IgG4-related disease (IgG4-RD) is a multisystem immune-mediated entity that preferentially affects the pancreas, gallbladder, and bile ducts. It is an underdiagnosed disease that requires a high index of suspicion, especially in subclinical cases. Type 1 autoimmune pancreatitis (AIP) is the prototype of organ involvement in IgG4-RD. Typical clinical features of AIP-1 include obstructive jaundice, abdominal pain, and acute pancreatitis, although up to 15% of cases may have an indolent course1; it has a typical radiological appearance and the differential diagnosis is basically made with pancreatic cancer. Exceptionally diabetes mellitus (DM) may be the first or only manifestation of AIP-1.2 The association between AIP-1 and the development of DM was initially described by Tanaka et al. in the year 20003 and a prevalence of DM of 21%–70% has been described in patients with AIP-1.4,5
Clinical caseA 58-year-old man from Bolivia with a four-year history of type two DM treated with metformin monotherapy with good metabolic control (HbA1c <7%) and a right submandibulectomy for a Küttner tumour without follow-up or further study. He was referred to the endocrinology department due to a sudden deterioration in glycaemic control. On questioning, the patient reported only polyuria, polydipsia and weight loss of nine kilograms in the six weeks prior, with no associated gastrointestinal symptoms. Physical examination revealed bilateral parotid and left submandibular gland hypertrophy, as well as discrete bilateral exophthalmos. Capillary blood glucose at consultation was 339 mg/dl and HbA1c 14%, for which treatment was started with basal-bolus insulin. The pancreatic autoimmunity study was negative. The histopathological report of the submandibulectomy surgical specimen was reviewed, and it reported a dense lymphoplasmacytic infiltrate, storiform fibrosis, a proportion of IgG4+/IgG + cells >40%, and >10 IgG4+ plasma cells/high power field. The determination of serum immunoglobulins showed elevated values of total IgG (1950 mg/dl, normal range 700–1600 mg/dl) as well as of the IgG4 subclass (757 mg/dl, normal range 3−210 mg/dl). Computerised axial tomography (CT) showed multifocal involvement of the pancreas, preserving the opening of the pancreatic and bile ducts at the level of the pancreatic head (Fig. 1). Positron emission tomography (PET)-CT revealed a pathological increase in metabolic activity in the body and tail of the pancreas, with notable diffuse thickening of the parenchyma, as well as in the left submandibular gland, prostate, and axillary and mediastinal lymph nodes. (Fig. 2, A). A CT scan of the eye sockets revealed enlargement (pseudotumour) of both lacrimal glands. Chymotrypsin and faecal elastase levels were normal, so involvement of the exocrine pancreas was ruled out. The diagnosis of AIP-1 and therefore IgG4-RD was established. Combination therapy with prednisone (0.6 mg/kg body weight with gradual and progressive dose reduction) was started along with two doses of rituximab (1000 mg, separated by two weeks). The hyperglycaemia gradually subsided, which made it possible to substitute rapid insulin for metformin and reduce basal insulin, maintaining good glycaemic control (control HbA1c 5.6%). Four months after starting treatment, serum IgG4 decreased to 248 mg/dl and control FDG-PET showed a complete metabolic response in the left submandibular gland, axillary/mediastinal lymphadenopathy, and tail/body of the pancreas (Fig. 2, B). Other organs frequently affected by IgG4-RD, such as the lungs, kidneys, and retroperitoneum, were found to be unharmed in the initial and follow-up study using PET-CT.
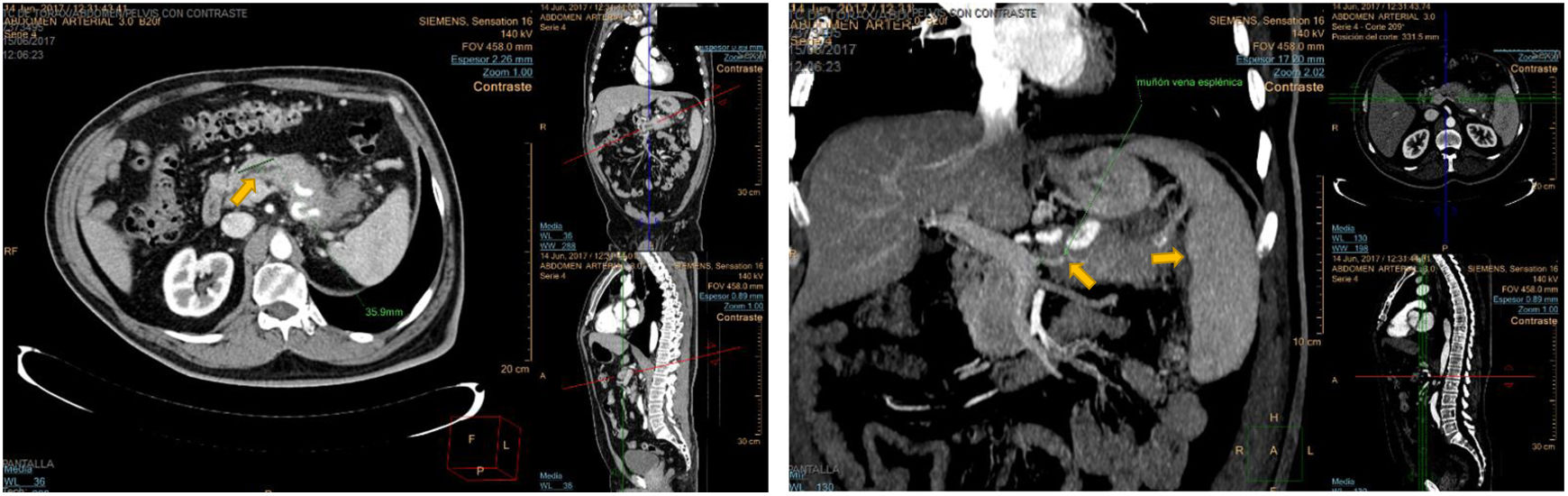
Simple and contrasted abdominal CT showing multifocal pancreatitis with subtotal visceral involvement. A portion of the pancreatic neck of about 3.5 cm is not thickened and shows through it a dilated and irregular pancreatic duct. Entrapment and occlusion of the splenic vein can be seen, diverting the venous flow through collaterals and homogeneous splenomegaly of 16 cm.
(A) Axial and coronal PET-CT images revealing involvement of multiple organs: left submandibular gland, axillary and mediastinal lymphadenopathy, pancreas, and prostate. (B) Control PET-CT images after two cycles of treatment with rituximab and prednisone demonstrated a complete metabolic response in all previously affected locations.
Although the evidence is limited (four cases of AIP-1 with pancreatic biopsy), it is known that DM associated with AIP-1 is caused by a reduction in beta-cell mass and the suppression of their function by cytokines present in the pancreatic microenvironment,6 in addition to a net decrease in insulin secretion. No correlation has been observed between serum IgG4 levels and the development of DM in patients with AIP-1.7 Corticosteroid therapy induces an improvement in glycaemic control in patients with DM secondary to AIP-1, mainly due to an increase in endogenous insulin secretion,8 and it is more likely in those cases in which DM is diagnosed concurrently with AIP-19 compared to cases with pre-existing DM, and is also related to the degree of pancreatic atrophy,10 remission of DM being less likely in cases with extensive pancreatic atrophy. A relationship has not been found between serum IgG4 levels and rates of remission or improvement of DM in patients with AIP-1 either.7
The clinical manifestations of IgG4-RD need to be understood in order for it to be included in the differential diagnosis of many common symptoms, as well as not to exclude the less common causes of sudden severe hyperglycaemia with no other apparent cause, so that morbidity associated with diagnostic procedures and unnecessary therapeutics can be avoided.
Please cite this article as: Males-Maldonado D, Mola Reyes L, Martín González A, Gómez Grande A, Guadalix Iglesias S. Diabetes mellitus secundaria a enfermedad relacionada con la IgG4. Endocrinol Diabetes Nutr. 2022;69:151–152.