyslipidemia, and diabetes mellitus decrease CV events, and preventive interventions at workplaces may improve the risk factor profile. They should therefore be implemented as widely as possible.14
Morbidity and mortality associated to CVD have exponentially increased in recent years in most countries. It is estimated that approximately 80% of deaths from CVD occur in people more exposed to risk factors, and especially in those with no access to effective and equitable health care (including early detection services, which should also cover the workplace).
No conclusive results are available because of the limitations of studies reporting preventive interventions, but there is evidence of the efficacy of interventions on blood pressure levels, body mass index, and waist circumference in high risk populations. However, larger studies with longer follow-up times are required to confirm whether multifactorial interventions result in reduction of CV events and mortality, which would be related to socioeconomic factors of the population.15
There is agreement in the health care significance and the costs of events resulting from atherosclerosis and the weight of CVR factors on their occurrence, and there is strong evidence showing that stroke prevention is feasible in practice and that there is an urgent need to expand primary prevention actions.16
The study on the global, regional, and national load of CVDs conducted from 1990 to 2015 shows that they continue to be among the main causes of loss of health in all regions of the world and their direct relationship to sociodemographic and economical conditions in recent years.
Special attention is paid to the relationship between sleep disturbances, particularly OSAHS, and CVR. Obstructive sleep apnea is independently associated to an increase in mortality from CVDs, especially myocardial infarction and stroke, both of them complications of atherosclerosis, and may accelerate their occurrence because it increases atherogenic risk factors and has direct preatherogenic effects such as systemic inflammation, oxidative stress, activation of vascular smooth cells, increased expression of adhesion molecules, monocyte/lymphocyte activation, increased lipid load in macrophages, and endothelial dysfunction.17 In the workplace, workers with OSAHS show increases in dyslipidemia18 which agrees with the results found in our study. This may contribute to a greater risk of cardiovascular events detected in workers with this sleep disturbance.19
Some authors specifically state that patients with OSAHS have higher rates of dyslipidemia, but only LDL-C has been independently associated to OSAHS.20 They therefore suggest adoption of new interpretative and predictive strategies to assess risk progression in the clinical course of OSAHS.21
Some epidemiological studies estimate that obesity increases the risk of CVD and metabolic disorders, particularly insulin resistance, all of them associated to presence of OSAHS and vascular morbidity. However, further clinical studies and controlled trials are required to determine the extent to which OSAHS is a risk factor for the occurrence of diabetes and its effect of glucose metabolism.22
Our study results support this relationship between obesity and OSAHS, considering BMI, WC, WHR, and visceral fat, variables which are in turn related to metabolic syndrome.
Combined occurrence of obesity, high blood pressure, insulin resistance, and dyslipidemia is associated to marked increases in CVR. Prevalence of metabolic syndrome in patients with obstructive sleep apnea is very high, and obesity is the main risk factor. In turn, OSAHS is considered to be the most common cause of secondary hypertension. Our study showed a significant relationship between moderate/high risk of OSAHS and presence of MS and elevated mean blood pressure levels. Some studies have shown OSAHS to be independently associated to insulin resistance.23
The results of this study show that 15%-20% of the population has moderate/severe risk of OSAHS which is not diagnosed or treated. Such data agree with those reported in other previously mentioned studies, such as the Peppard et al. study, and other reports stating that obstructive sleep apnea occurs in up to 25% of healthy individuals and is associated to intermittent hypoxia, oxidative stress, sympathetic activation, and inflammatory response. Obstructive sleep apnea is therefore considered an independent, modifiable risk factor for CVD that may induce or speed up progression of the process.24 The effect of treatment of OSAHS with CPAP on CVD has not been established yet. The results reported appear to show attenuation of the risk and cardioprotective effects,25 with reduction in the rates of myocardial infarction and stroke.26 In this regard, results of our study show that not all workers diagnosed with OSAHS are on CPAP therapy and, of those who are, not all are subject to regular monitoring and follow-up.
The Stop-Bang Questionnaire has been validated for detection of risk of OSAHS and has shown excellent sensitivity for screening patients at risk, being able to predict OSAHS severity.27 Its simple use makes it especially advisable in the workplace and in specific health surveillance protocols or health promotion campaigns.
One of the most controversial aspects may be that of effectiveness of other preventive screening measured using routine blood count parameters. Among these, only red blood cell distribution width may show the inverse consequences of comorbidities associated to OSAHS.28 Some authors suggest that platelet distribution may also be a marker of OSAHS severity.29 Both parameters were not considered in this study, but may be analyzed in subsequent studies.
Strengths of this study include its sample size, the fact that it was conducted in a work setting, and evaluation of CVR using different risk indices and obesity parameters such as WHR and WC, as well as visceral fat, a parameter rarely used because there are different perceptions on its specificity.
A study limitation is that its results cannot be extrapolated to the general population or the whole working population because it was conducted on a specific group, the public administration sector, and in a limited geographical area, the Mediterranean region.
The importance of this question has led groups of specialists to state that they should be familiar with symptoms and signs of OSAHS and the pathophysiology of the association of untreated sleep pathology and CVD, and that sleep disturbances should be ruled out in patients with CVD and should be considered as an important modifiable risk factor. Knowledge of this association is of paramount importance for public health and for primary and secondary prevention of cardiovascular events, and also helps provide patients with health education and treatment.30
Although evidence exists of a causal relationship between OSAHS and cardiovascular disorders, additional controlled intervention data supporting such relationship are needed. Many risk factors for OSAHS (age, male sex, and obesity) are also risk factors for CVD. In the work setting, neurocognitive consequences of OSAHS, such as daytime sleepiness, loss of alertness, memory deficit, decreased vigilance, impaired executive function, increased risk of traffic and work accidents, and decreased quality of life, are of special concern.31 Risk of cardiovascular events, currently considered as one of the main causes of work accidents, should be added to this list.
Our study results support the relationship of sleep disturbances, namely OSAHS, with increased CVR as estimated with the Castelli, Kannel and TG/HDL indices, and with obesity assessed using BMI, waist circumference, waist-height ratio, and visceral fat Further prospective studies conducted in various productive sectors may be of value to support the results found in this study.
Conflicts of interestThe authors state that they have no conflicts of interest.
| Do you snore so loud you could hear it from the other room? | Yes | No |
| Are you often fatigued or sleepy during the day? | Yes | No |
| Has anyone observed that pauses while breathing while sleeping? | Yes | No |
| Have you been or are you treated for high blood pressure? | Yes | No |
| Is your BMI greater than 35kg/m2 | Yes | No |
| Is your age over 50? | Yes | No |
| Is your cervical circumference greater than 40 cm? | Yes | No |
| Are you a patient of the male gender? | Yes | No |
Three or more affirmative answers indicate a risk of almost 50% of suffering from OSAS, whereas if the answers are 2 or less, the risk is almost zero.
• Low risk: when you answer Yes to 0–2 questions.
• Intermediate risk: when you answer Yes to 3–4 questions.
• High risk: when he answers Yes to 5–8 questions, or if he answered “yes” to 2 or more of the first 4 questions and is male; or if you answered “yes” to 2 or more of the first 4 questions and your BMI is more than 35kg/m2; or if you answered “yes” to 2 or more of the first 4 questions and the circumference of your neck is: (17″/43cm in men, 16″/41cm in women).
Source: Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, et al. Validation of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea among different populations: A systematic review and meta-analysis. PLoS One. 2015; 14;10(12):e0143697. doi:10.1371/journal.pone.0143697. eCollection 2015.
Please cite this article as: Vicente-Herrero MT, Capdevila García L, Bellido Cambrón MC, Ramírez Iñiguez de la Torre MV, Lladosa Marco S. Riesgo cardiovascular y obesidad en el síndrome de apnea del sueño valorado con el cuestionario Stop-Bang. Endocrinol Diabetes Nutr. 2017;64:544–551.